SPINE Volume 27, Number 8, pp E207–E214
©2002, Lippincott Williams & Wilkins, Inc.
Interexaminer Reliability of Low Back Pain Assessment
Using the McKenzie Method
Sinikka Kilpikoski, MSc,* Olavi Airaksinen, MD, DmedSci,†
Markku Kankaanpa¨a¨, MD, DmedSci,†‡ Pa¨ivi Leminen, PT,*
Tapio Videman, MD, DmedSci,
§ and Markku Alen, MD, DmedSci*†
Study Design. A test–retest design was used.
Objective. To assess interexaminer reliability of the
McKenzie method for performing clinical tests and clas-
sifying patients with low back pain.
Summary of Background Data. Clinical methods and
tests classifying patients with nonspecific low back pain
have been based mainly on symptom duration or ex-
tent of pain referral. The McKenzie mechanical diagnos-
tic and classification approach is a widely used nonin-
vasive, low-technology method of assessing patients
with low back pain. However, little is known about the
interexaminer reliability of the method, previous stud-
ies having yielded conflicting results.
Methods. For this study, 39 volunteers with low back
pain, mean age 40 years (range, 24 –55 years), were
blindly assessed by two physical therapists trained in the
McKenzie method. The variability of two examiners for
binary decisions was expressed by the kappa coefficient,
and by the proportion of observed agreement, as calcu-
lated from a 2
⫻ 2 contingency table of concordance.
Results. On the basis of pure observation alone,
agreement among clinical tests on the presence and
direction of lateral shift was 77% (
⫽ 0.2; P ⬍ 0.248)
and 79% (
⫽ 0.4; P ⬍ 0.003), respectively. Agreement
on the relevance of lateral shift and the lateral compo-
nent according to symptom responses was 85% (
⫽
0.7; P
⬍ 0.000) and 92% (
⫽ 0.4; P ⬍ 0.021), respec-
tively. Using the repeated movements and static end-
range loading strategy to define the centralization phe-
nomenon and directional preference, agreement was
95% (
⫽ 0.7; P ⬍ 0.002) and 90% ( ⫽ 0.9; P ⬍ 0.000),
respectively. When patients with low back pain were clas-
sified into the McKenzie main syndromes and into specific
subgroups, agreement was 95% (
⫽ 0.6; P ⬍ 0.000) and
74% (
⫽ 0.7; P ⬍ 0.000), respectively.
Conclusions. Interexaminer reliability of the McKen-
zie lumbar spine assessment in performing clinical
tests and classifying patients with low back pain into
syndromes were good and statistically significant when
the examiners had been trained in the McKenzie method.
[Key words: agreement, classification, low back pain as-
sessment, McKenzie method, reliability] Spine 2002;27:
E207–E214
The origin of low back pain (LBP) remains unknown in
most cases. Even after careful clinical assessment and
specific measurements, the precise cause of the symptoms
may be identified in only 15% of cases.
24
Previous clas-
sifications used to subgroup these patients with “nonspe-
cific” LBP have mainly been based on symptom duration
or extent of pain referral.
24
This has been a major weak-
ness in etiologic research, and also in preventive and
treatment interventions.
Good interexaminer reliability is crucial for any clas-
sification of patients with LBP. Tests that could identify
etiopathogenetically separate subgroups would assist re-
lated research. It has also been suggested that patients
with LBP who undergo specific management based on an
assigned classification do better than patients whose
treatment is not based on their pretreatment classifica-
tion.
20,24
Therefore, the use of physical signs and symp-
tom behavior as criteria for classifications of LBP is an
important and promising area in clinical decision making
and trials.
3,5,11,14 –17,20,24
The McKenzie mechanical diagnostic and classifica-
tion approach is a noninvasive, low-technology, inex-
pensive method of assessing patients with LBP that uses
physical signs, symptom behavior, and their relation to
end-range lumbar test movements to determine appro-
priate classification and treatment (Table 1, Appendix
1). The McKenzie method classifies mechanical LBP into
three main syndromes: postural, dysfunction, and de-
rangement (Appendix 1).
15–17
Interexaminer reliability of the McKenzie approach in
performing clinical tests and classifying patients with
LBP into syndromes has been previously investi-
gated.
4 –7,9,13,18,19,23,25,26
Kilby et al
13
suggested that the
“McKenzie algorithm” is reliable in the examination of
pain behavior and pain response with repeated move-
ments, but unreliable in the detection of end-range pain
and lateral shift. Riddle and Rothstein
23
found that the
McKenzie approach was unreliable when physical ther-
apists classified patients into McKenzie syndromes. They
suggested that a potential source of unreliability was in
determining whether the patient had a lateral shift and, if
so, in which direction, and whether the patient’s pain
centralized or peripheralized during test movements.
23
From the *Department of Health Sciences, University of Jyva¨skyla¨,
Jyva¨skyla¨, Finland, the †Department of Physical Medicine and Reha-
bilitation, Kuopio University Hospital, Kuopio, Finland, the ‡Univer-
sity of Kuopio, Department of Physiology, Kuopio, Finland, and the
§Faculty of Rehabilitation Medicine, University of Alberta, Edmonton,
Canada.
Supported by the McKenzie Institute, Robhauptery, Germany.
Acknowledgment date: March 8, 2001.
First revision date: June 18, 2001.
Second revision date: September 12, 2001.
Acceptance date: November 6, 2001.
The manuscript submitted does not contain information about medical
devices.
No funds were received in support of this study.
