EUROPEAN SOCIETY FOR THERAPEUTIC RADIOL
OG
Y AND ONCOL
OG
Y
D
OMINIQUE
H
UYSKENS
R
IA
B
OGAERTS
J
AN
V
ERSTRAETE
M
ARIKA
L
ÖÖF
H
ÅKAN
N
YSTRÖM
C
LAUDIO
F
IORINO
S
ARA
B
ROGGI
N
ÚRIA
J
ORNET
M
ONTSERRAT
R
IBAS
D
AVID
I. T
HWAITES
Sponsored by
“Europe Against Cancer”
P
RACTICAL
G
UIDELINES
F
OR
T
HE
I
MPLEMENTATION
O
F
I
N
V
IVO
D
OSIMETRY
W
ITH
D
IODES
I
N
E
XTERNAL
R
ADIOTHERAPY
W
ITH
P
HOTON
B
EAMS
(E
NTRANCE
D
OSE
)
PHYSICS FOR CLINICAL RADIOTHERAPY
BOOKLET No. 5
Entrance in vivo dosimetry with diode detectors has been demonstrated to be a
valuable technique among the standard quality assurance methods used in a radio-
therapy department. Although its usefulness seems to be generally recognised, the
additional workload generated by in vivo dosimetry is one of the factors that
impedes a widespread implementation. Especially during the initial period of es-
tablishing the technique in clinical routine, the responsible QA person is con-
fronted with variable tasks, such as purchasing equipment, calibrating, defining
measurement and interpretation procedures. Often, this is accompanied by the
time-consuming activities of searching through literature and contacting expe-
rienced departments in order to gather information and define the sequence of the
steps to be undertaken.
This booklet is set up as a tool to reduce these initial efforts: it is conceived as a
step-by-step guide to implement entrance in vivo dosimetry with diodes in the
clinical routine of a radiotherapy department.
The first chapter about the preparation of the measurements contains information
(including commercial specifications) on diodes, electrometers and software.
Practical guidelines for the calibration of the diodes and the determination of cor-
rection factors are given.
The second chapter discusses the actual tasks of the responsible QA person dur-
ing the initial training period, with the emphasis on the implementation of the
measurement procedure (e.g. the training of personnel with explanation of imme-
diate actions to be undertaken in case of out-of-tolerance measurements)
In the third chapter, the interpretation of the measurement in relation to tolerance
and action levels is discussed and possible origins and consequences of out-of-tol-
erance measurements are given.
In an additional chapter, we present an overview resulting from the evaluation of
a questionnaire on how in vivo dosimetry has been implemented in different inter-
national centres. In the final chapter, elaborate contributions are given from five
centres about particular topics in in vivo dosimetry.
ISBN 90-804532-3
P
RACTICAL
G
UIDELINES
F
OR
T
HE
I
MPLEMENT
A
TION
O
F
I
N
V
IVO
D
OSIMETRY
W
ITH
D
IODES
I
N
E
XTERNAL
R
ADIOTHERAP
Y
W
ITH
P
HOTON
B
EAMS
(E
NTRANCE
D
OSE
)
TW KAFT BOOKLET 5 11-09-2001 11:46 Pagina 1

Practical guidelines for the implementation of in vivo dosimetry with
diodes in external radiotherapy with photon beams (entrance dose)
Dominique P. Huyskens, Ria Bogaerts, Jan Verstraete,
University Hospital Gasthuisberg, Department of Radiation Physics, Leuven,
Belgium
Marika Lööf, Håkan Nyström,
Rigshospitalet – The Finsen Centre, Radiation Physics Department, Copenhagen
University Hospital, Denmark
Claudio Fiorino, Sara Broggi,
Servizio di Fisica Sanitaria, Instituto Scientifico San Raffaele, Milano, Italy
Núria Jornet, Montserrat Ribas,
Servei de Radiofisica i Radioproteccio, Hospital Santa Creu i Sant Pau, Barcelona,
Spain
David I. Thwaites,
Department of Oncology Physics, Clinical Oncology, University of Edinburgh,
Western General Hospital, Edinburgh, Scotland, U.K.

2
D.P. Huyskens, R. Bogaerts, J. Verstraete, M. Lööf, H. Nyström, C. Fiorino, S. Broggi,
N. Jornet, M. Ribas, D.I. Thwaites
Practical guidelines for the implementation of in vivo dosimetry with diodes
in external radiotherapy with photon beams (entrance dose)
2001 – First edition
ISBN 90-804532-3
©2001 by the authors and ESTRO
All rights reserved.
No part of this publication may be reproduced,
stored in a retrieval system, or transmitted in any form or by any means,
electronic, mechanical, photocopying, recording or otherwise
without the prior permission of the copyright owners.

3
ESTRO
Mounierlaan 83/12 – 1200 Brussels (Belgium)

4
SUMMARY
Entrance in vivo dosimetry with diode detectors has been demonstrated to be a valuable
technique among the standard quality assurance methods used in a radiotherapy
department. Although its usefulness seems to be generally recognized, the additional
workload generated by in vivo dosimetry is one of the factors that impedes a widespread
implementation. Especially during the initial period of establishing the technique in clinical
routine, the responsible QA person is confronted with variable tasks, such as purchasing
equipment, calibrating, defining measurement and interpretatio n procedures. Often, this is
accompanied by the time -consuming activities of searching through literature and
contacting experienced departments in order to gather information and define the sequence
of the steps to be undertaken.
This booklet is set up as a tool to reduce these initial efforts: it is conceived as a step-by-
step guide to implement entrance in vivo dosimetry with diodes in the clinical routine of a
radiotherapy department.
The first chapter about the preparation of the measurements contains information
(including commercial specifications) on diodes, electrometers and software. Practical
guidelines for the calibration of the diodes and the determination of correction factors are
given.
The second chapter discusses the actual tasks of the res ponsible QA person during the
initial training period, with the emphasis on the implementation of the measurement
procedure (e.g. the training of personnel with explanation of immediate actions to be
undertaken in case of out-of-tolerance measurements)
In the third chapter, the interpretation of the measurement in relation to tolerance and
action levels is discussed and possible origins and consequences of out -of-tolerance
measurements are given.
In an additional chapter, we present an overview resulting from the evaluation of a
questionnaire on how in vivo dosimetry has been implemented in different international

5
centres. In the final chapter, elaborate contributions are given from five centres about
particular topics in in vivo dosimetry.

6
TABLE OF CONTENT
Introduction ……………………………………………………………………………….10
Chapter 1 "Getting started” ........................................................................................................13
1.1
Equipment.......................................................................................................................13
1.1.1
Diodes ......................................................................................................................13
1.1.2
Electrometer.............................................................................................................16
1.1.3
Software ...................................................................................................................16
1.1.4
Commercially available equipment .......................................................................18
1.2
Calibration procedures ..................................................................................................22
1.2.1
Validation before use .............................................................................................22
1.2.2
Calibration of the diode for entrance dose measurements ...............................23
1.2.3
Determination of correction factors .....................................................................25
1.2.4
Long term performance ..........................................................................................28
Chapter 2 Implementation o f the measurement procedure in clinical practice ....................29
2.1
Training period: initial tasks of the Responsible QA person..................................29
2.2
Defining guidelines for the persons performing the measurements ......................31
2.3
Recording of in vivo dosimetry ...................................................................................35
Chapter 3 Interpretation of the measurement...........................................................................36
3.1
Defining tolerance and action levels ..........................................................................36
3.2
Which errors can be detected?....................................................................................39
3.2.1
Malfunctioning of the quality control process ..................................................39
3.2.2
Deviations in the treatment process (dosimetric errors)...................................41
3.2.2.1
Errors in data generation and data transfer (human errors) .................................................... 41
3.2.2.2
Errors due to equipment breakdown or malfunctioning ....................................................... 44
3.2.2.3
Discrepancies in patient positioning/geometry between treatment planning and delivery ........... 45
3.3
Evaluation of in vivo dosimetry data..........................................................................45

7
3.3.1
Actions after the first measurement.....................................................................45
3.3.2
Persisting deviations: interpretation of the result .............................................46
3.3.3
Monitoring in vivo dosimetry with time ..............................................................48
Chapter 4 Techniques and procedures in different radiotherapy centres ...........................50
4.1
What equipment do you use to carry out routin e in vivo dose measurements?.50
4.2
Philosophy of your department concerning the use of in vivo dosimetry? .........53
4.2.1
When do you use in vivo dosimetry? .................................................................53
4.2.2
What d o you measure?..........................................................................................54
4.3
Procedure for in vivo dosimetry? ................................................................................57
4.3.1
Calibration procedure? Which correction factors are used? ...........................57
4.3.2
Which measured and expected doses are compared? ......................................59
4.3.3
Value of tolerance and action levels + actions undertaken..............................61
4.3.4
Time period between checks of calibration and correction factors ................65
4.4
What system do you use for the recording of in vivo dose measurements?.......66
4.5
Workload? Specific tasks of people involved?.........................................................69
4.6
Examples of practical problems?..................................................................................73
Chapter 5 Experiences from different radiotherapy centres ...................................................76
5.1
Calibration and measurement procedures – The Barcelona experience ................76
5.1.1
Tests performed before diode calibration ...........................................................76
5.1.1.1
Signal stability after irradiation...................................................................................... 78
5.1.1.2
Intrinsic precision ....................................................................................................... 78
5.1.1.3
Study of the response/dose linearity................................................................................ 78
5.1.1.4
Verification of the water equivalent depth of the measuring point.......................................... 78
5.1.1.5
Perturbation of the radiation field behind the diode ............................................................ 79
5.1.2
Diode calibration (entrance dose)........................................................................79
5.1.2.1
Field size correction factor (CF
FS
)................................................................................... 81
5.1.2.2
Tray correction factor (CF
tray
)........................................................................................ 83

