
Immunology of
Cancer

Why Immunology?

The immune system’s influence on the
development of cancer can be seen in
immunocompromised patients.
a.
5% persons with congenital immunodeficiencies develop
cancer
(200 x rate)
b.
immunosuppresed transplant patients (rate 80 x)
c.
AIDS
lymphomas (activated B cells)
XLP + EBV - chronic infectious mononucleosis
or
- malignant lymphomas

So basically in healthy
individuals the immune
system recognizes tumor
cells as foreign and
destroy them before they
have a chance to multiply.

How does the immune
system recognize tumor
cells?

The immune system can distinguish
between normal and transformed
cells by:
• Tumor specific antigens (TSA)-present on
tumor cells, and not on normal cells.
• Tumor associated antigens (TAA)-present on
tumor cells and some normal cells.
•
40% melanomas
•
20% breast ca express
MAGE-1
•
30% lung small cell ca
Examples of tumor
antigens
Renal cell carcinoma 70% express
GP250
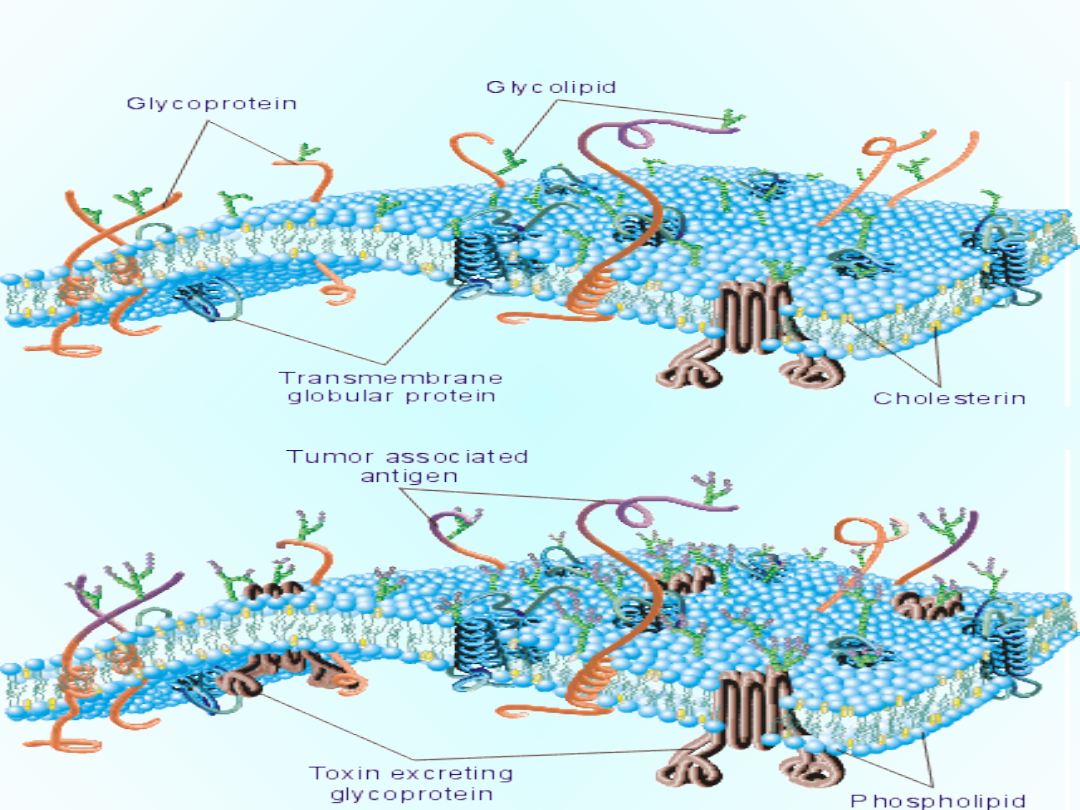
The membrane of the normal cells & cancer
cells