E207

However, in a previous study,
18
interexaminer reliability
between two therapists trained in the McKenzie method
seemed to be high for classifying patients with LBP into
McKenzie syndromes, and excellent for judging pain sta-
tus change, including the centralization phenomenon,
during examination of the lumbar spine.
9,18,19
Donahue et al
4
found that the McKenzie method was
unreliable for detecting the presence of a lateral shift, but
that a relevant lateral component could be reliably de-
tected using symptom response to repeated movements.
On the other hand, Tenhula et al
25
showed a significant
relation between positive results on a contralateral side-
bending movement test and a lumbar lateral shift, indi-
cating that the former is a useful clinical test for confirm-
ing the presence of a lateral shift in patients with LBP.
The obvious discrepancies among earlier studies on
agreement and reliability of the McKenzie method
prompted this study.
This study aimed to assess the interexaminer agree-
ment among physical therapists trained in the McKenzie
method as they performed clinical tests and classified
patients with LBP. The specific aims of the study were to
test interexaminer reliability 1) in determining the pres-
ence and direction of lateral shift by using pure observa-
tion alone, the relevance of lateral shift and the lateral
component as noted by symptom responses to repeated
movement, and the centralization phenomenon and di-
rectional preference in relation to the repeated move-
ment end-range test pattern, and 2) in classifying patients
with LBP into the main McKenzie syndromes and their
specific subgroups (Table 1, Appendix 1).
Methods
Participants.
For this study, 39 volunteers with LBP, mean age
40 years (range, 24 –55 years), with or without radiation to the
lower limb, randomly drawn from a randomized ongoing
wider study
12
at Kuopio University Hospital, participated in
this study (Table 2). Participants were recruited through the
Kuopio Occupational Health Center (Kuopio, Finland), where
they had sought medical attention for LBP. The participants
had experienced chronic low back disorder with symptom du-
ration longer than 3 months and moderate functional disability
that enabled them to work with only occasional absences. In
the initial clinical examination at the health center, the cause of
the back pain was confirmed to be nonspecific. Patients with
radicular symptoms (radiating pain below the knee, loss of
sensation, muscle dysfunction, or loss of reflexes), disc pro-
lapse, severe scoliosis, spondyloarthrosis, previous back sur-
gery, and other specific and serious causes of back pain were
excluded from the study.
12
Examiners.
The examiners, two physical therapists, possessed
a high level of training, averaging 5 years of clinical experience
in the McKenzie method. They were diploma and examination
credential holders in spine mechanical diagnosis and therapy.
Table 1. Definitions and Operational Terms of the McKenzie Method
Presence and direction of lateral shift
“Lateral displacement or deviation of the trunk, in relation to the pelvis in the frontal plane, viewed from
behind (C7–S1), while the patient is in the standing position. If the trunk is shifted to the right, relative
to the pelvis, this is a right shift.
16,18
Deformity
“Deformity may be a feature of some acute derangements (Appendix 1). The patient has a sudden loss of
movement that corresponds to the onset of pain. This loss of movement is severe enough to cause the
patient to be unable to actively move out of that abnormal posture. Depending on the direction of the
blockage of the movement, patients may present with the deformity of kyphosis (unable to straighten
up), deformity of increased lordosis (unable to bend forward), or lateral shift (unable to cross the
midline in frontal plane). A deformity is relevant only when attempted correction influences the
symptoms.”
5,18
Relevance of lateral shift
“A shift that is related to the patient’s present symptoms, ie, patient’s symptoms centralize to the lumbar
spine while attempt is made to correct the deformity of the lateral shift.”
16,18
Relevant lateral component
“This term is used for patients with unilateral or asymmetrical symptoms who do not centralize by
movements in sagittal plane. Centralization can only be achieved with asymmetrical lateral movements
such as side-glides or rotations. If symptoms can be resolved simply by performing extension in the
sagittal plane, the lateral component is considered to be insignificant.”
16,18
Centralization phenomenon
“Describes the phenomenon by which distal limb pain emanating from, though not necessarily felt in
spine, is immediately or eventually abolished in response to the deliberate application of loading
strategies. Such loading causes a decrease or abolition of peripheral pain which appears to
progressively retreat in a proximal direction. As this occurs there may be a simultaneous development
or increase in proximal symptoms. The phenomenon occurs only in derangement syndrome (Appendix
1).”
6,7,9,15–17,26
Directional preference
“Used to describe the phenomenon of preference for movement in one direction, which is a characteristic
of the derangement syndrome (Appendix 1). It describes the situation when movements in one direction
will improve pain and the limitation of range, whereas movements in the opposite direction cause signs
and symptoms to worsen.”
6,7,15–17
Table 2. Characteristics of Subjects
Mean (Range)
No. (%) of Study
Participants
Gender
Women
15 (38)
Men
24 (62)
Age (yr)
40 (24–55)
Symptom duration, yr
14 (1–38)
Symptoms at study entry
Symptom free
2 (5)
Acute:
⬍7 days
5
(13)
Subacute:
⬎7 days ⬍7 weeks
9 (23)
Chronic:
⬎7 weeks
23 (59)
No. of previous episodes
1–5
16 (41)
6–10
7 (18)
⬎10
16 (41)
E208 Spine
•
Volume 27
•
Number 8
•
2002
Procedure.
After receiving an oral and written explanation of
what would be required of them, the participants all signed an
informed consent.