8
5.1.2.3
Wedge correction factor (CF
wedge
)................................................................................... 83
5.1.2.4
SSD correction factor (CF
SSD
) ........................................................................................ 86
5.1.2.5
Angle correction factor (CF
angle
)..................................................................................... 87
5.1.2.6
Temperature correction factor (CF
temperature
) ...................................................................... 91
5.1.2.7
Influence of the dose rate on the diode’s sensitivity ........................................................... 93
5.1.2.8
sensitivity variation with accumulated dose (SVWAD) ...................................................... 94
5.2
Performance of some commercial diodes in high energy photon beams –
The Leuven experience .................................................................................................98
5.2.1
Introduction.............................................................................................................98
5.2.2
Material and Methods ...........................................................................................99
5.2.2.1
Material .................................................................................................................... 99
5.2.2.2
Methods...................................................................................................................102
5.2.3
Results ....................................................................................................................103
5.2.3.1
Independence of field size and SSD correction factors ........................................................103
5.2.3.2
Field size correction factor C
FS
without tray.....................................................................104
5.2.3.3
SSD correction factor without tray.................................................................................106
5.2.3.4
Influence of beam modifiers: tray and block correction factor C
T
and C
B
................................108
5.2.3.5
Wedge correction factors..............................................................................................109
5.2.3.6
Correction factor variation within the same batch .............................................................110
5.2.3.7
Perturbation effects .....................................................................................................110
5.2.4
Discussion .............................................................................................................111
5.2.4.1
Independence of field size and source-to-surface distance correction factors .............................111
5.2.4.2
Total build-up thickness of the diode.............................................................................111
5.2.4.3
Treatment unit dependence ..........................................................................................112
5.2.4.4
Beam modifiers .........................................................................................................113
5.2.4.5
Perturbation effects .....................................................................................................113
5.2.5
Conclusion.............................................................................................................114
9
5.3
Practical implementation of cost-effective approaches to in vivo dosimetry -
The Edinburgh experience..........................................................................................115
5.3.1
Introduction...........................................................................................................115
5.3.2
Initial physics testing and workup.....................................................................117
5.3.3
Pilot clinical studies ..............................................................................................119
5.3.4
Routine use............................................................................................................122
5.3.5
Methods to simplify routine use........................................................................125
5.3.5.1
Possible omission of correction factors ...........................................................................125
5.3.5.2
The use of build-up caps .............................................................................................126
5.3.5.3
The use of ‘generic’ correction factors ............................................................................127
5.3.5.4
Data communication and recording................................................................................128
5.3.5.5
Diode mounting and handling ......................................................................................130
5.3.5.6
Diode quality control..................................................................................................131
5.4
Large scale in vivo dosimetry implementation –
The Copenhagen experience......................................................................................132
5.4.1
Introduction...........................................................................................................132
5.4.2
Methodology ........................................................................................................132
5.4.3
Equipment..............................................................................................................133
5.4.4
Calibration procedure ...........................................................................................133
5.4.5
Correction factors .................................................................................................135
5.4.6
Tolerance levels ....................................................................................................135
5.4.7
Results and discussion........................................................................................136
5.4.8
Conclusion.............................................................................................................139
5.5
Results of systematic in vivo entrance dosimetry –
The Milano (HSR) experience ....................................................................................141
5.5.1
Materials and methods ........................................................................................141
5.5.1.1
Equipment................................................................................................................141

10
5.5.1.2
In vivo measured and expected entrance dose...................................................................141
5.5.1.3
QA chain: methods ....................................................................................................142
5.5.1.4
MU calculation/data transfer check.................................................................................144
5.5.2
Results ....................................................................................................................144
5.5.2.1
Detection of systematic errors.......................................................................................144
5.5.2.2
Systematic errors detected before in vivo dosimetry by MU calculation/data transfer check .......145
5.5.2.3
Patients with more than one check ................................................................................145
5.5.2.4
Accuracy of treatment delivery ......................................................................................145
5.5.3
Final remarks..........................................................................................................149
Appendix 1 : Literature overview.......................................................................................140
11
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the support of the EU in the framework of the program
“Europe against Cancer”. The contribution from Leuven on the performance of diodes in
high-energy beams is based on work performed for the most part by Dietmar Georg
(presently at AKH, Vienna). The contribution from Barcelona on calibration and
measurement procedures has been partially financed by FIS project 98/0047-02. We also
acknowledge the collaboration of Alain Noel (Centre Alexis Vautrin, Nancy) and Ben
Mijnheer and André Minken (Nederlands Kanker Instituut, Amsterdam).

12
INTRODUCTION
The aim of this booklet is to provide the radiotherapy community with practical guidelines
for the implementation of in vivo dosimetry (IVD) with diodes at a routin e/departmental
level.
Since in vivo dosimetry with diodes is a broad subject, considering the full map of varieties
encountered in radiotherapy, the authors have restricted themselves to guidelines for the
measurements of the entrance dose with diodes in p hoton beams. This technique of in vivo
dosimetry is the first to be considered by a radiotherapy department planning to start with
in vivo dosimetry as a routine QA method. As such, entrance diode measurements
supplement and complement basic pre -treatment QA methods, such as the independent
check of dose calculation and data transfer, which should be in routine use in the
department prior to the implementation of in vivo dosimetry.
The information contained in this booklet is a practically usable distillate from other
publications on in vivo dosimetry. The literature overview is set up as a database, which
includes, for the sake of completeness, publications dealing with exit dose measurements
and midline dose calculations, and in vivo dose measurements in electron beams. The way
in which the information is presented has rendered a booklet that is complementary to
other ESTRO booklets on in vivo dosimetry - that have appeared and will appear – and to
other review publications. These include the first ESTRO booklet on in vivo dosimetry
“Methods for in vivo dosimetry in external radiotherapy”, written by J. Van Dam and G.
Marinello
[
Van Dam 1994
]
, and a new ESTRO booklet “In vivo dosimetry in clinical
practice: When and What to measure? How to correct?”, written by E. van der Schueren,
A. Dutreix and C. Weltens [van der Schueren 2001]. A nice general review on in vivo
dosimetry was written by M. Essers and B. Mijnheer
[
Essers 1999
]
.
The latter two publications highlight the more philosophical questions concerning the use
of in vivo dosimetry. These will not be discussed here. Also, the future use of diode
measurements in relation to conformal irradiation techniques and IMRT - for which point
dose verification is obviously inadequate – is a topic outside the scope of this work.
13
CHAPTER 1 "GETTING STARTED”
1.1 EQUIPMENT
1.1.1 DIODES
Semiconductor diodes, when connected to a suitable electrometer, offer the unique
combination of high sensitivity, immediate readout, simplicity of operation (no external bias
voltage), small size and robustness.
Silicon diodes can be made starting from either n-type or p-type silicon, which behave
differently because their minority carriers are holes or electrons, respectively. Figure 1.1
illustrates the basic operation of a p-type silicon detector diode. In the boundary between
two regions, one of p-type and another of n -type silicon, there is a depletion of free charge
carriers. When the detector is operating with zero external voltage a potential difference of
about 0.7 V exists over this depletion area, causing the charge carriers created by the
radiation to be swept away into the body of the crystal. As the diode is asymmetrically
doped - the n-type region is much more heavily doped than the p-type region - the
irradiation induced charge flow is comprised almost entirely of electrons (holes in an n -type
diode). Due to defects in the crystal lattice some electrons are trapped and will
consequently not contribute to the diode signal. An n-type diode is more influenced by
these recombinations as holes are more easily trapped than electrons.
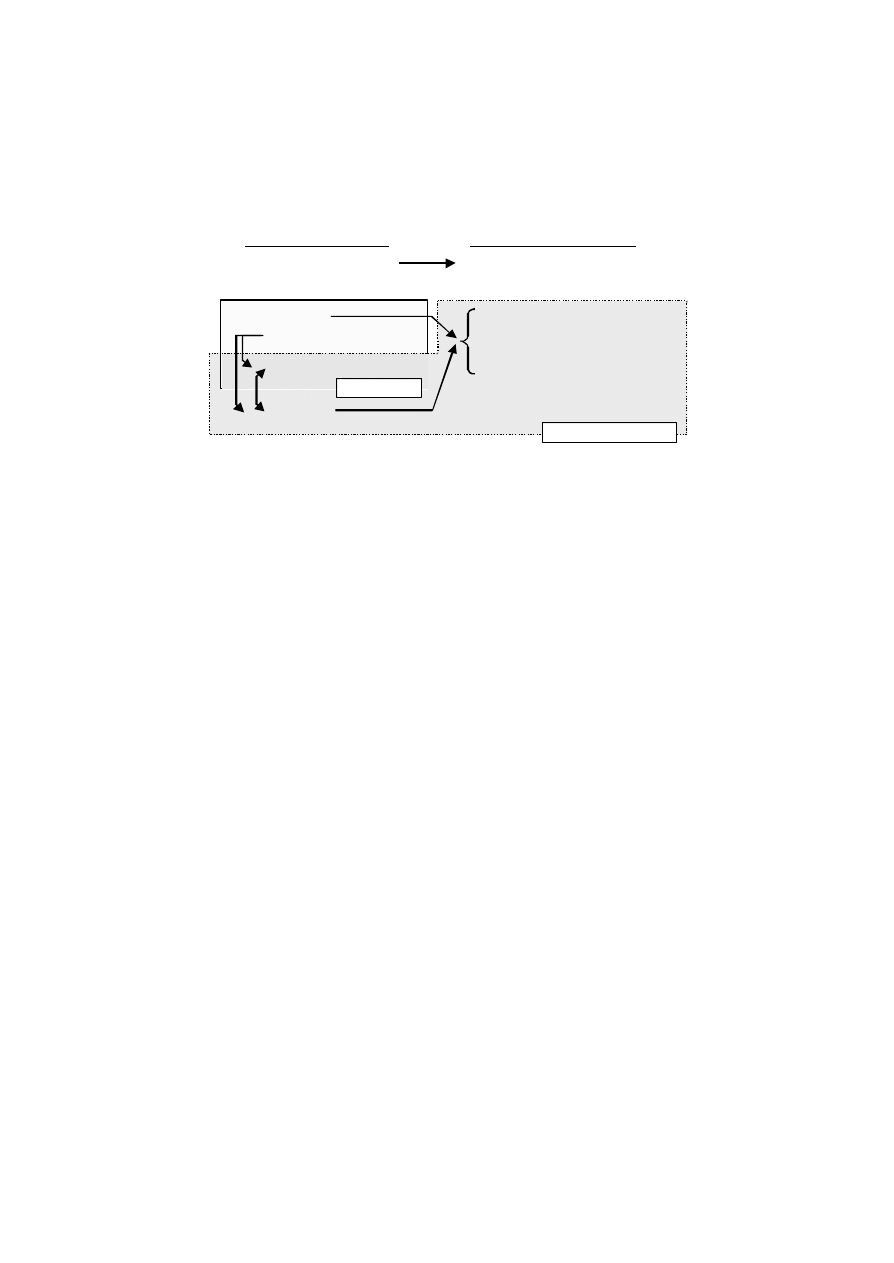
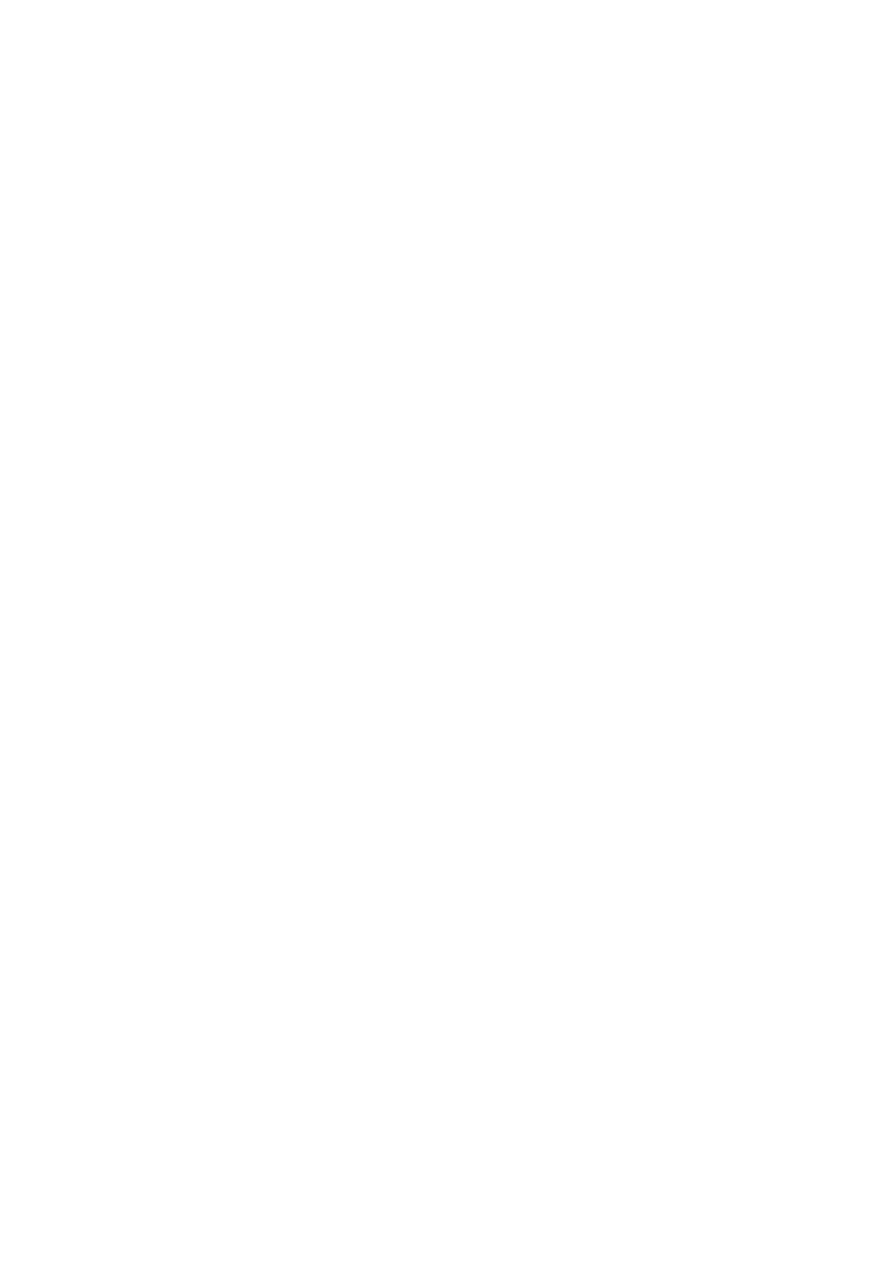
Figure 1.1 Schematic overview of the basic principal of a p-type silicon diode used
as a radiation detector.
depletion layer
p-type
+
+
+
+
+
+
+
+
+
+
+
+
+
+
+
+
-
+
+
+
-
+
+
+
+
-
+
+
+
+
+
+
+
-
+
+
+
+
+
+
+
+
+
-
+
+
+
+ +
+
+
+
+
+
+
+
+
+
+
+
+
+
-
+
+
-
+
-
+
+
+
+
+
+
+
-
+
+ +
+
-
-
-
-
+
-
-
-
-
-
+
-
- +
-
-
n-type
I
e
-
-
-
-
-
-
-
-
-
-
+
+
+
+
+
+
+
+
+
+
+
+
+
electrostatic potential ~ 0.7 V
14
The detector sensit ivity depends on the lifetime of the charge carriers and consequently on
the amount of recombination centres in the crystal, which is determined by the diode type,
the doping level and the accumulated dose. As the radiation induces recombination
centres within the lattice, the sensitivity will decrease with accumulated dose.
Figure 1.2 Schematic summary of the factors (physical as well as geometrical)
influencing the diode signal. Arrows indicate dependencies of one factor on
another. The different influences are taken into account in calibration and
correction factors (see Section 1.2).
The effect of radiation damage represents the main limitation of silicon diodes.
Furthermore, other effects related to the detector material have to be considered (Figure
1.2):
•
The diode signal depends on the photon energy. This is due to the higher atomic
number of silicon (Z = 14) compared to soft tissue (Z =
∼
7) and the corresponding
higher contribution to the diode signal from the photo-electric effect.
•
The diode signal is dose rate dependent. At high instantaneous dose rates the
recombination centres will be “occupied” resulting in a rela tively lower rate of
recombination. This leads to a proportionally higher response at higher dose rates. This
effect is more pronounced for n-type Si-diode detectors than for those made of highly
CALIBRATION
CORRECTION FACTORS
physical dependencies
geometrical dependencies
related to detector material
+ related to measurement methodology
+ related to build-up cap design/thickness
energy
field size
accumulated dose
SSD
tray, blocks
temperature
wedge
dose rate
orientation