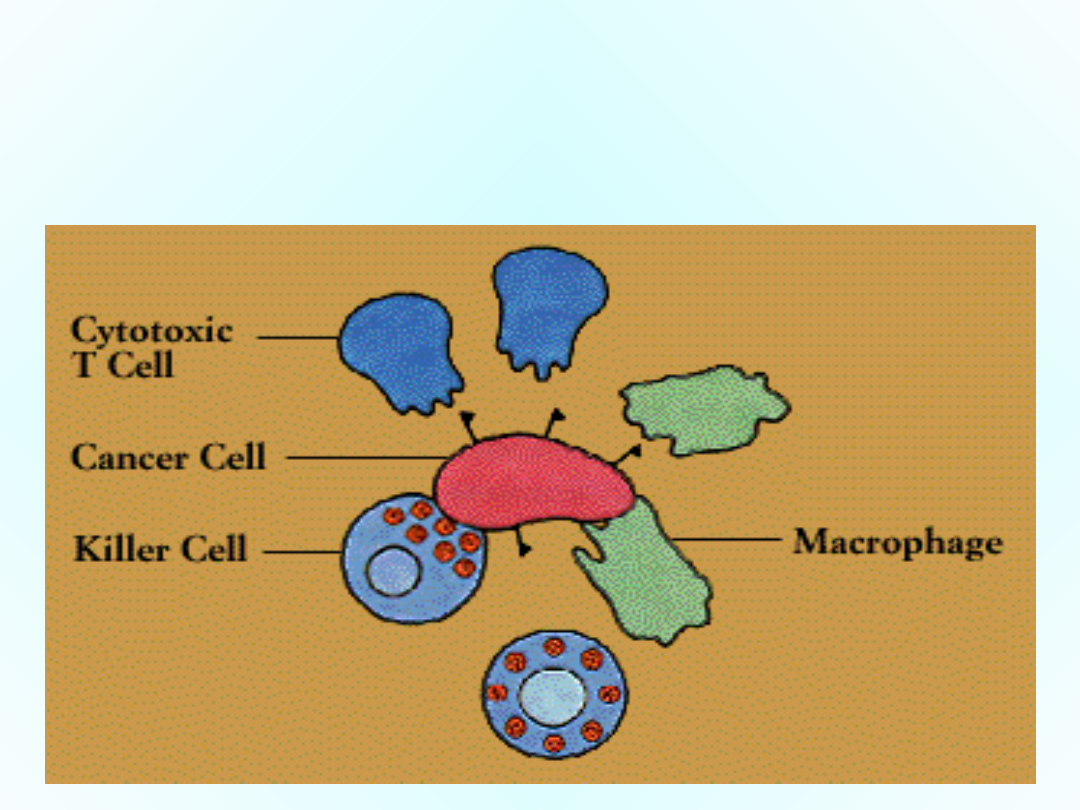
How the immune system “kill” the
cancer cell.
Cellular Effectors that Mediate Immunity
1.Cytotoxic T lymphocytes-protective role against
virus-associated neoplasms (EBV, HPV)
2.Natural killer cells (NK)-lymphocytes capable of
destroying tumor cells w/o prior sensitization - first
line of defense against tumors. After activation
with IL-2, NK lyse a variety of tumors (even if they
appear to be non-immunogenic to T cells.
T cells
complementary anti-tumor mechanisms
NK cells
Cellular Effectors that Mediate Immunity
3. Macrophages-activated exhibit selective
cytotoxicity against tumor cells.
T cells
NK cells
collaborate in anti-tumor reactivity
Macrophages
(e.g. INF- secreted by T and NK cells, activator of
macrophages). Kill by production of reactive
oxygen , or secretion of TNF-
4. Humoral mechanisms
activation of
complement
induction of
ADCC
(antibody-
dependent cell cytotoxicity):
by NK
cells
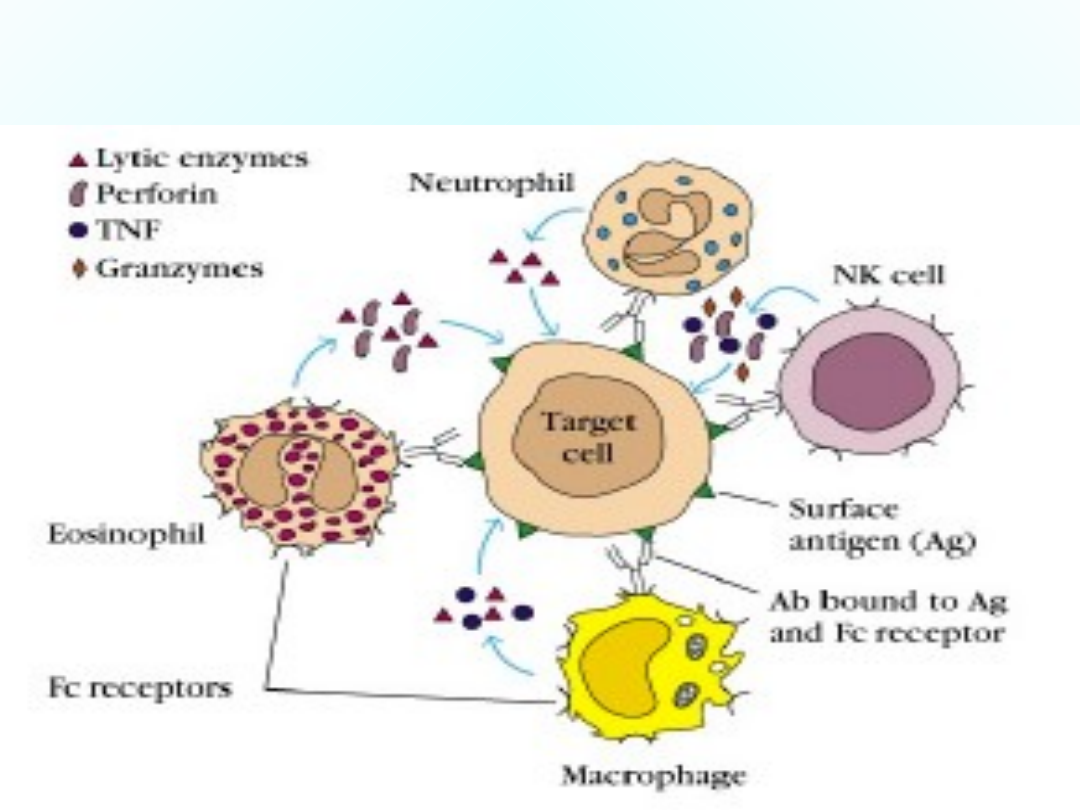
Antibody-dependent cellular
cytotoxicity (ADCC)