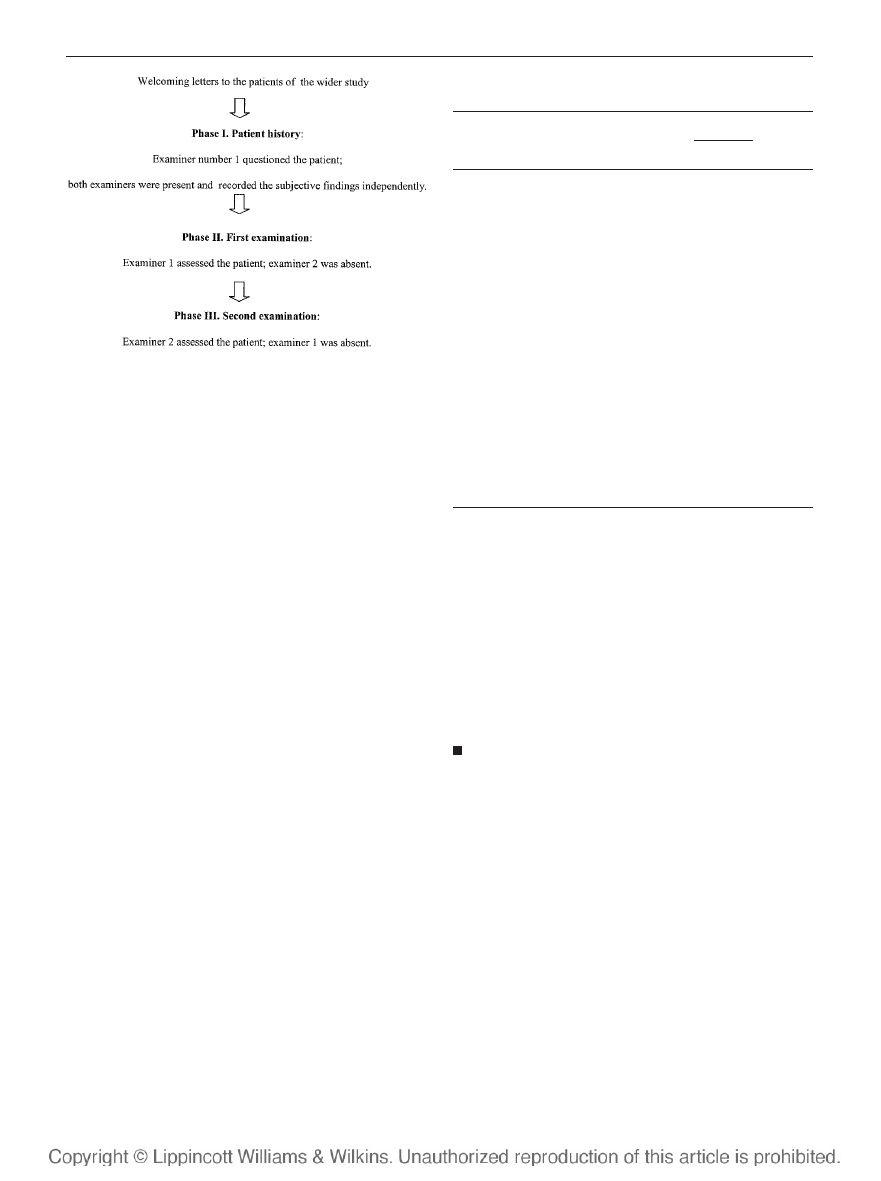
The clinical assessment procedure is shown in Figure 1. In
brief, before entering the current study, the patients with LBP
were assessed medically, first by a general practitioner, and
second by a specialist in physical and rehabilitation medicine.
Patients fulfilling the inclusion criteria were randomly selected
to participate in this clinical assessment.
12
The participants
were examined independently by two physical therapists in
succession (the duration of an assessment session was approx-
imately 1
1
⁄
2
hours). The examiners were randomly assigned to
be examiner number 1 and examiner number 2 so that each
was examiner number 1 in 50% of the cases.
The data were collected using the McKenzie lumbar spine
assessment form.
16
The assessment consisted of taking a his-
tory (verbally), observing the spinal range of motion, and com-
pleting specific test movements. The subjects were allowed to
communicate only with examiner number 1 during the history-
taking period. During the questioning, leading questions and
verbal clues were avoided.
The physical examination was performed twice, once by
each examiner. The participants were asked to stand in their
normal relaxed position, with their feet approximately 20 cm
apart, on a marked line. A plumbline passing through C7 to S1
assisted in identifying the presence and direction of a lateral
shift.
The examiners completed the lumbar spine assessment
forms and data collection forms, which were based on the orig-
inal McKenzie form. The syndrome categories were expanded
to subgroups, and the category “other” included inconclusive
mechanical pain patterns and nonmechanical conditions, in
which pain was not presumed to originate from the spine (Ap-
pendix 1). After completing the forms, the examiners sealed
them in envelopes for storage pending data analysis.
Ethics.
The study was approved by the Kuopio University
Hospital Human Ethics Committee.
Statistical Methods.
The variability of the two examiners in
binary decisions was expressed by the kappa (
) coefficient, and
by the proportion of observed agreement. The kappa statistic
provides an index of chance-corrected agreement. Together,
these indexes offer a single expression that summarizes the re-
sults from a 2
⫻ 2 contingency table of concordance.
1,2,8,10
The data were analyzed using SPSS Version 9.0 for the Win-
dows program. Two-sided significance was defined as a P value
less than 0.05. The verbal translations of the kappa scores are
as follows: 0 to 0.20 (poor agreement), 0.21 to 0.40 (slight
agreement), 0.41 to 0.60 (moderate agreement), 0.61 to 0.80
(good agreement), and 0.81 to 1 (very good/excellent
agreement).