15
doped p-type Si [Heukelom 1991b]. The dose rate dependence may change with
accumulated dose due to radiation damage.
•
The diode signal is influenced by temperature. In general, the sensitivity increases with
increasing temperature. This effect is less pronounced for an un-irradiated diode and
will increase with accumulated dose. However, the rate of change of sensitivity with
temperature tends to stabilise as accumulated dose increases [Grusell 1986].
Due to these dependencies, the “true” entrance dose dependence on geometric
parameters, as SSD (source skin distance), field size, and the presence of wedges, trays and
blocks, will be incorrectly reflected by the diode signal variation. For this reason, correction
factors have to be determined (see Section 1.2.3 describing t he practical details). Beside the
physical properties of the diode crystal, other factors contribute to the magnitude of these
correction factors (Figure 1.2). First, there is the inevitable fact that the measureme nts are
performed with the diode located outside the patient or the phantom. The photon scatter
conditions experienced by the diode are therefore different from those at the point of
entrance dose definition, i.e. at the depth of dose maximum inside the patient or the
phantom. For instance in high energy beams the diode reading is nearly independent of
phantom scatter, while the entrance dose is clearly not (see [Jornet 2000], [Lööf 2001],
[Wierzbicki 1998]). In addition, the diode may experience a different amount of head-scatter
electrons. As a consequence, the effect of field size, SSD, and presence of wedges, trays
and blocks on the contaminating head-scatter electron contribution may induce large
variations in the diode correction factors (see Section 5.2).
In relation to this, the construction of the detector, for instance the thickness and the
shape of the build -up cap, is another factor influencing the diode signal. The shape of the
build-up cap will influence the angular response: a cylindrical cap has a different angular
dependence than a hemi -spherical one. The thickness of the build -up cap determines the
scatter conditions seen by the diode. To minimise the correction factors and ensure a
greater accuracy in the measurements, it is preferable to have a (possibly in house made)

16
build-up cap with a thickness equal to the depth of maximum dose (see Sections 5.2 and
5.3). On the other hand, it should be kept in mind that a thick build -up cap means a larger
perturbation of the treatment field and may jeopardise the dose to the patient if
measurements are performed during many fractions of the treatment course. In addition, if
the same diode is used for different beam qualities (for instance 6 MV and 18 MV), it may
be preferable to use the same build -up cap for both, in order to avoid confusion and
interchange of build -up caps. It follows therefore that the choice of the "optimal" diode
design is a question of each department’s policy for the in vivo dosimetry procedure.
1.1.2 ELECTROMETER
The diode should be connected to a dedicated electrometer with a low input impedance
and low offset voltage. Diode current generated by sources others than radiation is
considered to be leakage current and is not desirable. The leakage current ideally should be
zero. Due to the input offset voltage of the amplifier, however, there is always a small bias
across the diode introducing a small leakage current. An electrometer used together with a
diode requires therefore the offset voltage of the amplifier to be low, 10
µ
V or less. The
leakage current increases with temperature and accumulated dose due to defects in the
diode and it is essential that the electrometer has adequate zero drift compensation and
stabilisation.
1.1.3 SOFTWARE
There is a range of electrometers available for in vivo dosimetry, having greater or lesser
degree of sophistication. The simplest type of electrometer provides 5 to 10 chann els with
manual adjustment of the input offset and gain for each channel. This type of electrometer
may allow only one gain setting for each channel while more sophisticated ones offer
several separate calibration sets and correction sets with automatic calculation, storage of
factors and zero drift compensations. Thus one detector may be calibrated to be used in