Tumor
cell
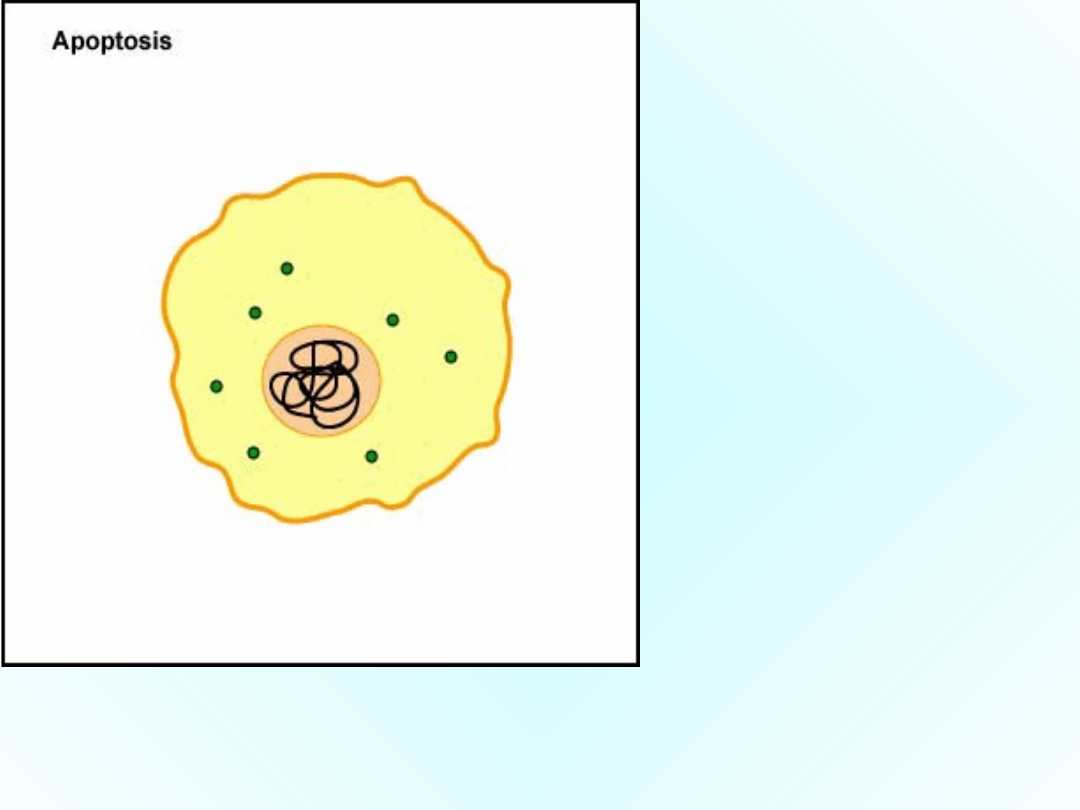
Granzymes pass through the pores and activate the
enzymes that lead to apoptosis of the infected cell by
means of destruction of its structural cytoskeleton
proteins and by chromosomal degradation. As a result,
the cell breaks into fragments that are subsequently
removed by phagocytes. Perforins can also sometimes
result in cell lysis.
The Fab portion of the
antibody binds to
epitopes on the
"foreign" cell. The NK
cell then binds to the
Fc portion of the
antibody. The NK cell is
then able to contact
the cell and release
pore-forming proteins
called perforins,
proteolytic enzymes
called granzymes, and
chemokines.
As a result, the cell breaks into fragments that are
subsequently removed by phagocytes. Perforins can also
sometimes result in cell lysis.
The NK cell releases
pore-forming proteins
called perforins,
proteolytic enzymes
called granzymes, and
chemokines.
Granzymes pass
through the pores and
activate the enzymes
that lead to apoptosis
of the infected cell by
means of destruction
of its structural
cytoskeleton proteins
and by chromosomal
degradation.