1
Results
Lateral Shift and Lateral Component
Visual agreement on the presence and direction of lateral
shift was 77% (
⫽ 0.2; P ⬍ 0.248) and 79% ( ⫽ 0.4;
P
⬍ 0.003), respectively (Tables 3 and 4). The examiners
agreed that the shift was to the right in 15 (54%) of 28
cases. Agreement on the relevance of lateral shift and the
lateral component according to symptom responses was
85% (
⫽ 0.7; P ⬍ 0.000) and 92% ( ⫽ 0.4; P ⬍
0.021), respectively (Table 3).
Centralization Phenomenon and
Directional Preference
Among 34 (87%) patients, whose pain was centralizing,
agreement was 95% (
⫽ 0.7; P ⬍ 0.002) on the central-
ization phenomenon and 90% (
⫽ 0.9; P ⬍ 0.000) on
directional preference. The agreed-on primary direction
was side-gliding to left in 16 patients (47%), and to right
in 9 patients (26%), and extension in 7 patients (21%)
(Tables 3 and 4).
Figure 1. Assessment flow chart for a patient with low back pain.
Table 3. Results of Clinical Tests and McKenzie Main
Syndrome Classification
Examiner 1
Examiner 2
Total
⫹
⫺
Presence of lateral shift (N
⫽ 39)
⫹
28
3
31
⫺
6
2
8
Total
34
5
39
Relevance of lateral shift (N
⫽ 39)
⫹
22
2
24
⫺
4
11
15
Total
26
13
39
Relevance of lateral component (N
⫽ 39)
⫹
1
2
3
⫺
1
35
36
Total
2
37
39
Centralization phenomenon (N
⫽ 39)
⫹
34
1
35
⫺
1
3
4
Total
35
4
39
Directional preference (N
⫽ 39)
⫹
32
1
33
⫺
3
3
6
Total
35
4
39
McKenzie main syndromes (N
⫽ 39)
⫹
35
1
36
⫺
1
2
3
Total
36
3
39
E209
Interexaminer Reliability of the McKenzie Method
•
Kilpikoski et al
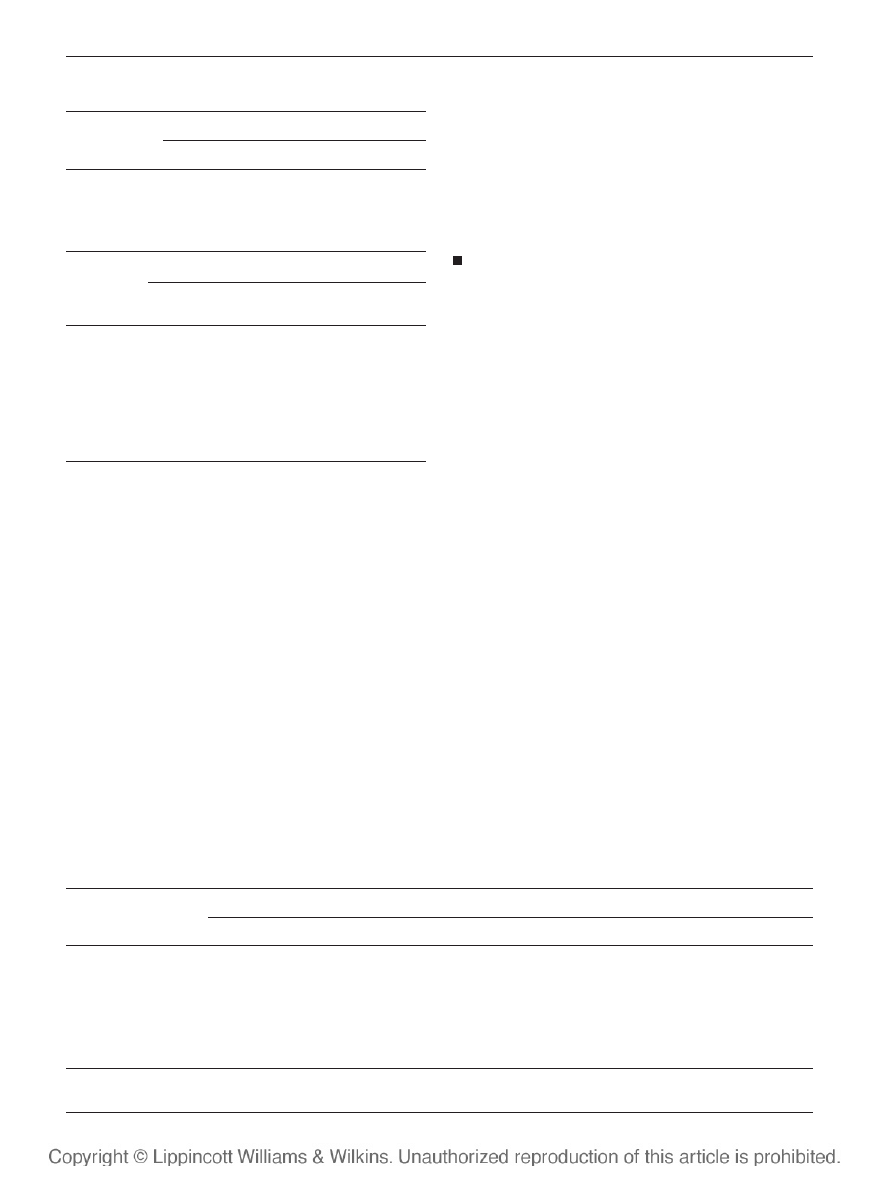
Main Syndromes According to the
McKenzie Approach
In classifying patients with LBP into the main syn-
dromes, agreement was 95% (
⫽ 0.6; P ⬍ 0.000). Both
examiners assigned the patients mainly into the derange-
ment syndrome group (90%; 35 of 39 patients). Two
patients were symptom free. The examiners disagreed in
two (5%) cases (Table 3).