17
several different irradiation conditions. Most of the electrometers offer the possibility to
use interface software designed to run in a Windows environment in conjunction with
commercial available software or in house made programs loaded onto a personal
computer.
More advanced systems are incorporated with the department’s verification system,
simplifying the management of the in vivo dosimetry procedure. Such system provides the
possibility to store all calibration and correction factors for every diode in use. The
measured diode signal is then automatically converted to dose using the treatment field
parameters downloaded from the patient’s data in the verification system. This gives an
immediate "on line" check of the preparation and treatment delivery in the radiotherapy
process, thereby reducing the incidence of errors.
CONSIDERATIONS WHEN CHOOSING EQUIPMENT
•
Pre-irradiated diodes have in general lower sensitivity. This parameter has to be taken
into account when choosing the electrometer, which must have a sensitivity range that
matches the diode. The manufacturer of the detectors usually also supplies adequate
electrometers.
•
The diodes are available in negative and positive polarity and the electrometer has to
be adapted to this.
•
The rate of sensitivity degradation will affect the required calibration frequency. In
general, n-type diodes have larger sensitivity degradation but the rate of degra dation
will decrease after a certain amount of pre -irradiation (both for n- a n d p-type).
Therefore, the pre -irradiation level is of interest and should be stated by the
manufacturer.
•
The best choice of diode design i.e. shape and thickness of the build -up cap depends
on the application. A cylindrical cap (uniform directional response around the detector
axis) is preferable in measurements in tangential treatment techniques while in entrance
dose measurements with perpendicular incident beams a hemi -spherical is a better
18
choice (smaller perturbation than the cylindrical cap). If little influence on the
perturbation of the treatment field is desired (measurements in all sessions) a diode with
thin build-up cap is preferable. This however means that larger correction factors have
to be used for accurate measurements, whereas diodes with thicker caps need smaller
correction factors at the expense of larger perturbation.
•
A number of properties of importance for the clinical use of diodes are related to their
dose rate dependence. If diodes are to be used in irradiation situations with large
variations of dose per pulse i.e. wedged fields or treatments at SSD deviating from
calibration SSD, it is advisable to choose diodes with a low dose per pulse dependence,
usually high doped p -type diode detectors.
1.1.4 COMMERCIALLY AVAILABLE EQUIPMENT
There are several different types of diodes commercially available having various
properties with regard to pre -irradiation level, doping type, design and thickness of build -
up cap to accommodate a large photon energy range. For accurate in vivo dosimetry it is
essential that each diode characteristic is well understood in order to utilise it properly and
efficiently. Unfortunately though, manufacturer’s specifications can sometimes be difficult
to interpret. Some specifications should be handled with caution: for instance, it is known
that several commercial diodes lack sufficient build -up for the energy range that they are
specified for (see [Jornet 1996], [Georg 1999] and [Meijer 2001]).
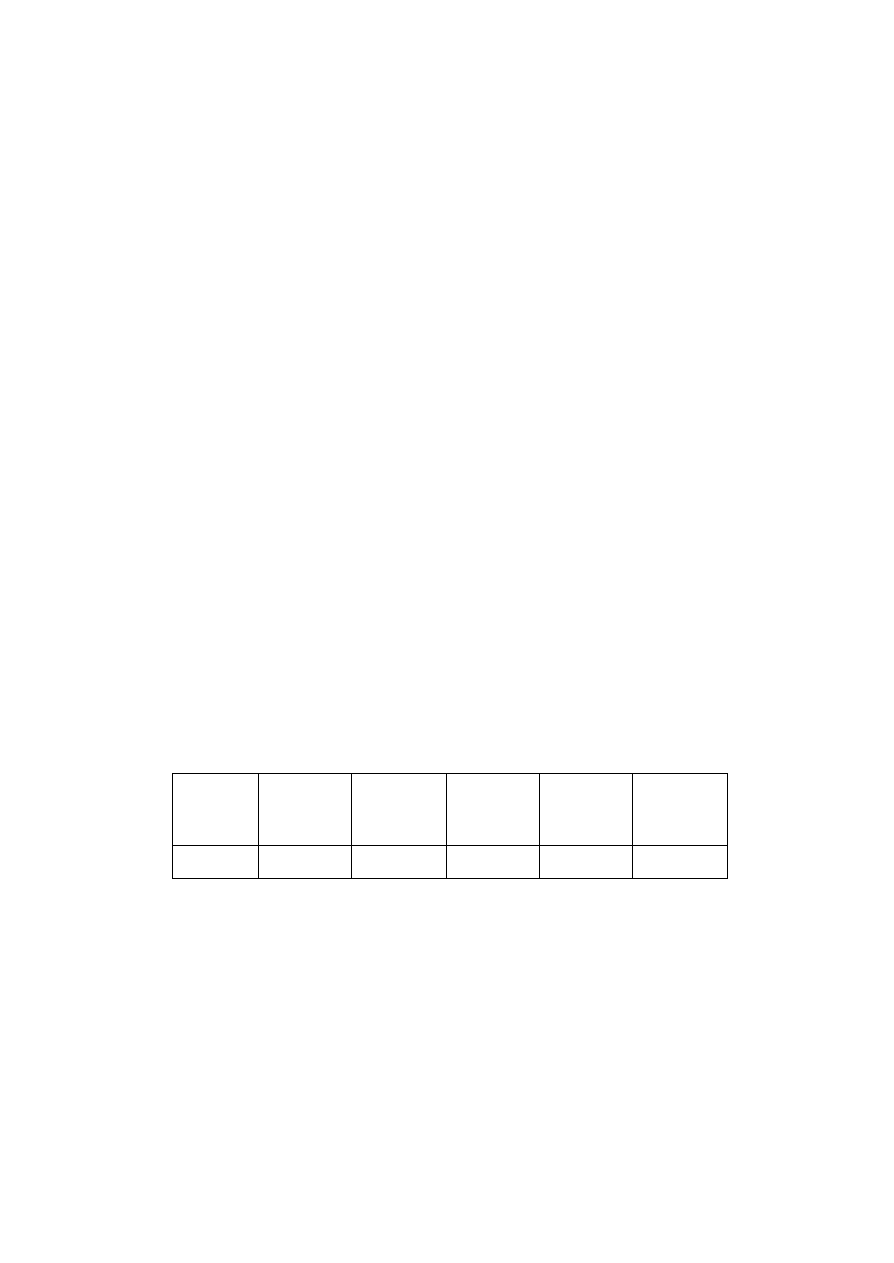
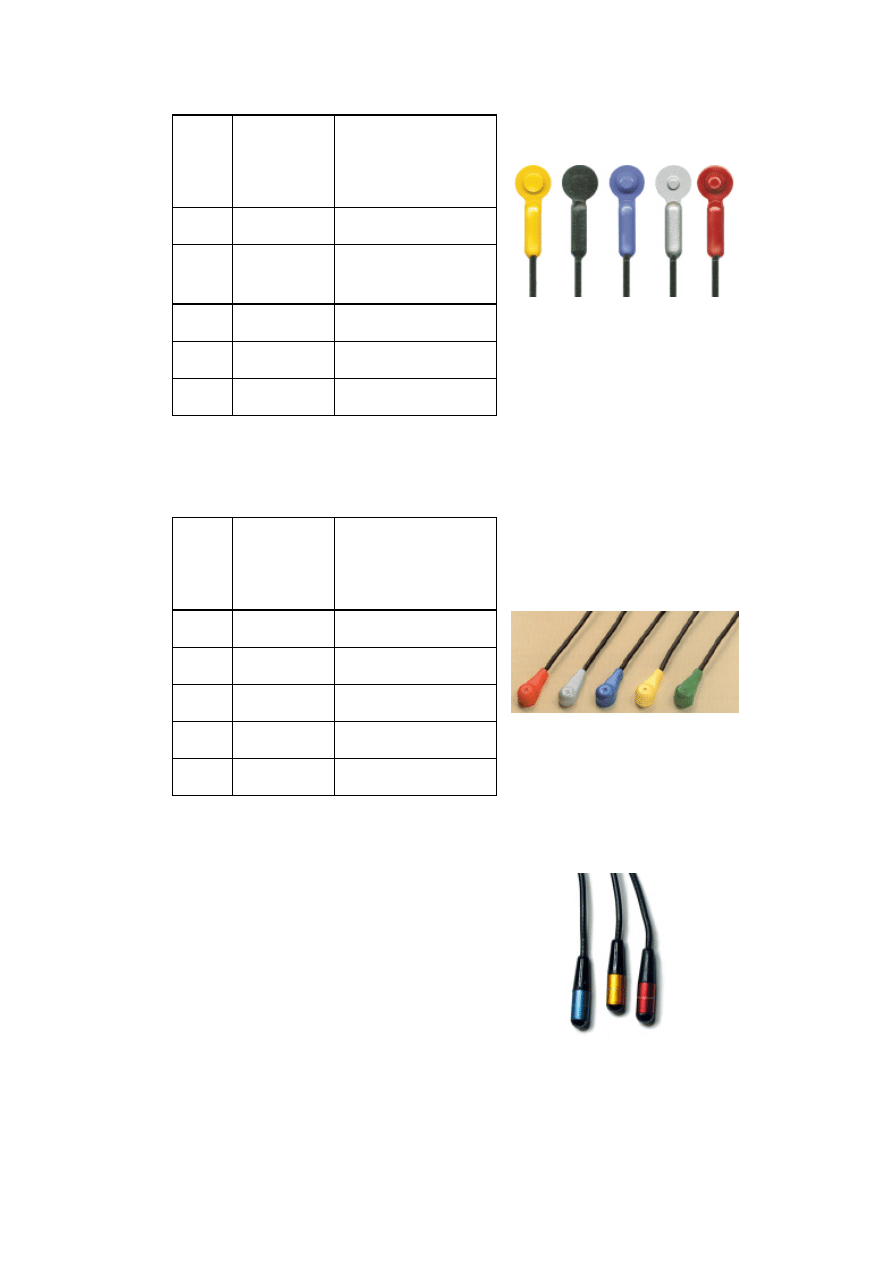
Table 1.1 to Table 1.6 present diodes and selected specifications available from leading
companies.
Company
Scanditronix
Medical AB
EDP diodes
Sun Nuclear
Corporation
QED diodes
Precitron MDS
Nordion AB
P diodes
Nuclear
Associates
VeriDose diodes
Sun Nuclear
Corporation
Isorad-p diodes
Type
p-type
p-type
n-type
n-type
p-type
19
Sensitivity
[nC/Gy]
40
40
150-300
150
40
Sensitivity
degradation
[% / kGy]
1
< 1.5 - 10 MeV
< 1.5 - 18 MV
0.1 at 6 MV
< 15 %
after 10 kGy
1 at 10 MeV
0.1 at 6 MV
Sensitivity
degradation
with
temperature
[% /
°
C]
0.4
0.3
0.1 - 0.3
< 0.5
0.3
Pre irradiation
level
8 kGy at 10
MeV
10 kGy at 10
MeV
25 kGy
10 kGy at 10
MeV
Linearity
(Dose per
pulse
dependence)
< 1%
in the range
of
0.1 - 0.6 mGy
per pulse
SSD
dependence
±
2% for
18MV
±
1% for 8MV
at SSD 80-130
cm for a
typical
accelerator
< 1% of SSD
<
±
1% for
6 and 18MV
at SSD 80-130
cm for a
typical
accelerator
Output
polarity
Negative
Negative or
positive
Negative
Negative or
positive
Negative or
positive
Table 1.1 Commercially available diodes listed along with the specifications given by
the manufacturers.
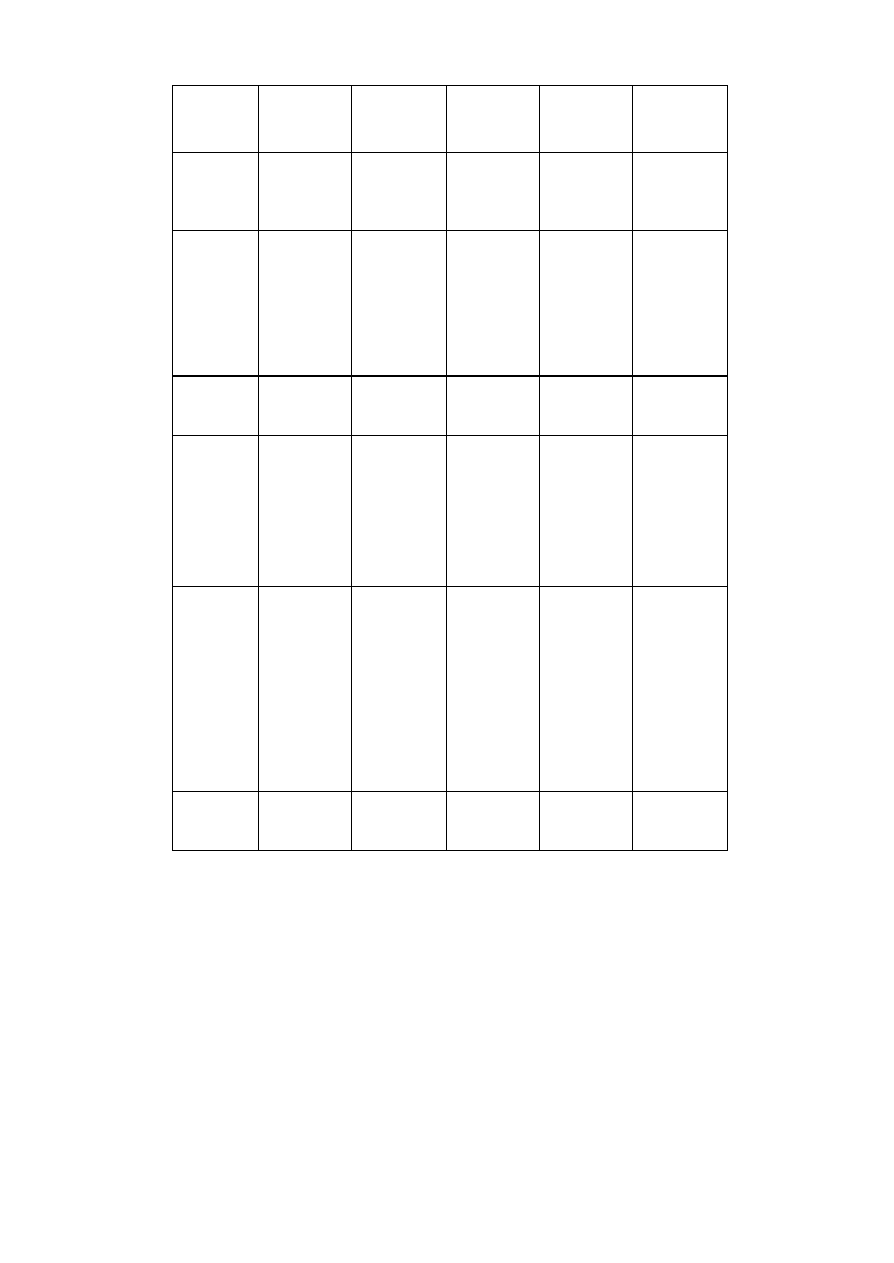
20
Model
Application /
Energy range
Build-up cap /
Water equivalent build -
up
E5
60
Co
5 mm
P10
4 - 8 MV
10 mm
P20
8 -16 MV
20 mm
P30
16 - 22 MV
tungsten / 30 mm
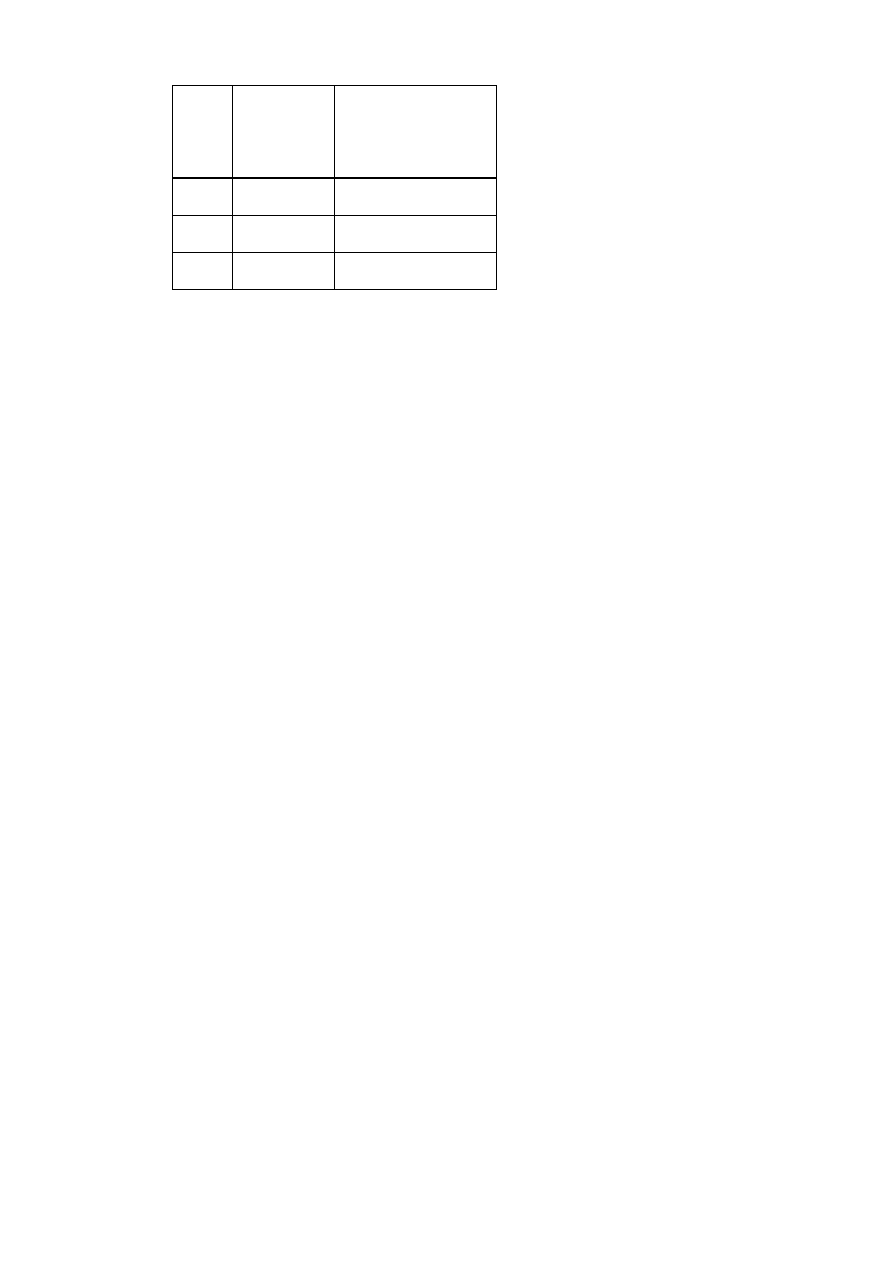
Table 1.2 Precitron–Helax, P-diodes
Model
Application /
Energy range
Build-up cap /
Water equivalent build -
up
EDD-2
Entrance / Exit
Electrons
paint / 2mm
EDD-5
Risk organ
monitoring
60
Co
polystyrene / 4.5 mm
EDP- 0
Skin dose
None
EDP-10
4 - 8 MV
stainless steel / 10 mm
EDP-15
6 -12 MV
stainless steel / 15 mm
EDP-20
8 -16 MV
stainless steel / 20 mm
EDP-30
16 - 25 MV
tantalum / 30 mm*
*less than 30 mm [Jornet 1996], [Meijer 2001]
Table 1.3 Scanditronix Medical AB, EDP diodes
21
Model
Application /
Energy range
Build-up cap /
Water equivalent build -
up
1112
Electron
acrylic
1113
Skin dose /
Scatter dose
none
1114
1 -4 MV
aluminium / 10 mm
1115
6 -12 MV
brass / 18.5 mm
1116
15 -25 MV
brass / 30.4 mm
Table 1.4 Sun Nuclear Corporation, QED diodes
Model
Application /
Energy range
Build-up cap /
Water equivalent build -
up
30-475
6 – 25 MeV
30-471
1 – 4 MV
copper / 7 mm
30-472
5 – 11 MV
copper / 14 mm
30-473
12 –17 MV
tungsten / 26 mm
30-474
18 - 25 MV
tungsten / 36 mm
Table 1.5 Nuclear Associates, VeriDose diodes
22
Model
Application /
Energy range
Build-up cap /
Water equivalent build -
up
1162
1 - 4 MV
aluminium / 10 mm
1163
6 -12 MV
brass / 18.5 mm
1164
15 - 25 MV
tungsten / 30.4 mm
Table 1.6 Sun Nuclear, Isorad-p diodes.
1.2 CALIBRATION PROCEDUR ES
1.2.1 VALIDATION BEFORE US E
The signal stability of the diode, influenced e.g. by the leakage current without irradiation,
should be checked after adequate warm-up time with the diode connected to the
electrometer and compensated. Compared to the current obtained for the real measurement,
the leakage current should be insignificant. It is advisable to measure the leakage curr ent
for a time period that is at least five times longer than the time period used in the clinical
application. The leakage current should not exceed 1% in one hour
[
Van Dam 1994
]
.
A general test of the reliability and stability of the equipment, before using it in clinical
routine, can be performed as follows. The diode positioned on top of a calibration phantom
(see Section 1.2.2) is irradiated for 10 to 15 times with the same reference field. The standard
deviation of the resulting signals should be within 0.5 %. The measurements are repeated
on different days during two weeks. The measurement procedure, including the
measurement equipment, the phantom set-up and diode positioning, is reliable and stable,
if all measurements are within 1 % (provided that the beam output of the treatment unit is
stable).
23
Some centres perform more extensive tests before using the diode, for instance a
measurement of the effective water equivalent thickness of the build -up cap. An example of
this can be found in Section 5.1.
1.2.2 CALIBRATION OF THE DIODE FOR ENTRANCE DOSE MEASUREMENTS
The diode is calibrated to measure the entrance dose, i.e. when positioned on the skin of
the patient the measured dose should correspond to the dose to tissue at the depth of
maximum dose of the photon quality in use for a particular beam geometry.
The calibration procedure firstly involves the determination of the calibration factor (F
cal
).
It is recommended to calibrate the diode for each beam quality with which it is intended to
be used (see Figure 1.2). Due to the variation of the diode signal with accumulated dose,
calibration should be regularly repeated in time. Time intervals typically vary between
weekly and monthly. The temperature dependence of the diode signal can be accounted for
during calibration, if this is performed at the same temperature as the measurements with
that particular diode in the clinical application. Usually, however, a temperature correction
factor will be determined (see Section 1.2.3).
The entrance dose value in a clinical situation is calculated from the diode measurement as
the product of the diode reading, the calibration factor and the correction factors (equation
1). The calibration factor is defined as the ratio of the ion chamber dose and the diode
reading measured in the reference geometry (equation 2).
∏
⋅
⋅
=
i
cal
diode
entr
entr
CF
F
R
D
,
(1)
condition
ref
diode
ic
cal
R
D
F
.
=
(2)
24
The diode may be calibrated against the dose monitor chamber of the accelerator or against
a secondary reference chamber. To determine the calibration factor, the diode is positioned
on the surface of a suitable (plastic) calibration phantom (e.g. made of polystyrene). The
ion chamber is inside the phantom on the central axis, at reference depth. According to the
definition of entrance dose, this should be the depth of maximum dose, as indicated in
Figure 1.3. The ion chamber is thus probing the depth dose curve at its maximum, and not
at its subsequent fall-off. As a consequence, if the protocol that is used for absolute dose
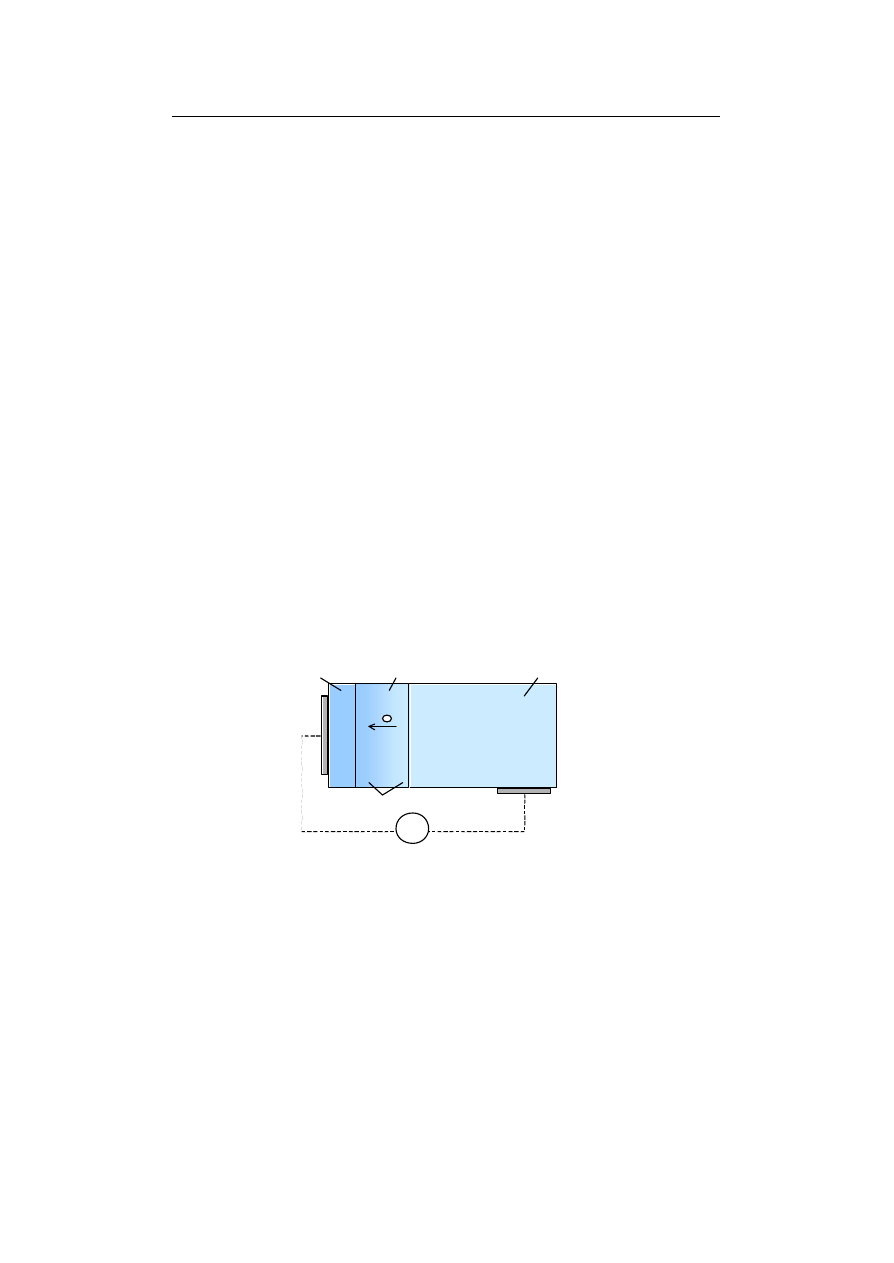
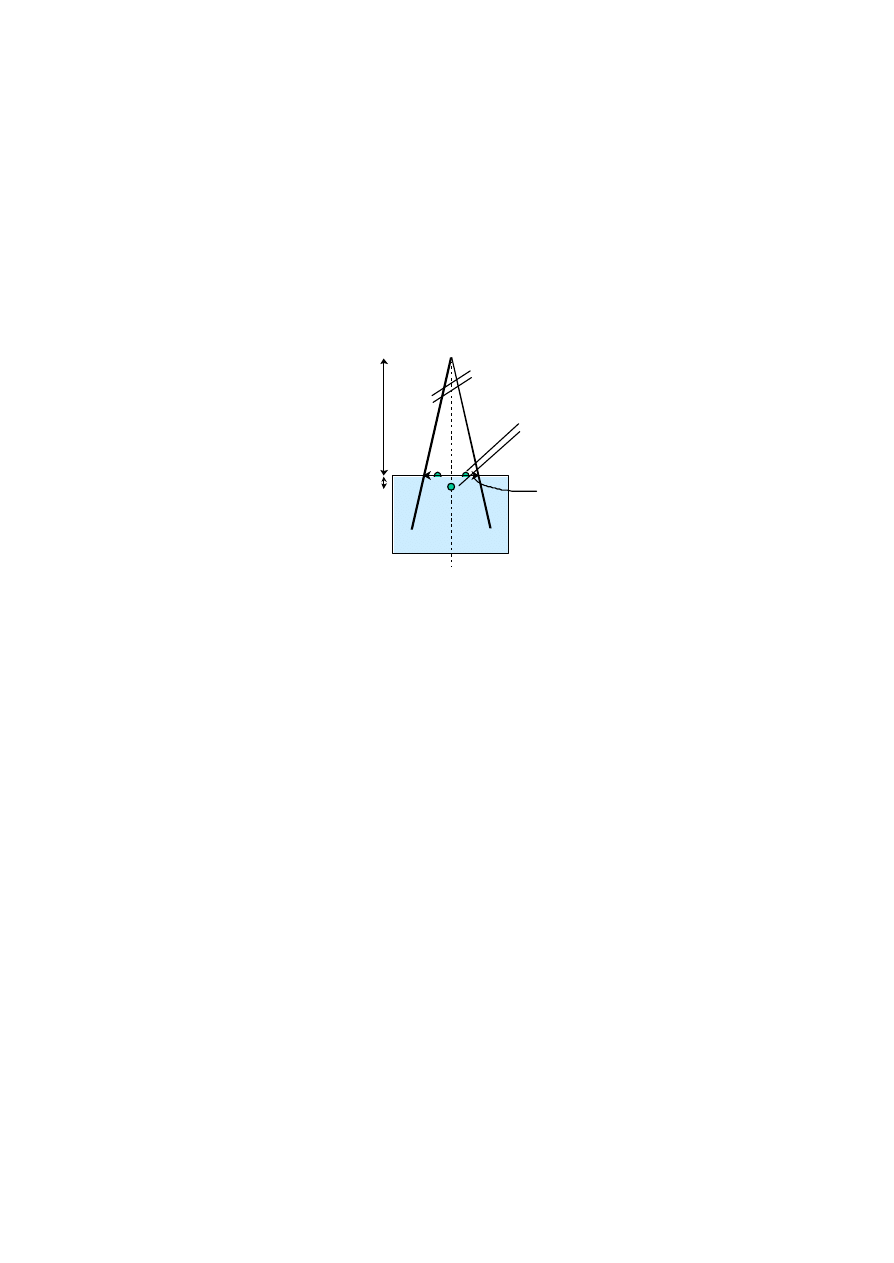
Figure 1.3 Diode calibration procedure for entrance dose measurements. The ionisation
chamber is positioned at the reference depth in the phantom and the diode at
the entrance surface in the reference geometry.
Depth of d
max
SSD
Reference distance
Diode
Ion chamber
Solid phantom
Reference field size