Possible Effector Mechanisms in Tumor
Immunity
Humoral
Opsonization and
phagocytosis
Complement-mediated lysis
Loss of cell adhesion
(antibody dependent)
Cell-Mediated
Cytotoxicity
T Cell
Antibody-dependent
cytotoxicity
NK
LAK (lymphokine-activated
killer) cells
Macrophages (macrophages
can be activated by
lymphokines)
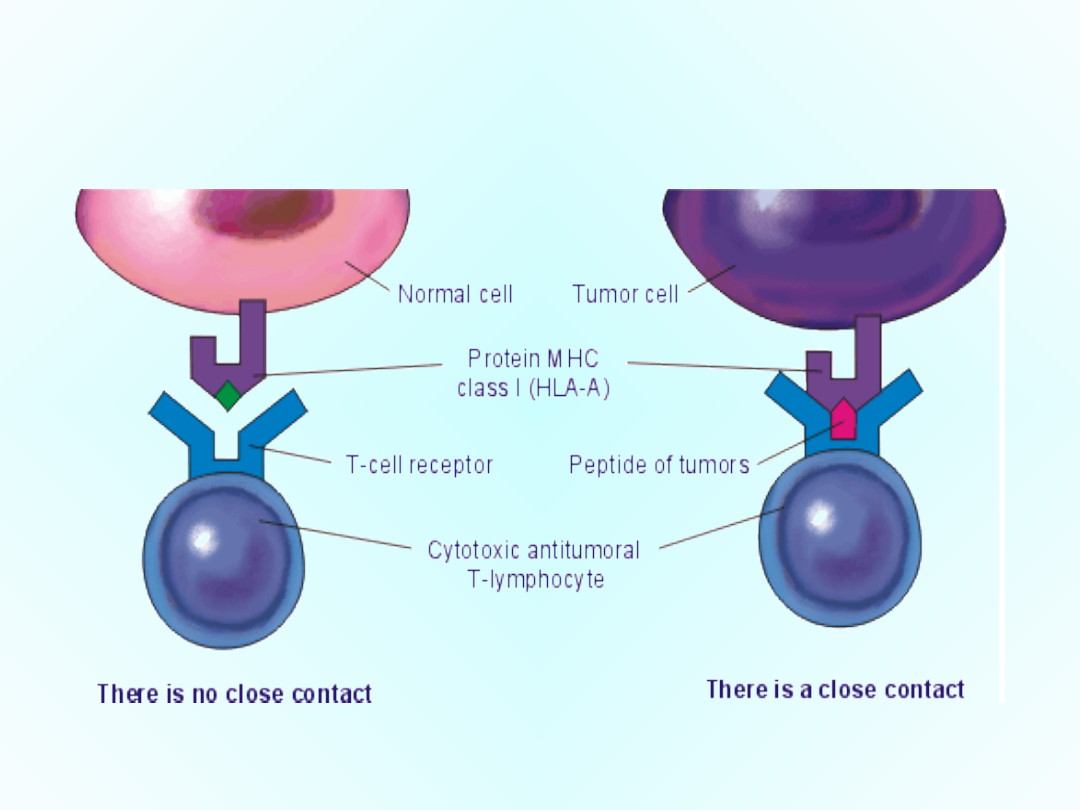
The antitumoral T-lymphocyte bind with the
tumoral cell
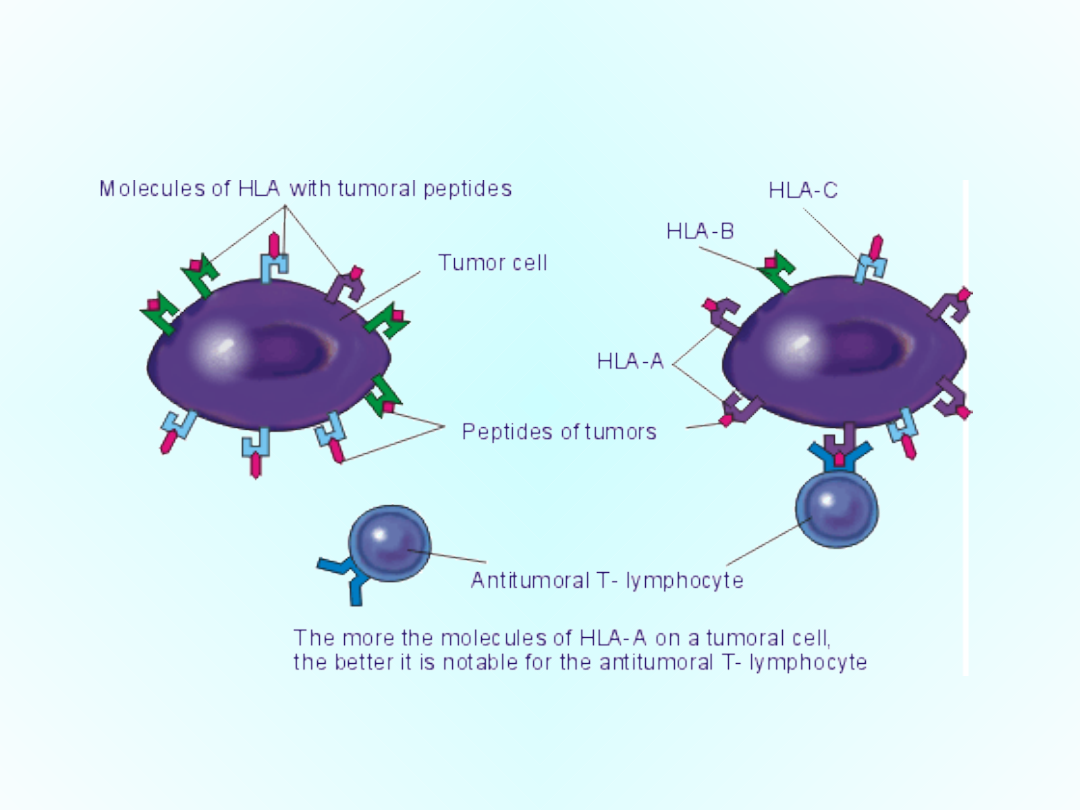
The search of tumor cells with a
help of the antitumoral T-
lumphocytes
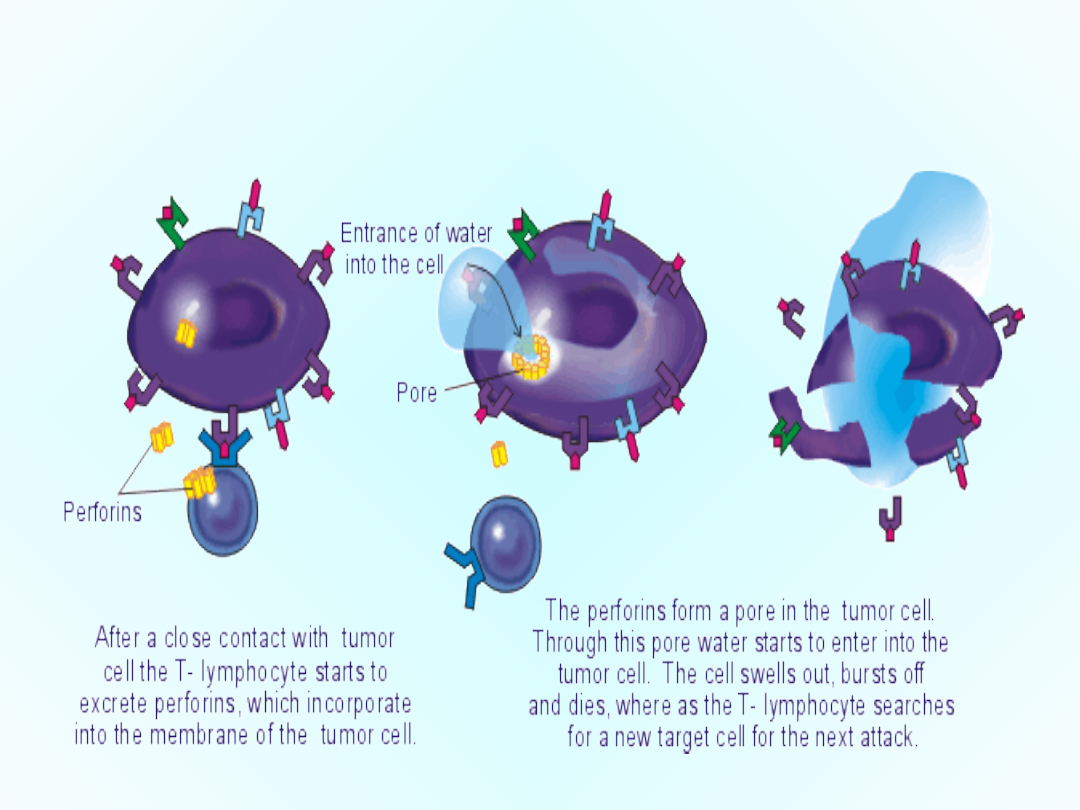
The destruction of tumor
cells by T-lymphocyte
HOW THE T CELL DESTROYS CANCER

