Am J Psychiatry 157:4, April 2000
641
BRIEF REPORTS
Proton Magnetic Resonance Spectroscopy
of the Medial Prefrontal Cortex in Patients
With Deficit Schizophrenia: Preliminary Report
Pascal Delamillieure, M.D., Jésus Fernandez, M.D., Jean-Marc Constans, M.D.,
Perrine Brazo, M.D., Karim Benali, M.D., Pascale Abadie, M.D., Ph.D.,
Thierry Vasse, M.D., Florence Thibaut, M.D., Ph.D., Patrick Courthéoux, M.D.,
Michel Petit, M.D., and Sonia Dollfus, M.D., Ph.D.
Objective: Proton magnetic resonance spectroscopy (
1
H-MRS) was used to study me-
dial prefrontal metabolic impairments in schizophrenic patients with the deficit syndrome.
Method: The subjects were 22 schizophrenic patients categorized as deficit (N=5) or non-
deficit (N=17) and 21 healthy subjects.
1
H-MRS was performed for the right and the left me-
dial prefrontal cortex. Results: The patients with the deficit syndrome had significantly
lower ratios of N-acetylaspartate to creatine plus phosphocreatine than did the healthy sub-
jects or nondeficit patients. Conclusions: As N-acetylaspartate levels could reflect neu-
ronal density and/or viability, this finding suggests a neuronal loss in the medial prefrontal
cortex of deficit patients.
(Am J Psychiatry 2000; 157:641–643)
P
roton magnetic resonance spectroscopy (
1
H-MRS)
can measure levels of cerebral metabolites such as N-
acetylaspartate, which has been described as a neuronal/
axonal marker, choline, which is known to increase in
myelin breakdown, and myo-inositol, a glial cell marker
whose increase could reflect a gliosis. Studies with
1
H-
MRS in schizophrenia have shown contradictory find-
ings (1–3), which could be due to heterogeneous patient
groups. Therefore, the aim of this study was to examine,
with a single-voxel spectroscopy technique, whether a
low ratio of N-acetylaspartate to creatine is associated
with primary and enduring negative symptoms in
schizophrenic patients with the deficit syndrome (4).
METHOD
The Schedule for the Deficit Syndrome (5) was used to evaluate 22
right-handed schizophrenic patients (DSM-IV) without history of
head injury, past or present neurological disorders, alcoholism, or
drug abuse. Five were categorized as having the deficit syndrome,
and 17 were categorized as nondeficit. We matched 21 healthy sub-
jects with the patients for age, educational level, sex, and handed-
ness. None of the comparison subjects had any history of the lifetime
psychiatric disorders evaluated with the National Institute of Mental
Health Diagnostic Interview Schedule (6), organic illness, alcohol-
ism, or drug abuse. After complete description of the study to the
subjects, written informed consent was obtained.
1
H-MRS was performed on a General Electric Signa 1.5-T MRI
system with a standard quadrature head coil. Proton spectra were
obtained from an 8-cm
3
voxel in the medial prefrontal cortex includ-
ing the anterior cingulate region. The spectra were obtained by using
a stimulated echo acquisition mode (STEAM) sequence (TE/TR=30
msec/1500 msec).
Repeated measures analysis of variance (ANOVA) was used to
test the metabolite differences between groups (deficit versus non-
deficit versus healthy). Post hoc pairwise comparisons with Bonfer-
roni correction were used to identify which group differences ac-
counted for the significant overall F value (Bonferroni/Dunn tests). A
separate repeated measures ANOVA with the same factors was per-
formed to compare untreated and treated patients. All of these tests
were two tailed, and results were considered significant with proba-
bility levels of p
<
0.05. Correlations between metabolite ratios and
length of illness (time between first episode and time of evaluation),
dose of antipsychotic in chlorpromazine equivalents, and level of ex-
posure to antipsychotic medications (chlorpromazine-equivalent
dose times years of exposure) were performed by Spearman tests.
RESULTS
One patient was drug naive, and four had been free
of medication for at least 6 months. Among the treated
Received Dec. 21, 1998; revisions received July 6 and Aug.
30, 1999; accepted Sept. 2, 1999. From the Groupe de Recher-
che Centre Esquirol and the Département d’Imagerie par Réso-
nance Magnétique, Centre Hospitalier et Universitaire; and the
Centre Cycéron, Caen, France. Address reprint requests to Dr.