Specific Subgroups According to the
McKenzie Approach
In classifying patients with LBP into specific subgroups,
agreement was 74% (
⫽ 0.7; P ⬍ 0.000). The examiners
agreed in defining the same derangement subgroups for
27 (69%) patients. They disagreed about 11 (28%) pa-
tients (Table 5). Of these 11 cases, 9 were classified as
“posterior derangement syndromes,” but into different
subgroups, as shown in Table 5, and 2 were assigned to
a totally different subgroup. One case was classified as
“posterior derangement syndrome 3” by Examiner 2 and
as “extension dysfunction syndrome” by Examiner 1,
and one case was classified as “posterior derangement
syndrome 4” by Examiner 1 and as “mechanically incon-
clusive” by Examiner 2. These two patient groups were
not included into the 2
⫻ 2 contingency table by classi-
fication, but were coded as symptom-free/other group
(value
⫽ 0) to avoid asymmetry in the 2 ⫻ 2 contingency
table (Table 5).
Discussion
In this study, concurrence on certain clinical tests based
on patients’ symptom behavior was found to be moder-
ate to excellent. The study is among those that describe
the proportion of those responding to extension and lat-
eral forces. Donelson et al
6
found that 40% of their study
group had a directional preference for extension. In our
study 64% of the patients responded to lateral forces,
whereas only 18% responded to extension. On the basis
of these responses, patients were classified into the Mc-
Kenzie syndromes with a moderate to good level of
agreement. The reliability was best in defining the cen-
tralization phenomenon, directional preference, and rel-
evance of lateral shift, good in determining main syn-
dromes and subgroup classification, and moderate in
defining the lateral component. Reliability was accept-
able also for defining direction of lateral shift.
The three main mechanical syndromes are postural,
dysfunction, and derangement. “They are characterized
by completely different patterns of mechanical and
symptomatic responses when LBP patients are examined
by a structured repeated end-range movement and static
loading strategy. Each syndrome response to repeated
movement is different from that of other syndromes.”
17
(Appendix 1) “Clinically, patients with pain of postural
syndrome are not often seen.”
17
In fact, no case in the
current study was classified primarily as “postural syn-
drome,” as would be expected of patients with chronic
low back disorder.
As found in the current study, “most patients develop
pain and seek assistance as a result of derangement.”
15
(Tables 3 and 5). This would account for the absence of
Table 4. Distribution of Lateral Shift Directions and
Directional Preferences
Examiner 1
Examiner 2
No shift
Left shift
Right shift
Total
Direction of lateral shift (N
⫽ 39)
No shift
2*
3
3
8
Left shift
2
7*
2
11
Right shift
1
4
15*
20
Total
5
14
20
39
Examiner 1
Examiner 2
No
Extension
SGL Right/
Extension
SGL Left/
Extension
Total
Directional preference (N
⫽ 39)
No
3*
1
0
0
4
Extension
0
7*
0
2
9
SGL
right/
extension
0
0
9*
0
9
SGL left/
extension
1
0
0
16*
17
Total
4
8
9
18
39
Table 5. Distribution of McKenzie Specific Subgroups
Examiner 1
Examiner 2
Symptom Free/Other
Der 1
Der 2
Der 3
Der 4
Der 5
Der 6
Total
Symptom free/other
2*
0
0
1‡
0
0
0
3
Der 1
0
3*
0
1
1
0
0
5
Der 2
0
0
2*
0
0
0
0
2
Der 3
0
0
0
1*
3
0
0
4
Der 4
1†
0
0
0
14*
0
1
16
Der 5
0
0
0
0
0
1*
0
1
Der 6
0
0
0
1
1
0
6*
8
Total
3
3
2
4
19
1
7
39
Der
⫽ derangement syndrome group.
† Includes extension dysfunction syndrome (n
⫽ 1).
‡ Includes “mechanically inconclusive” (n
⫽ 1).
E210 Spine
•
Volume 27
•
Number 8
•
2002
the other syndromes in such a small patient population.
Only one patient was assigned primarily to the “dysfunc-
tion syndrome” group by Examiner 2, and one was “me-
chanically inconclusive” (Appendix 1, Table 5).
This study had certain limitations. The observation
that most patients fell into the derangement category
accords with McKenzie’s original description of this me-
chanical syndrome as occurring most frequently in those
who seek care. It also is consistent with the findings of a
recent study.
15,18
However, the result from having a
sample that is too homogeneous may be overinflation of
the kappa value. Another limitation of this study was the
rather small study population and the use of only two
examiners.
21–23
Despite these limitations, agreement
was statistically significant, which strengthens the
results.
To ensure internal validity, both examiners per-
formed the physical examination of each patient inde-
pendently. In this way, both examiners could make an
independent judgment about the clinical tests and syn-
drome classification. Repetition of the physical examina-
tion may have caused a problem in examining reliability
because of baseline differences in patients tested twice
consecutively. The symptoms reported by patients could
vary between the initial test situation and the second test
trial. Thus, differences in baseline descriptions could af-
fect classification judgment. This problem also was noted
in previous studies,
5,13,18,19
and may explain some dis-
crepancies between examiners.