25
determination with the ionisation chamber includes the application of a displacement
factor, this factor should be omitted. If a plastic phantom is used that is not completely
water-equivelant (for instance made of polystyrene), a conversion factor dose to p lastic –
dose-to-water should be employed. The reference SSD is usually 100 cm (for linacs) and
the reference field 10 x 10 cm
2
.
The calibration may be performed with one or several diodes placed in a circle around the
central axis provided that variations in the field flatness are insignificant. Field flatness at
d
max
should therefore be checked, for instance by measuring the ratio of diode readings at
the circle and at the centre of the field. Furthermore, the diodes should be placed at a
distance from the central axis to avoid perturbation of the beam at the reference chamber.
1.2.3 DETERMINATION OF CORRECTION FACTORS
Subsequent to the determination of the calibration factor, a set of correction factors has to
be established to account for variations in diode response in situations deviating from the
reference conditions (see Figure 1.2). The ultimate factors influencing the diode response
are the field size, source-to-skin distance, presence of beam modifiers such as filters or
wedges, presence of tray and blocks and the beam incident angle (equation 3). As
described in Section 1.1.1, the dependence of the diode signal on most of these factors is
not only arising from the intrinsic properties of the diode crystal, but also from elementary
beam physics, i.e. the fact that the detector experiences different scatter contributions than
the ones experienced at the depth of maximum dose. As a consequence, most of the
correction factors are inherent to the use of dose detectors taped to the patient’s skin, and
should also be applied e.g. for thermoluminescent dosimeters (TLDs).
The temperature dependence, intrinsic to diodes, should be accounted if a particular diode
is used at different temperatures. This may be done by applying a constant temperature
correction factor or by using a thermostatically controlled calibration phantom. However, if
the patient measurement is assessed before the diode has reached thermal equilibrium (2 -3
minutes) the influence of temperature dependence may be neglected (see Sections 5.3.3
26
and 5.5.1). Diodes used for TBI, for which the low dose rate is achieved by enlarging the
SSD, should be calibrated in TBI conditions.
Correction factors accounting for the variations in response are determined as the ratio of
the reading of an ionisation chamber and the reading of the diode for a clinical irradiation
situation normalised to the same ratio for the refe rence situation (equation 4):
angle
block
tray
wedge
SSD
FS
i
CF
,
CF
,
CF
,
CF
,
CF
,
CF
CF
=
(3)
condition
.
ref
diode
ic
condition
clinical
diode
ic
)
R
/
R
(
)
R
/
R
(
CF
=
(4)
The reference conditions are as stated in Section 1.2.2. However, if the value of a particular
parameter (for instance the field size) influences the value of the correction factor for a
second parameter (e.g. the presence of a tray), the ‘reference condition’ for the
determination of this second correction factor is adapted in order to avoid double inclusion
of the first correction factor. This is made clear in the practical recommendations given
below. These may be modified/simplified according to the type of diode (and previous
experience with that particular type of diode), the clinical application, and the beam quality
in use:
•
The variation in response due to different beam incident angles is measured for
different gantry and couch angles and normalised to the response measured when the
central beam axis and the symmetry axis coincide.
•
Field size correction factors are measured for square fields ranging e.g. from 5 x 5 cm
2
to
40 x 40 cm
2
, at the reference SSD of 100 cm.
•
SSD correction factors are measured for SSDs within a range determined by local
clinical conditions, for instance from 75 cm to 110 cm, at the reference field of 10 x 10
cm
2
. Note that SSD correction factors and field size correction factors are assumed to be
independent. This is not always the case for high energies (see remark below and
[Georg 1999]).