Dollfus, Groupe d’Imagerie Neurofonctionnelle, Université de
Caen. CNRS FRE 2233, CEA LRC 13V, Centre Esquirol, Centre
Hospitalier et Universitaire, 14000 Caen, France; dollfus-s @
chu-caen.fr (e-mail).
Sponsored by the French Health Ministry in a National Research
Program on schizophrenia.
642
Am J Psychiatry 157:4, April 2000
BRIEF REPORTS
patients, two without and three with the deficit syn-
drome were receiving atypical neuroleptics. Each of
the treated patients was in a stable phase, defined by
no change in dose of antipsychotic medication for 2
months.
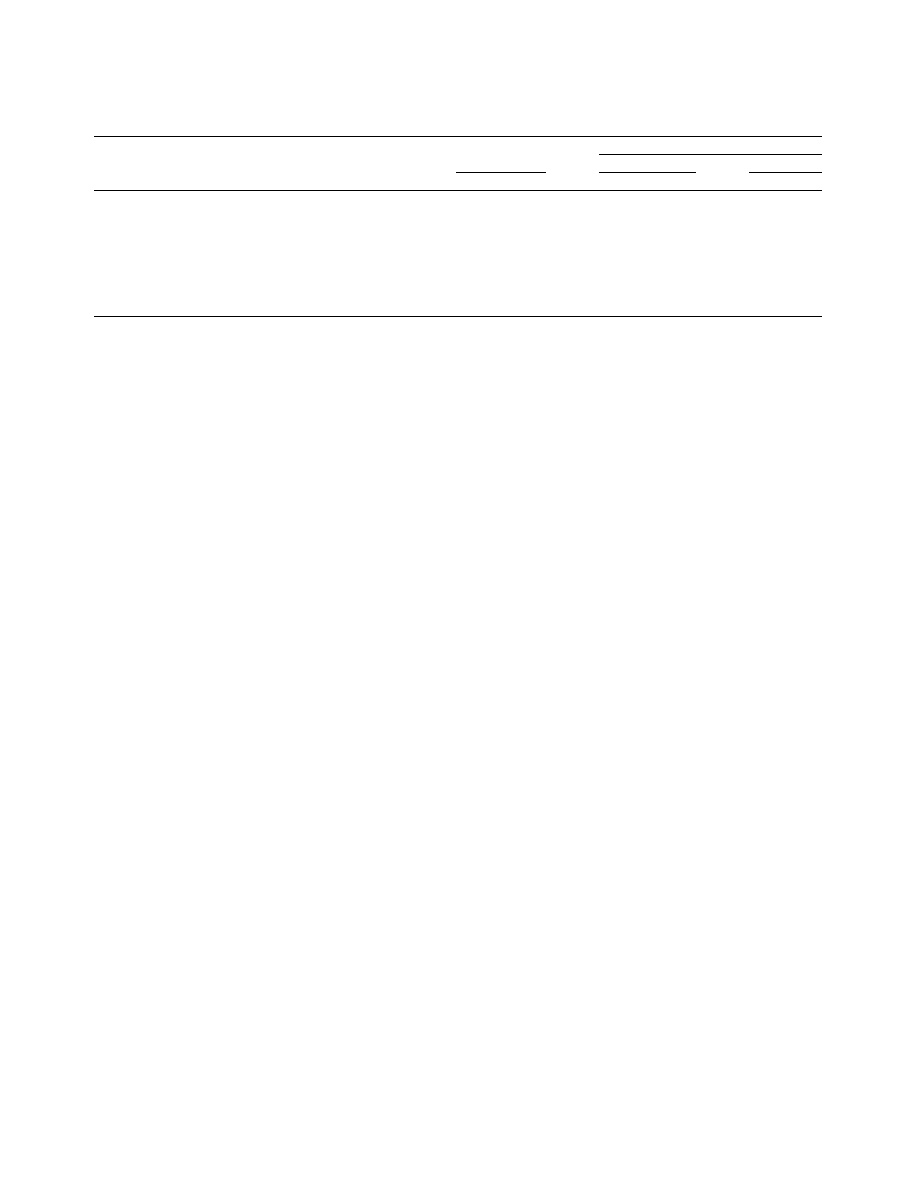
The deficit and nondeficit schizophrenic patients did
not differ significantly in age, age at onset of illness,
or duration of illness. ANOVA showed a significant
difference in N-acetylaspartate/creatine among the
healthy subjects, schizophrenic patients with the deficit
syndrome, and nondeficit patients (table 1). Post hoc
analyses showed that the deficit patients had signifi-
cantly lower ratios of N-acetylaspartate/creatine than
the healthy subjects (p=0.01) and the nondeficit pa-
tients (p=0.009). No difference in myo-inositol/creat-
ine or choline/creatine was observed among the deficit
patients, nondeficit patients, and healthy subjects. No
difference in any metabolite ratio was noted between
the untreated and treated patients. No significant cor-
relation was found between any metabolite ratio and
length of illness, dose of medication, or level of expo-
sure to antipsychotics.