Despite the limitations of the study, several conclu-
sions agree with those of previous studies.
3,5,9,13,18,19,25
The findings of poor reliability on observational tests is
replicated in earlier studies.
4,13
The interexaminer agree-
ment in classifying patients into the main McKenzie syn-
dromes and the subgroups was good (Tables 3 and 5).
These results are supported by Kilby et al,
13
who showed
that the “McKenzie algorithm” is reliable for the exam-
ination of pain behavior and pain response with repeated
movements on the basis of clinical evaluations by two
physical therapists partially trained in the McKenzie
method. In addition, Razmjou et al
18
demonstrated that
the intertester reliability between two therapists trained
in the McKenzie method is high for classifying patients
with LBP into the McKenzie syndromes. In contrast,
Riddle and Rothstein,
23
in a large group of patients eval-
uated by multiple therapists, found poor intertester reli-
ability in classifying patients into McKenzie syndromes.
The therapists used in their study had limited or no pre-
vious experience with the McKenzie method, and for
many, their only training was an abbreviated version
provided by the study authors. It is unclear whether the
lack of reliability they found was a product of poorly
trained and inexperienced therapists or an intrinsic un-
reliability of the method itself. In comparison, the find-
ings from the current study and other work
13,18
suggest
that a higher level of training in the McKenzie approach
is a significant factor in achieving reliability among
therapists.
In conclusion, the results of this study suggest that
interexaminer reliability in performing clinical tests and
classifying patients with LBP into the main McKenzie
syndromes seems to be high when the therapists have
been trained in the McKenzie method. Future research
should involve a larger patient population that is more
l i k e l y t o c o n t a i n e n o u g h r a r e m e c h a n i c a l
syndromes.
15–18
Acknowledgment
The authors thank Stephen May, BA, MCSP, Dip MDT
MSc, for his valuable assistance in preparing this article.
Key Point
●
The McKenzie method seems to be a reliable pre-
treatment method for classifying patients with non-
specific low back pain into ethiopathogenetically
separate subgroups.
Appendix 1
The McKenzie syndromes, subgroups, and their clinical
presentation
Postural Syndrome
Definition
Pain is caused by mechanical deformation of normal soft
tissues or vascular insufficiency arising from prolonged
positional or postural stresses, affecting any articular or
contractile structures.
15–17
Clinical Presentation
●
Age: usually not over 30 years
●
Poor posture; no movement loss
●
Intermittent, local pain
●
Better when on the move
Test Movements
●
“Repeated movements” do not reproduce the
pain originating from postural syndrome
●
Pain can be reproduced only by sustained posi-
tions or posture
●
Not progressively worse; no rapid changes in
symptom
16,18
Dysfunction Syndrome
Definition
Pain is caused by mechanical deformation of structurally
impaired soft tissues. These abnormal tissues may be the
product of previous trauma, or inflammatory or degenera-
tive process. These events cause contraction, scarring, ad-
herence, or adaptive shortening. Pain is felt when the ab-
normal tissue is loaded. Dysfunction may be located in
articular or contractile tissue.
15–17
E211
Interexaminer Reliability of the McKenzie Method
•
Kilpikoski et al

Flexion Dysfunction Syndrome
Clinical Presentation
●
Age: usually over 30 years, unless trauma or de-
rangement is the causative factor
●
May present with poor posture, and the patient
always has a loss of movement or function
●
Intermittent pain, only at the end of the range of
flexion
●
No pain during movement; no radiation
Test Movements
●
Repeated movements reproduce pain at the end-
range of flexion, but pain not worse as a result of
repeated flexion
●
Not progressively worse; no rapid changes in
symptoms
16,18
Extension Dysfunction Syndrome
Clinical Presentation
●
Age: usually exceeds 30 years, unless trauma or
derangement is the causative factor
●
Poor posture; patient always presents with a loss
of movement or function
●
Intermittent pain only at the end of the range of
extension
●
No pain during movement; no radiation
●
Difficulties while sleeping in prone position
Test Movements
●
Repeated movements reproduce pain at the end
range of extension; symptoms not worse as a result
of repeated extension
●
Not progressively worse; no rapid changes in
symptoms
16,18
Side-Glide Dysfunction Syndrome
Clinical Presentation
●
Age: usually exceeds 30 years unless trauma or
derangement is the causative factor
●
Poor posture; patient always presents with a loss
of movement or function
●
Intermittent pain only at the end of the range of
side-glide
●
No pain during movement; no radiation
Test Movements
●
Repeated movements reproduce pain at the end
range of side-glide, but pain not worse as a result of
repeated side-glide
●
Not progressively worse; no rapid changes in
symptoms
16,18
Multidirectional Dysfunction Syndrome
●
Clinical presentation and principles of treatment
dependent on the direction of dysfunction (see sin-
gle-plane dysfunction subsyndromes)
Adherent Nerve Root Syndrome
Clinical Presentation
●
Intermittent sciatica
Test Movements
●
Flexion in standing produces leg pain, which
stops on return to the upright position
●
Flexion in lying has no effect on symptoms
●
Repeated extension has no effect on symptoms
●
Leg symptoms are produced at end range of flex-
ion in standing
●
Symptoms do not remain worse after the test
movements are stopped
16,18
Derangement Syndrome
Definition
Internal dislocation of articular tissue, of whatever ori-
gin, that causes a disturbance in normal resting position
of the affected joint surfaces. This deforms the capsule
and periarticular supportive ligaments resulting in pain,
which will remain until such time as the displacement is
reduced or adaptive changes have remodelled the dis-
placed tissues. Internal dislocation of articular tissue ob-
structs movement attempted towards the direction of
displacement. In spinal column derangement syndrome
is caused by internal disruption and displacement of the
fluid nucleus/anulus complex of the outer innervated
anulus fibroses and/or adjacent soft tissues resulting in
back pain alone or back pain and referred pain depend-
ing on the degree of internal displacement and whether
or not this causes compression of the nerve root.