27
•
Wedge correction factors may depend on the field size. They are measured at reference
SSD, for different square fields (e.g. fields with 5 cm, 10 cm and 20 cm side length). The
ratio of the signal of the ionisation chamber to the diode signal is in this case
normalised to the same ratio for the open beam (with the same field size).
•
Tray correction factors may depend on SSD and field size. They can be determined by
repeating all measurements carried out for the SSD and field size correction factors, and
normalising the data to the reference situation of an open beam with the appropriate
SSD and field size.
•
Block correction factors can be measured for different blocks defining square fields at a
fixed collimator opening (for instance a collimator opening of 20 x 20 cm
2
for blocks
defining fields of 5 x 5 cm
2
, 10 x 10 cm
2
and 15 x 15 cm
2
). The reference condition is again
the corresponding open beam (with the same collimator opening).
Practical examples of calibration procedures and typical values of correctio n factors for
particular types of diodes are given in Section 5.1. In order to minimise redundant use of
correction factors, minimum values can be set below which factors are discarded (for
instance if a correction factor deviates less than 1 % from 1, the correction is within the
measurement uncertainty). Other ways of limiting the use of correction factors are
described in Section 5.3.5.
If the dosimetric characteristics of a diode are not (well) known, it is recommended to check
its response extensively at different irradiation conditions to establish the range where no
correction factors are needed. As the type of diode is a major determinant of the magnitude
and the behaviour of most of the correction factors, diodes of the same type will require
similar correction factors, showing similar tendencies. However, when a high accuracy is
required, it is advisable to check also the correction factors for every individua l diode.
Correction factors associated with increased diode sensitivity due to variation in beam
energy spectrum are of major importance in high-energy photon beams, especially if diodes
with a thin build -up cap are used. One should also bear in mind that, for insufficient build -
28
up, other interdependencies of correction factors than the ones mentioned above may exist
[Georg 1999]. In practice, one can start by considering all correction factors to be
independent and then check the accuracy of the measured d ose when changing more than
one reference condition at the same time (i.e. field size, SSD and wedge). Useful information
about the performance of diodes in high-energy beams is given in Section 5.2.
1.2.4 LONG TERM PERFORMANCE
It is good practice to keep a record of the change in the calibration factor in order to
estimate how often re -calibration will be required to achieve a certain accuracy. As the
sensitivity degradation may vary with different beam qualities this is especially important
when diodes are used in various beam qualities. It is advisable to start with weekly
calibrations and to adjust the calibration interval after having monitored the accumulated
dose in between calibrations and the corresponding change in calibration factor for a while.
Depending on the diode type in use the correction factors associated with the dose per
pulse dependence may also change with time due to the accumulated dose. A quick and
efficient test of the long-term stability is to perform a linearity check by measuring the
diode response normalised to an ionisation chamber at two different SSDs. If the ratio is as
expected, the diode is working accurately and the correction factors are still valid. The
change of the temperature dependence with time is accounted for if the diode is calibrated
at the same temperature as the measurements in the clinical application.