DISCUSSION
The major finding was a lower N-acetylaspartate/
creatine ratio in the prefrontal cortex of the patients
with the deficit syndrome than in the healthy subjects
and nondeficit patients. As N-acetylaspartate could re-
flect neuronal density, this result suggests a neuronal
loss in the prefrontal cortex of deficit patients, sup-
porting previous results showing hypofrontality in def-
icit schizophrenia (7). This finding is also consistent
with that of Shioiri et al. (8), who found, by using
31
P-
MRS, that abnormalities in phosphomonoesters and
β
-
ATP were related to the severity of negative symptoms
but not specifically to primary negative symptoms. A
lower than normal N-acetylaspartate/creatine ratio
was also observed by Bertolino et al. (1) in the dorso-
lateral prefrontal cortex of schizophrenic patients but
was not particularly linked to negative symptoms. The
absence of high ratios of choline/creatine and myo-
inositol/creatine in our patients with the deficit syn-
drome is not consistent with gliosis and therefore does
not support a neurodegenerative process in deficit
schizophrenia.
As no correlation between N-acetylaspartate/creatine
and length of illness in the deficit patients was ob-
served, this result suggests that the low N-acetylaspar-
tate/creatine ratio probably did not reflect an ongoing
process. Antipsychotic treatment did not affect the N-
acetylaspartate level, since there was no difference be-
tween the treated and untreated patients, and no rela-
tionship between N-acetylaspartate/creatine and the
dose of antipsychotic or level of exposure to medication
was noted. This is consistent with the result of Ber-
tolino et al. (9), who found a low N-acetylaspartate/
creatine ratio in the dorsolateral prefrontal cortex of
unmedicated schizophrenic patients, suggesting that
lower N-acetylaspartate/creatine ratios are independent
of drug effects.
The absence of segmentation analyses is one major
limit of the present study. The voxels contained various
proportions of gray and white matter. Determining
these proportions could be informative since some
studies in schizophrenia have shown low levels of N-
acetylaspartate in white but not gray matter (10). Thus,
the lower N-acetylaspartate level observed in our study
could be due to a larger prefrontal white matter volume
in deficit patients, as has been suggested (11).
In conclusion, these preliminary results provide sup-
port for neuronal loss in the prefrontal cortex of deficit
schizophrenic patients, but further studies with seg-
mentation analyses are needed to determine the reason
for these lower N-acetylaspartate levels.