If our immune system
can destroy tumor cells
then why do we have
cancer?

There is a selection for tumor cells that among other
things:
1. Avoid the immune response by being non-
immunogenic, selective outgrowth of antigen
negative variants.
2. Loss or reduced expression of HLA antigens.
2. Immunosupression, producing anti-inflamatory
cytokine such as TGF-1.
3. Induce apoptosis of immune cells (NK cells,
Cytotoxic T lymphocytes, Helper T lymphocytes)
4. No costimulation, no sensitization
Escape Mechanisms from Immuno
Surveillance
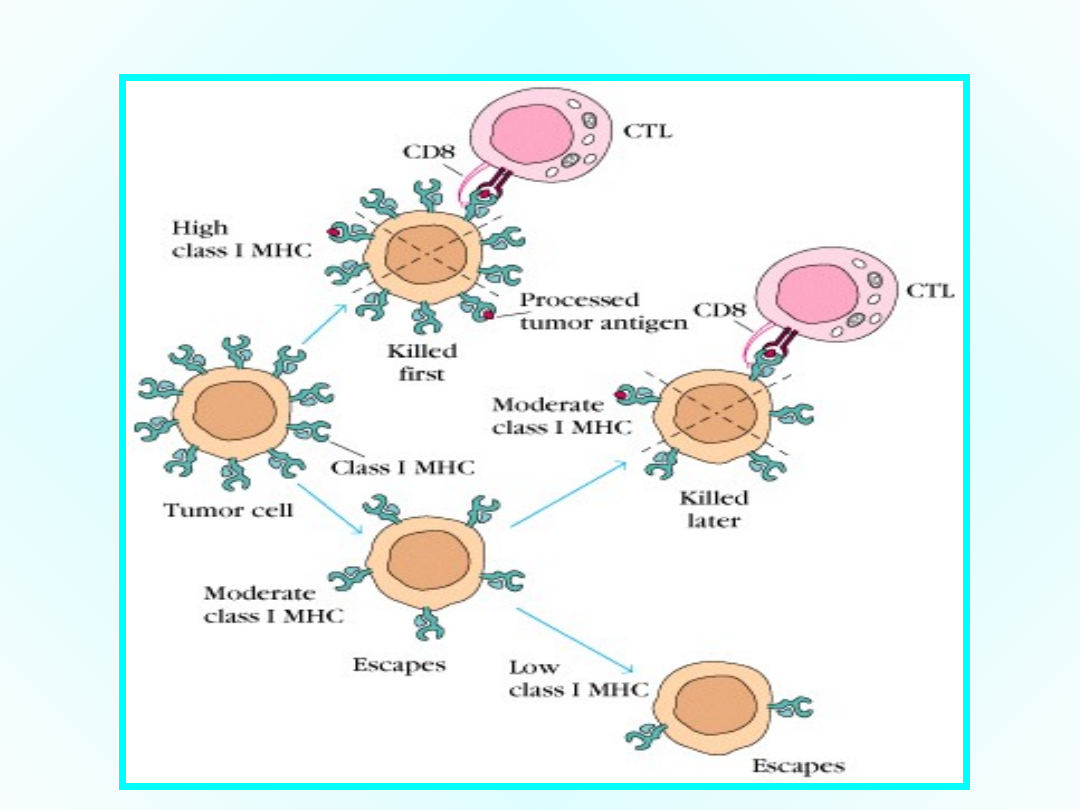
Tumor Evasion of Cytotoxic T lymphocytes (CTL) eg.
Tumor Evasion of Cytotoxic T lymphocytes (CTL) eg.
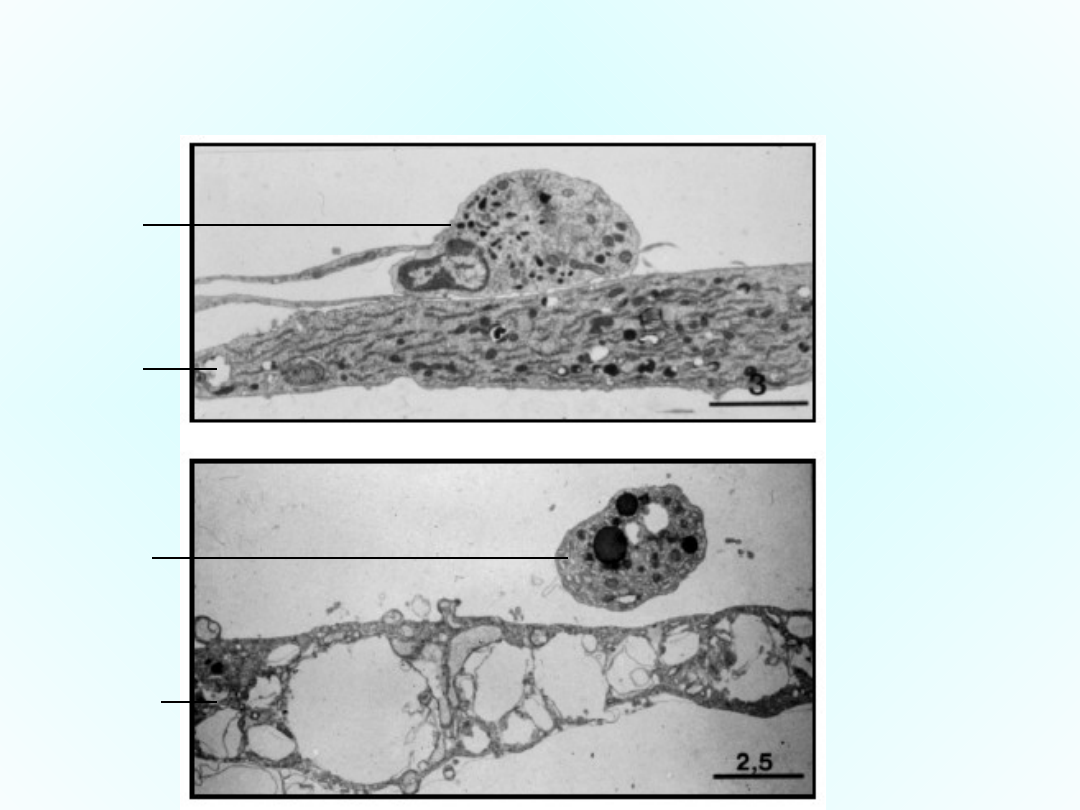
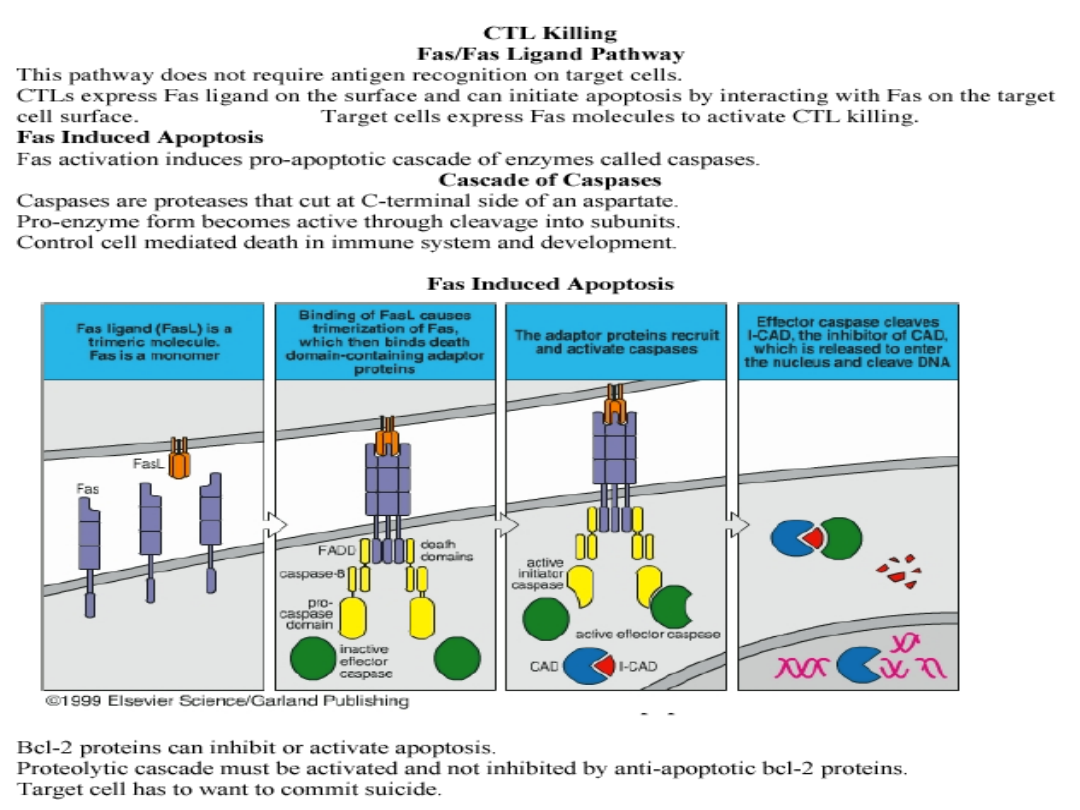
The Tumor cell can also induce apoptosis
(programmed cell death) of T lymphocytes.
5 min after
contact
45 min
after
contact
T cell
tumor
Apoptoti
c T cell
tumor
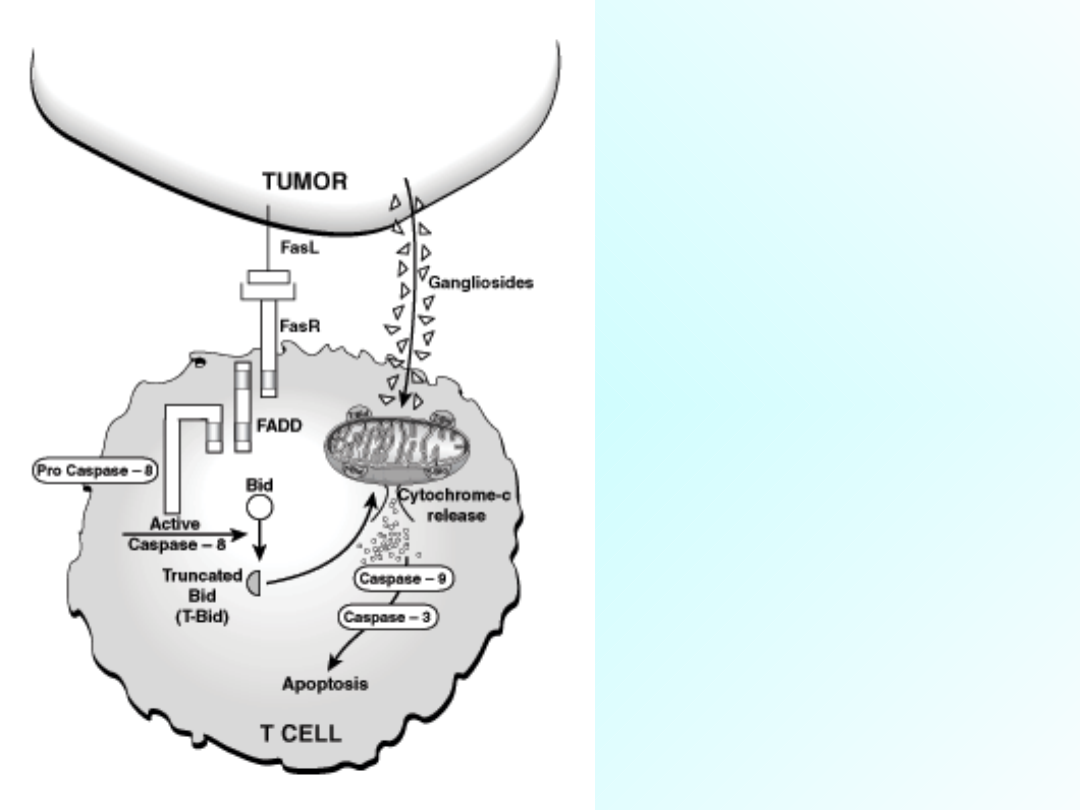
Tumor cells
can destroy T
cells by the
Fas/FasL (Fas
ligand)
pathway or
with the use
of
gangliosides.