29
CHAPTER 2 IMPLEMENTATION OF THE MEASUREMENT
PROCEDURE IN CLINICAL PRACTICE
Regarding the workload associated with routine in viv o dose measurements, two
categories of work can be distinguished: the calibration procedures and the actual patient
measurement procedures. Depending on the strategy of the radiotherapy department, these
procedures can either be carried out by a small team of qualified personnel, or assigned to
different groups of personnel within the department (for instance calibration procedures
are carried out by a dosimetrist/physicist; patient measurements are performed by the
radiographers/nurses at the treatment units). In the latter case, one person or a small group
of persons have the responsibility for the in vivo dosimetry program and train the others.
2.1 TRAINING PERIOD: INITIAL TASKS OF THE RESPONSIBLE QA PERSON
The person(s) responsible for the in vivo dosimetry program initiates the implementation of
it. First, he/she gets acquainted with the theoretical background of in vivo dosimetry,
available in literature (see appendix), with the equipment used in the department
(electrometer and diodes) and with the calibration techniques using the (plastic) calibration
phantom. The test of the reliability and stability of the equipment (see Section 1.2.1) is
performed. After the reliability test, the electrometer is calibrated following the instructions
in the manual, and the calibration and correction factors of the diodes are determined as
prescribed in Section 1.2.
Another task is the practical training for the personnel performing the measurements. The
importance of the accurate positioning of the diode in the centre of the treatment field is
emphasised. A demonstration is given by performing 10 irradiations with a wedge, e.g. 30°,
for which the positioning of the diode is critical. Between each irradiation the diode is
removed and repositioned. The readings of the electrometer should be within 1.5 %.

30
If the beam axis of the treatment field is covered by a shielding block or in case of an
asymmetric field, the penumbra region should be avoided by positioning the diode as close
as possible to the field centre and at a similar SSD. If it is a wedged field, the actual
attenuation of the wedge at the off-axis position of the diode should also be considered.
Before starting patient measurements, it is useful to simulate some patient set-ups with a
phantom. The irradiations and diode measurements are performed in identical conditions as
in the clinical situation. The expected signal is calculated, either with an independent
formula or with a treatment planning system (TPS) able to calculate dose at d
max
. The
difference between the calculated and the measured signal should not exceed 1 %. These
patient simulations are an excellent test for the whole measuring procedure: calibration of
the dio de and determination of correction factors, calculation of the expected dose, and
diode positioning.
Patient measurements should be started for treatment fields where easy fixation of the
diode in the field centre is possible, for instance mediastinal or large head and neck fields
without wedge. When the deviations between measured and expected signal are smaller
than 3% to 5%, measurements for other treatments like breast or pelvic irradiations can be
initiated.
In the course of the training period, tolerance and/or action levels have to be established.
Since a measurement result out of the tolerance window triggers the chain of measurement
interpretation, determination of the values of these levels is discussed in more detail as a
first item in Chapter 3. The adequacy of tolerance/action levels should be examined
regularly (see Section 3.1), and especially during the training period. In this period it is also
useful to keep track of other parameters:
•
the precision of a single measurement: this can be done by performing repetitive
measurements on the same patient during consecutive sessions (at least 5). The mean

31
value, the standard deviation and the deviation of each individual measurement are
evaluated. A small standard deviation is a strong argument for considering the value of
the first measurement as being representative for the whole treatment. This evaluation
should be made for different groups of patients and t reatments.
•
the calibration and correction factors (see Section 1.2.4).
2.2 DEFINING GUIDELINES FOR THE PERSONS PERFORMING THE
MEASUREMENTS
It is essential to define departmental guidelines and/or procedures describing
the
immediate actions to be taken when the measured entrance dose is out of the tolerance
and/or action levels. These guidelines will differ among the radiotherapy departments
depending on the choice of the general philosophy for in vivo dosimetry (which patients,
which fraction, which treatment sites etc.), the education level of radiation technologists,
the existence of a Quality Assurance group and/or the involvement of the physics
department.
Practical guidelines towards the radiation technologists, assuming that they are in charge
of these in vivo measurements, should provide an answer to the following questions:
•
if the measured entrance dose exceeds the tolerance or action levels, what
should be done (perform a new measurement, call the QA group/physicist, ...)?
•
if there is a difference between the stated SSD and the actual SDD (source-diode
distance), what should be done i) for isocentric techniques or ii) when using bolus or
immobilisation devices (correct for inverse square law, ... )?
Other questions regarding staffing and management of personnel should also be clarified:
•
who is the contact person for measurements out of tolerance or action levels?
•
if a second measurement is requested, should it be performed in the presence of a
physicist?
32
•
who will perform phantom measurements, if needed?
•
who is in charge of the calibration and the determination of correction factors of the
diodes?
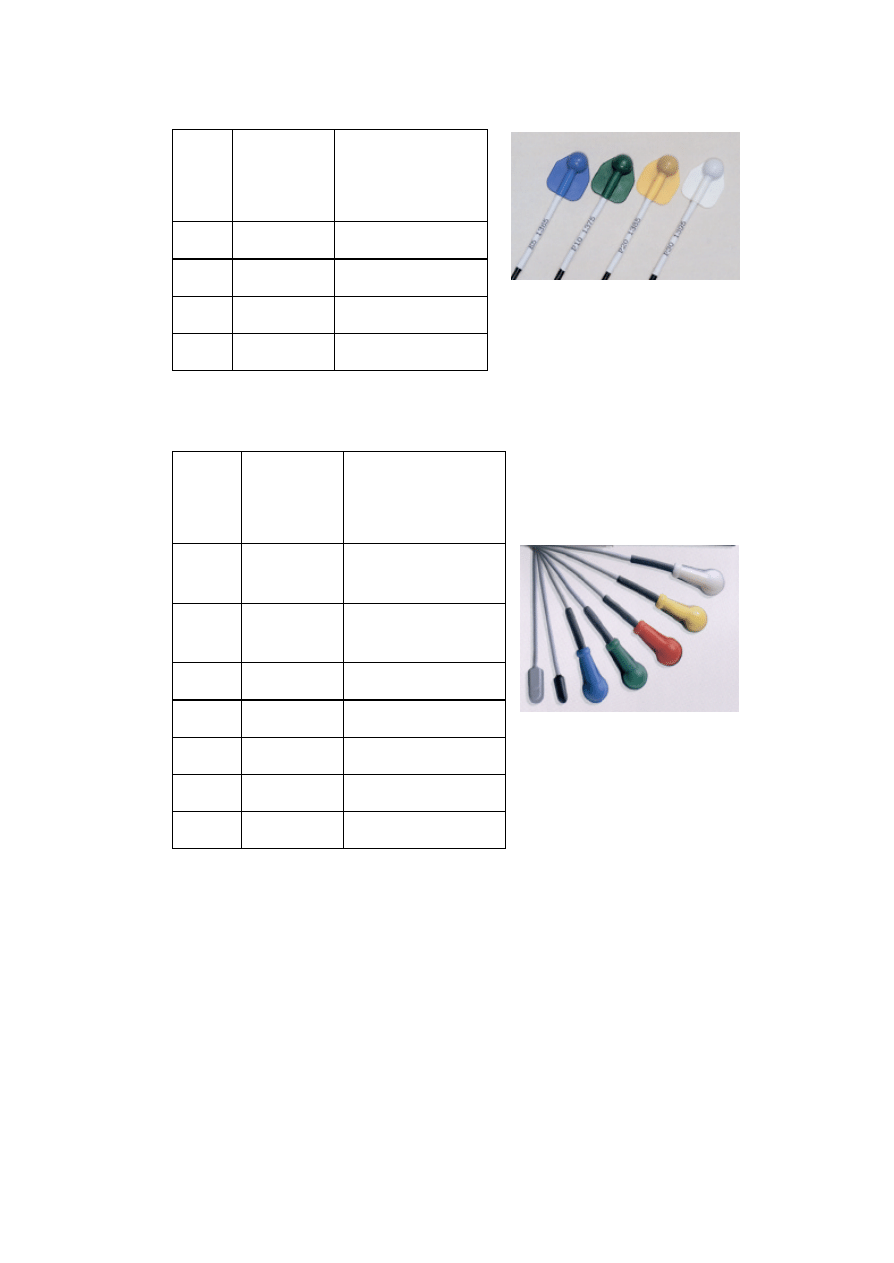
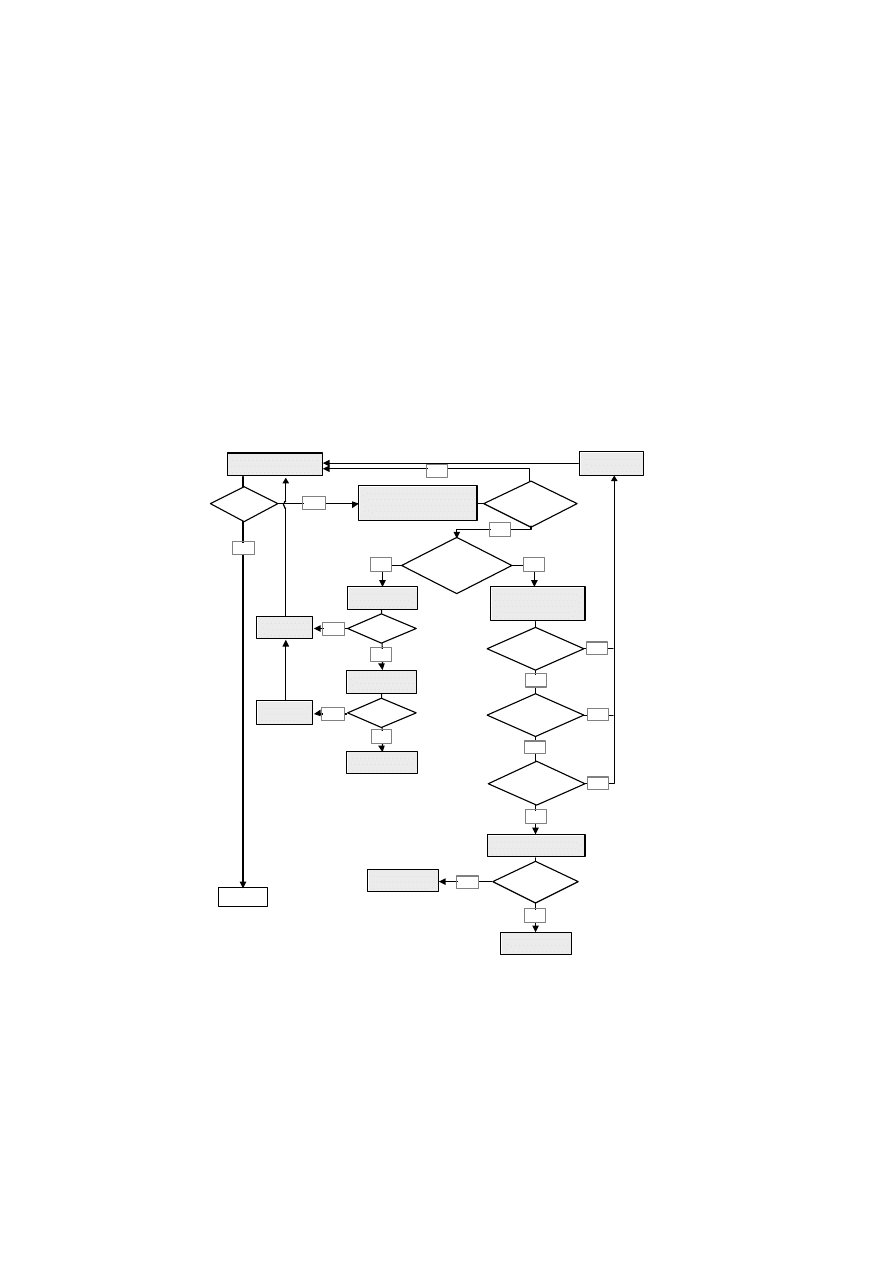
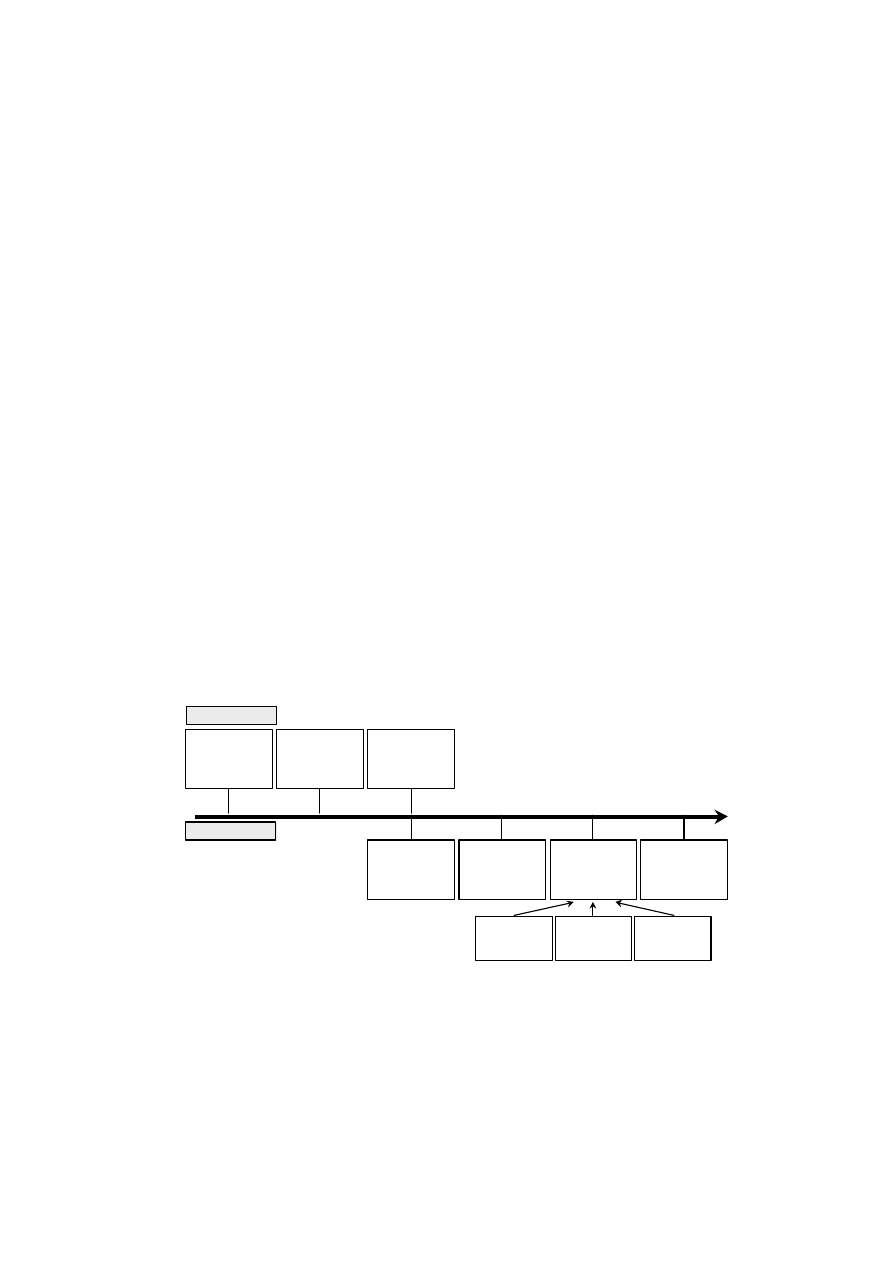
Examples of guideline flowcharts, including actions undertaken at different levels, are given
in Figure 2.1 and Figure 2.2; more examples are given in the questionnaire of Chapter 4. The
possible origin of errors and the actions undertaken are discussed in more detail in
Sections 3.2 and 3.3. Typically, the investigation of an error is performed in two steps.
Because of the on-line read-out, the first action can be triggered instantaneously by the
technical staff, who performs an immediate check on the spot. If the origin of the error is
not found, an “a posteriori” check should be performed by a physicist/QA personnel.
out-of-tolerance
signal for most of the
patients that day?
immediate check:
patient set-up/ diode
error on IVD
chart?
phantom simulation
OK
error on
dosimetry chart?
check diode
calibration factor
“a posteriori” check:
IVD chart check;
data transfer, MU check
is treatment OK?
yes
no
no
no
no
yes
yes
yes
START:
entrance measurement
signal
within 5 %?
clearly wrong
diode/patient
position?
yes
no
error found?
correct /
recalibrate
check accelerator
output
error found?
yes
stop
treatments
no
stop treatments;
discussion
no
correct
no
error in MU
calculation?
no
stop treatment;
discussion
check diode
correction factors
yes
yes
yes