15–17
Derangement 1
Clinical Presentation
●
Central/symmetrical pain, rarely buttock or
thigh pain
●
No postural deformity
Test Movements
●
Repeated flexion usually increases; peripheral-
izes pain
●
Pain often remains worse as a result of repeated
flexion
●
Repeated extension usually reduces, centralizes,
and abolishes pain
●
Pain usually remains better as a result of repeated
extension
16,18
Derangement 2
Clinical Presentation
●
Usually constant central or symmetrical pain,
with or without buttock or thigh pain
●
Deformity of lumbar kyphosis
E212 Spine
•
Volume 27
•
Number 8
•
2002

Test Movements
●
Repeated flexion progressively increases and pe-
ripheralizes the pain
●
Pain usually remains worse as a result of re-
peated flexion
●
Time factor is important in Derangement 2 (cor-
rection of blockage in extension requires time for a
successful reduction)
●
Repeated extension, therefore, may not be pos-
sible initially
●
Sustained positioning is attempted if a major de-
formity of kyphosis exists
●
Pain initially decreases with prone lying in flexed
position; derangement reduces gradually by in-
creasing the extension in unloaded position
16,18
Derangement 3
Clinical Presentation
●
Unilateral or asymmetrical pain, with or without
buttock or thigh pain
●
No postural deformity
Test Movements
●
Repeated flexion usually increases; peripheral-
izes pain
●
Pain may remain worse as a result of repeated
flexion
●
Repeated extension usually reduces, centralizes,
and abolishes pain; if pain does not decrease or
centralize with extension, then side-glide with ex-
tension decreases the pain
16,18
Derangement 4
Clinical Presentation
●
Usually constant unilateral or asymmetrical
pain, with or without buttock or thigh pain
●
Deformity of sciatic scoliosis (lateral shift)
Test Movements
●
Repeated flexion and extension usually increases
and peripheralizes the pain
●
Symptoms usually remain worse as a result of
sagittal movements (flexion and extension) because
of lateral shift deformity
●
Correction of lateral shift decreases and central-
izes the pain
●
If the lateral shift can be successfully corrected,
extension procedures often complete the reduction
of the hypothesized derangement
16,18
Derangement 5
Clinical Presentation
●
Unilateral or asymmetrical pain, with or without
buttock or thigh pain
●
No postural deformity
●
Leg pain extending below knee joint (constant or
intermittent sciatica)
Test Movements
●
Repeated flexion usually increases; peripheral-
izes pain
●
Symptoms may remain worse as a result of re-
peated flexion
●
Repeated extension usually decreases, central-
izes, and abolishes pain; if unsuccessful, then side-
glide or rotation techniques decrease the pain
16,18
Derangement 6
Clinical Presentation
●
Unilateral or asymmetrical pain, with or without
buttock or thigh pain
●
Leg pain extending below the knee (usually con-
stant sciatica)
●
Deformity of sciatic scoliosis (lateral shift)
Test Movements
●
Repeated flexion and extension increase or pe-
ripheralize the symptom
●
Symptoms usually remain worse as a result of
sagittal movements (flexion and extension) because
of lateral shift deformity
●
Correction of lateral shift decreases and central-
izes the pain
●
If the lateral shift can be successfully corrected,
extension procedures often complete the reduction
of the hypothesized derangement
16,18
Derangement 7
Clinical Presentation
●
Symmetrical or asymmetrical pain, with or with-
out buttock or thigh pain
●
Deformity of accentuated lordosis
Test Movements
●
Repeated extension increases and may peripher-
alize the pain
●
Symptoms remain worse as a result of repeated
extension
●
Repeated flexion decreases and centralizes the
pain
●
Symptoms remain better as a result of repeated
flexion
16,18
Other
Nerve Root Entrapment Syndrome
Clinical Presentation
●
Longstanding, constant radicular-type pain or
paraesthesias
Test Movements
●
Repeated flexion may reduce the pain tempo-
rarily, but the patient is no better as a result
●
Range increases temporarily
E213
Interexaminer Reliability of the McKenzie Method
•
Kilpikoski et al
●
Repeated extension may increase symptoms tem-
porarily, but the patient does not remain worse
after testing.
16,18
Inconclusive Mechanical Pain Pattern
Behavior of mechanical presentation, for instance move-
ment loss, in response to particular loading strategy, but
conclusion of syndrome classification is still unclear or
inconclusive.
15–18
Nonmechanical Low Back Pain
Pain not of spinal origin such as SI joint dysfunction.
16,18
References
1. Bogduk N. Musculoskeletal Pain: Toward Precision Diagnosis. Proceedings
of the 8th World Congress on Pain. Prog Pain Res Manage 1997;8:507–25.
2. Cincchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving
the paradoxes. J Clin Epidemiol 1990;43:551– 8.