So the Tumor cell can
avoid the immune system’s
response by “hiding”,
“pretending to be normal”,
or “killing” the immune
cells.

OK, so what now?
How do we make the
immune system recognize
and destroy the tumor
cells?
The Challenges of The immune
system
1. How to identify and specifically
respond to millions of different antigens
2. How to distinguish between foreign
(tumor) and self antigens
3. How to optimally and appropriately
respond to tumors
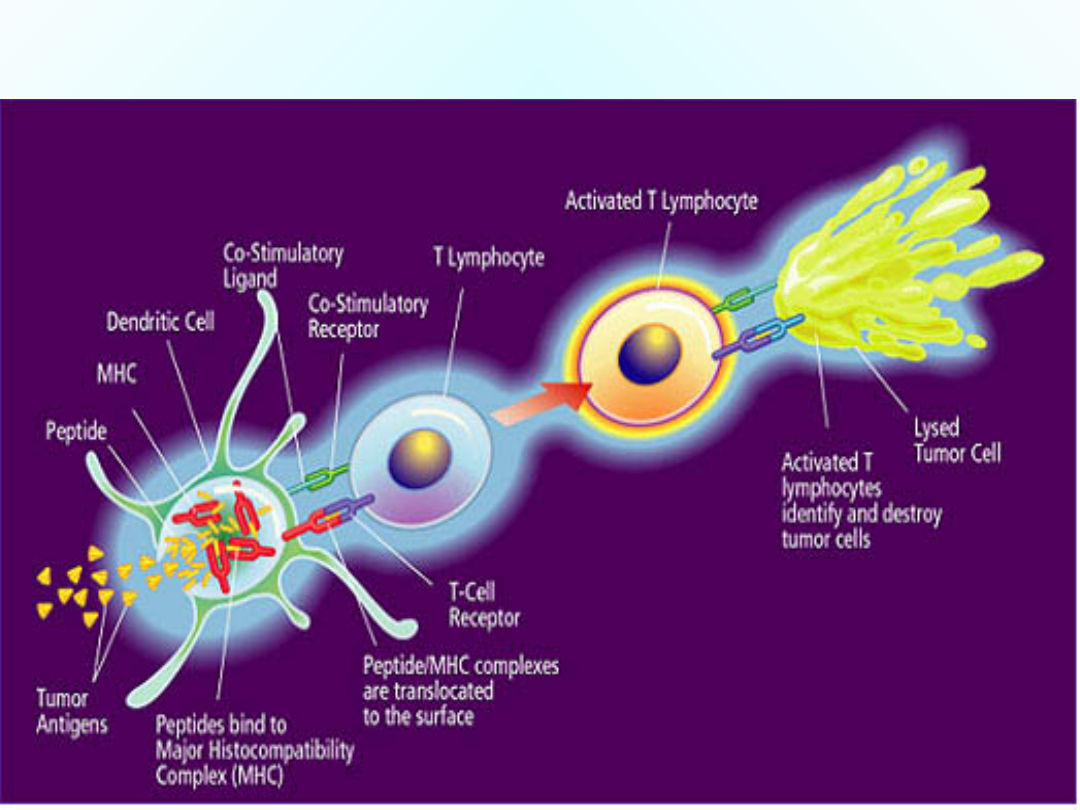
The players, or the cells of the
immune system
• Lymphocytes (B and T cells): Determining
the specificity of the immune response
• Monocytes/Macrophages and Dendritic
cells (Antigen presenting cells - APC):
presentation of antigen on the major
histocompatability complex (MHC).
• Natural Killers
• Mast cells and Basophils