REFERENCES
1. Bertolino A, Nawroz S, Mattay VS, Barnett AS, Duyn JH,
Moonen CT, Frank JA, Tedeschi G, Weinberger DR: Region-
ally specific pattern of neurochemical pathology in schizo-
phrenia as assessed by multislice proton magnetic resonance
spectroscopic imaging. Am J Psychiatry 1996; 153:1554–
1563
2. Buckley PF, Moore C, Long H, Larkin C, Thompson P, Mulvany
F, Redmond O, Stack JP, Ennis JT, Waddington JL: 1H-mag-
netic resonance spectroscopy of the left temporal and frontal
lobes in schizophrenia: clinical, neurodevelopmental, and
cognitive correlates. Biol Psychiatry 1994; 36:792–800
TABLE 1. Ratios of Metabolites in the Medial Prefrontal Cortex of Healthy Subjects and Schizophrenic Patients With and Without
the Deficit Syndrome
Metabolite Ratio and Brain Hemisphere
Healthy Subjects
(N=21)
Schizophrenic Patients
Nondeficit (N=17)
Deficit (N=5)
Mean
SD
Mean
SD
Mean
SD
Ratio of N-acetylaspartate to creatine plus phosphocreatine
Left
a
1.35
0.21
1.42
0.23
1.15
0.36
Right
a
1.33
0.16
1.27
0.22
1.13
0.06
Ratio of choline to creatine plus phosphocreatine
Left
0.88
0.13
0.97
0.17
0.86
0.17
Right
0.91
0.11
0.93
0.18
1.06
0.56
Ratio of myo-inositol to creatine plus phosphocreatine
Left
0.66
0.13
0.69
0.26
0.70
0.18
Right
0.72
0.15
0.62
0.15
0.63
0.03
a
Significant group effect (F=3.45, df=2, 41, p
<
0.04; repeated measures ANOVA)

Am J Psychiatry 157:4, April 2000
643
BRIEF REPORTS
3. Williamson PC, Bartha R, Drost DJ, Malla A, Carr T, Canaran
G, Densmore M, Neufeld RW: Medial prefrontal 1H MRS and
MRI findings in never-treated schizophrenics and healthy con-
trols (abstract). Schizophr Res 1998; 29:101
4. Carpenter WT Jr, Heinrichs DW, Wagman AM: Deficit and
nondeficit forms of schizophrenia: the concept. Am J Psychia-
try 1988; 145:578–583
5. Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Car-
penter WT Jr: The Schedule for the Deficit Syndrome: an in-
strument for research in schizophrenia. Psychiatry Res 1989;
30:119–123
6. Robins LN, Helzer JE, Croughan J, Ratcliff KS: National Insti-
tute of Metal Health Diagnostic Interview Schedule: its history,
characteristics and validity. Arch Gen Psychiatry 1981; 38:
381–389
7. Tamminga CA, Thaker GK, Buchanan R, Kirkpatrick B, Alphs
LD, Chase TN, Carpenter WT: Limbic system abnormalities
identified in schizophrenia using positron emission tomogra-
phy with fluorodeoxyglucose and neocortical alterations with
deficit syndrome. Arch Gen Psychiatry 1992; 49:522–530
8. Shioiri T, Kato T, Inubushi T, Murashita J, Takahashi S: Corre-
lations of phosphomonoesters measured by phosphorus-31
magnetic resonance spectroscopy in the frontal lobes and
negative symptoms in schizophrenia. Psychiatry Res 1994;
55:223–235
9. Bertolino A, Callicott JH, Elman I, Mattay VS, Tedeschi G,
Frank JA, Breier A, Weinberger DR: Regionally specific neu-
ronal pathology in untreated patients with schizophrenia: a
proton magnetic resonance spectroscopic imaging study. Biol
Psychiatry 1998; 43:641–648
10. Lim KO, Adalsteinsson E, Spielman D, Sullivan EV, Rosen-
bloom MJ, Pfefferbaum A: Proton magnetic resonance spec-
troscopic imaging of cortical gray and white matter in schizo-
phrenia. Arch Gen Psychiatry 1998; 55:346–352
11. Buchanan RW, Breier A, Kirkpatrick B, Elkashef A, Munson
RC, Gellad F, Carpenter WT Jr: Structural abnormalities in
deficit and nondeficit schizophrenia. Am J Psychiatry 1993;
150:59–65
Wyszukiwarka
Podobne podstrony:
Clinical and neuropsychological correlates of proton magnetic resonance spectroscopy detected metabo
Brain Proton Magnetic Resonance Spectroscopy
The relationship of Lumbar Flexion to disability in patients with low back pain
Application of Magnetic Resonance Spectroscopy in the Mental Diseases of Schizophrenia and Autism
Applications of magnetic resonance spectroscopy in radiotherapy treatment planning
Microsoft Word Spectre of the Black Rose Sam
Shock waves in molecular solids ultrafast vibrational spectroscopy of the first nanosecond
Brain to Serum Lithium Ratio and Age An In Vivo Magnetic Resonance Spectroscopy Study
The History of the USA 6 Importand Document in the Hisory of the USA (unit 8)
Existence of the detonation cellular structure in two phase hybrid mixtures
fitopatologia, Microarrays are one of the new emerging methods in plant virology currently being dev
Mossbauer study of the retained austenitic phase in
Lord of the Flies Character Changes in the Story
Contrastic Rhetoric and Converging Security Interests of the EU and China in Africa
Mossbauer study of the retained austenitic phase in
Knights of the Round Table inet in C
25 Because of the Angels – Angelic Intervention in Human Lives
Knights of the Round Table inst in B
więcej podobnych podstron