3. Delitto A, Snyder-Mackler L. The diagnostic process: examples in orthopedic
physical therapy. Phys Ther 1995;75:203–11.
4. Donahue MS, Riddle DL, Sullivan MS. Intertester reliability of a modified
version of McKenzie’s lateral shift assessments obtained on patients with low
back pain. Phys Ther 1996;76:706 –16.
5. Donelson R. Reliability of the McKenzie assessment. J Orthop Sports Phys
Ther 2000;30:770 –3.
6. Donelson R, Grant W, Kamps C, et al. Pain response to sagittal end-range
spinal motion. A prospective, randomized, multicentered trial. Spine 1991;
16:S206 –12.
7. Donelson R, Murphy K, Silva G. Centralisation phenomenon: its usefulness
in evaluating and treating referred pain. Spine 1990;15:211–3.
8. Feinstein AR, Cincchetti DV. High agreement but low kappa: I. The prob-
lems of two paradoxes. J Clin Epidemiol 1990;43:543–9.
9. Fritz JM, Delitto A, Vignovic M, et al. Interrater reliability of judgements of
the centralisation phenomenon and status change during movement testing
in patients with low back pain. Arch Phys Med Rehabil 2000;81:57– 60.
10. Gjorup T. The kappa coefficient and the prevalence of a diagnosis. Methods
Inf Med 1988;27:184 – 6.
11. Jensen IB, Bodin L, Ljungqvist T, et al. Assessing the needs of patients in pain:
a matter of opinion? Spine 2000;25:2816 –23.
12. Kankaanpa¨a¨ M, Taimela S, Airaksinen O, et al. The efficacy of active reha-
bilitation in chronic low back pain. Spine 1999;24:1034 – 42.
13. Kilby J, Stigant M, Roberts A. The reliability of back pain assessment by
physiotherapists using a “Mckenzie algorithm.” Physiotherapy 1990;76:
579 – 83.
14. McCombe PF, Fairbank JCT, Cockersole BC, et al. Reproducibility of phys-
ical signs in low back pain. Spine 1989;9:908 –18.
15. McKenzie RA. The Cervical and Thoracic Spine: Mechanical Diagnosis and
Therapy. Waikanae, New Zealand: Spinal Publications, 1990.
16. McKenzie RA. The Lumbar Spine: Mechanical Diagnosis and Therapy.
Waikanae, New Zealand: Spinal Publications, 1981.
17. McKenzie RA, May S. Human Extremities: Mechanical Diagnosis and Ther-
apy. Waikanae, New Zealand: Spinal Publications, 2000.
18. Razmjou H, Kramer JF, Yamada R. Intertester reliability of the McKenzie
evaluation in assessing patients with mechanical low back pain. J Orthop
Sports Phys Ther 2000;30:368 – 83.
19. Razmjou H, Kramer JF, Yamada R, et al. Author response. J Orthop Sports
Phys Ther 2000;30:386 –9.
20. Riddle DL. Classification and low back pain: a review of the literature and
critical analysis of selected systems. Phys Ther 1998;78:708 –37.
21. Riddle DL. Invited commentary. Intertester reliability of the McKenzie eval-
uation in assessing patients with mechanical low back pain. J Orthop Sports
Phys Ther 2000;30:384 – 6.
22. Riddle DL. Reliability of the McKenzie assessment. Author response. J Or-
thop Sports Phys Ther 2000;30:773–5.
23. Riddle DL, Rothstein JM. Intertester reliability of McKenzie’s classifications
of the syndrome types present in patients with low back pain. Spine 1993;
18:1333– 44.
24. Spitzer W. Scientific approach to the assessment and management of activity-
related spinal disorders. Spine 1987;7S:S1–55.
25. Tenhula JA, Rose SJ, Delitto A. Association between direction of lateral
lumbar shift, movement tests, and side of symptoms in patients with low
back pain syndromes. Phys Ther 1990;70:480 – 6.
26. Werneke M, Hart D, Cook D. A descriptive study of the centralisation
phenomenon: a prospective analysis. Spine 1999;24:676 – 83.
Address reprint requests to
Sinikka Kilpikoski, MSc
Department of Health Sciences
University of Jyva¨skyla¨
P. O. Box 35, 40351 Jyva¨skyla¨
Finland
E-mail:sinikka.kilpikoski@kolumbus.fi
E214 Spine
•
Volume 27
•
Number 8
•
2002
Wyszukiwarka
Podobne podstrony:
(IV)A Preliminary Report on the Use of the McKenzie Protocol versus Williams Protocol in the Treatme
Association of low back pain
(IV)Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low bac
(IV)The McKenzie approach to evaluating and treating low back pain
Categorizing patients with occupational low back pain by use of the Quebec Task Force Classification
The relationship of Lumbar Flexion to disability in patients with low back pain
low back pain
low back pain 2
Serum cytokine levels in patients with chronic low back pain due to herniated disc
Treating Non Specific Chronic Low Back Pain Through the Pilates Method
(IV)The diagnostic utility of McKenzie clinical assessment for lower back pain
(IV)Relative therapeutic efficacy of the Williams and McKenzie protocols in back pain management
(IV)McKenzie method and functional training in back pain rehabilitation A brief review including res
the!st?ntury seems to hale found an interesting way of solving problems OQ5R2UJ7GCUWHEDQYXYPNT2RBNFL
03 Electrophysiology of myocardium Myocardial Mechanics Assessment of cardiac function PL
Design Guide 10 Erection Bracing of Low Rise Structural Steel Frames
więcej podobnych podstron