• CD4
+
T cells- T helper cells
CD4 interacts with MHC II that process
Ag from the environment
• CD8
+
T cells- cytotoxic cells
CD8 interacts with MHC I that presents
intracellular antigens.

The immune response takes
place in specific tissues
• The cells of the immune system are
found in peripheral organized tissues:
• Recirculating in the blood and lymph
• Lymph nodes
• Spleens
It is within these tissues that the immune
response occur

The immune response
1. Humoral: B-cells/Th2
Production of Antibodies that
specifically bind antigens. Initiates the
clearance of the antigen by phagocytes
and the complement system.
2. Cellular response: T-cells/Th1
Specialized cells that respond
specifically to antigen on cell surface,
resulting in killing those cells and
activating other cells that clear the
antigen.

In cancer treatment, often
surgery, chemotherapy,
and radiotherapy does not
work eg. in malignant
melanoma.
Thus a new type of therapy
is thought. One of this is
IMMUNOTHERPY.

Cancer Immunotherapy
Aim:
To activate the patient’s
immune system to specifically
recognize and destroy human
tumor cells

Since the first use of smallpox vaccine in the late
1700s, therapies have been used to activate the
immune system to combat various infectious
diseases. Growing understanding of how cancer
cells challenge the immune system has given
hope for therapeutic vaccines that maybe able to
overcome the limitations of current cancer
therapies.
Therapeutic approaches for cancer
immunotherapy generally fall in to three
categories:
I.
Passive Immuntherapy
II.
Non-specific Immunotherapy
III.
Active Specifuc Immunotherpy

Passive Immunotherpy
Uses monoclonal antibodies to selectively
interfere with tumor cell functioning. What is
needed is
1. A monoclonal antibody specific for the cancer
cell attached to
2. A cytotoxic drug, toxin or radioactive atoms that
kills the cell once it gets inside.
Non-specific Immunotherapy
Uses compounds including cytokines such as
interferon, interleukin and BCG, that upregulates
the general immune system response to cancer.
However, cytokine therapy suffers the same
limitations as chemotherapy in that cytokines lack
selectivity and are associated with significant
toxicity. Eg. Interferon and IL-2 used in the
treatment of melanoma have significant side
effects in most patients.

Active Specific Immunotherapy
Purified antigens, peptides, gene-based systems, or
antigens contained in whole cells or cell lysates are
used in active specific immunotherapy for cancer.
They are also called therapeutic cancer vaccines.
Unlike chemotherapy, active specific
immunotherapy does not directly kill cancer cells,
but generate a specific and targeted humoral
and/or cellular immune response against the
cancer and stimulate an increase in the number
and type of immune cells and antibodies capable of
responding to cancer. Also therapeutic cancer
vaccines may activate the immune system to
overcome the immunosuppression caused by tumor
growth and development.
Cytokines that have been shown to
inhibit tumor establishment
• IL-2 - Activates T cell, NK cells and
marophages
• IL-4 - Activates T and B cells
• IL-6 - Augments B cell growth and Ab
production
• IL-12 - Stimulate T and NK cells to produce IFN-
• IL-15 – Activates T cell, NK cells, LAK, and TIL
• GM-CSF - Accelerates hematopoietic recovery
after
chemotherapy
• TNF- - Stimulates target cells, induces MHC
• IFN- - Induce cytotoxicity

Immunotherapy is still in its
infancy but holds great
potential.
Well anyway, Good luck on
your USMLE and the Match!
Document Outline
- Slide 1
- Slide 2
- Slide 3
- Slide 4
- Slide 5
- Slide 6
- Slide 7
- Slide 8
- Slide 9
- Slide 10
- Slide 11
- Slide 12
- Slide 13
- Slide 14
- Slide 15
- Slide 16
- Slide 17
- Slide 18
- Slide 19
- Slide 20
- Slide 21
- Slide 22
- Slide 23
- Slide 24
- Slide 25
- Slide 26
- Slide 27
- Slide 28
- Slide 29
- Slide 30
- Slide 31
- Slide 32
- Slide 33
- Slide 34
- Slide 35
- Slide 36
- Slide 37
- Slide 38
- Slide 39
Wyszukiwarka
Podobne podstrony:
Immunologia nowotworów
Immunologia Nowotworów
Immunoterapia nowotworów
immunologia nowotworow
Immunologia nowotworow ok, Immunologia
immunologia nowotworów
Immunoterapia nowotworów (moja)
IMMUNOLOGIA NOWOTWORÓW
199611 immunoterapia nowotworow
Immunohistochemia nowotworów
Immunologia nowotworów
Immunologia Nowotworów
Immunologia nowotworoTŽ w, niedobory odpornosTŽ ci, psychoneuroimmunologia
Immunologia Nowotworów
Immunoterapia nowotworów
więcej podobnych podstron