33
Figure 2.1 Example of a flowchart (taken from Barcelona), guiding the actions to be
undertaken after an in vivo entrance dose measurement.
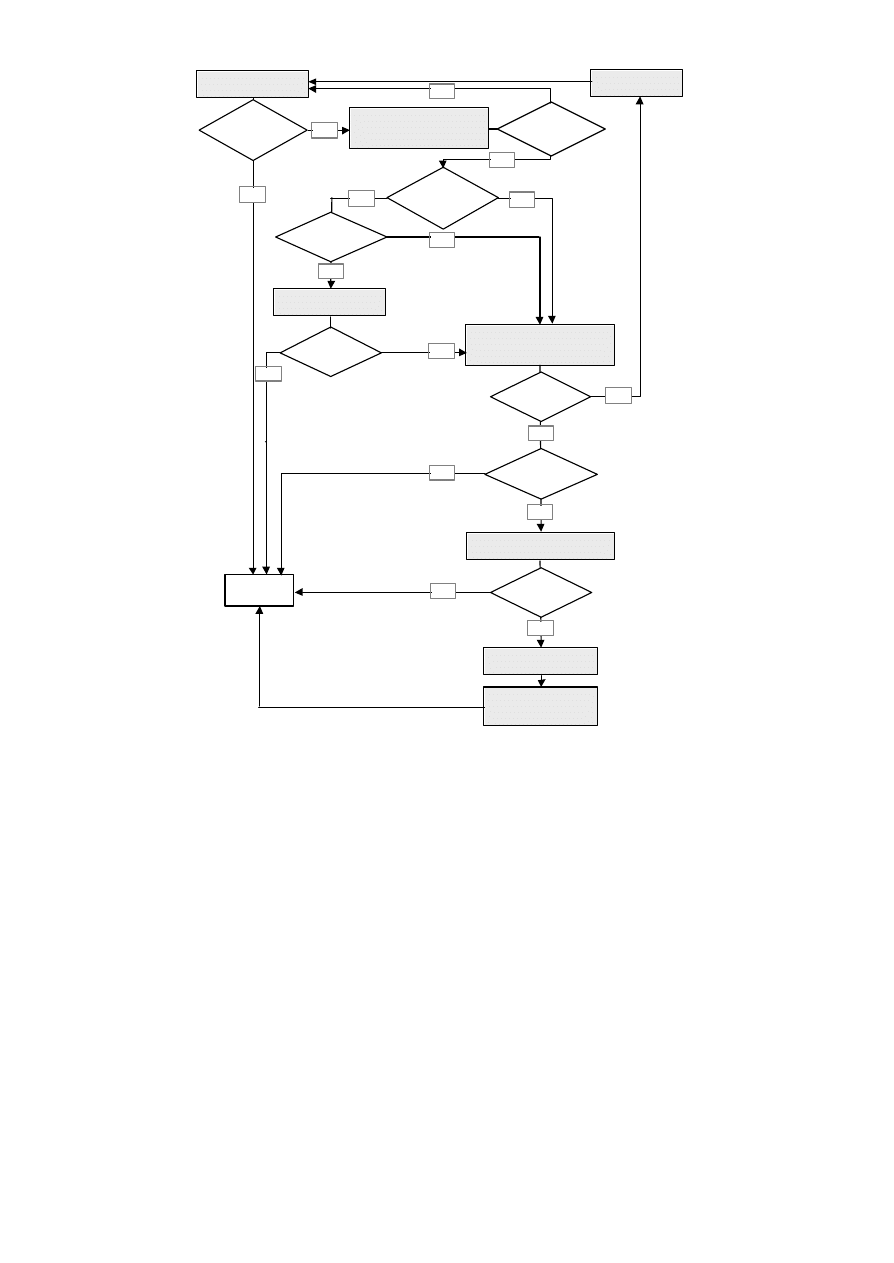
34
Figure 2.2 Example of a flowchart (taken from Leuven), guiding the actions to be
undertaken after an in vivo entrance dose measurement. The tolerance level
coincides with the lowest action level.
wedged field
or IMN (critical
diode position)?
signal
within tolerance?
immediate check “on the spot”:
record SSD and SDD;
check diode position
treatment
plan/data transfer
error?
new measurement
by QA personnel
phantom simulation
OK
wrong SDD,
wrong calculated
signal?
signal within
action level 2?
second measurement
“a posteriori” check:
data transfer check;
recalculation expected signal
signal within
tolerance?
treatment plan
modification
yes
no
no
no
no
no
no
no
yes
yes
yes
yes
yes
yes
discussion with Head of
Physics Department;
check of equipment
START:
entrance measurement
signal
within tolerance
(= action level 1)?
clearly wrong
diode/patient
position?
yes
no

35
2.3 RECORDING OF IN VIVO DOSIMETRY
Recording of the in vivo entrance dose may be done on a treatment chart, on a separate
sheet for QA and/or in a database accessible in a network (possibly linked to the R & V
system
1
). The results should be easily available (after the first treatment session, during
chart rounds, etc.).
It is important to record in vivo dosimetry data together with sufficient information, such as
the date of measurement, the type of field, the treatment unit, the anatomical location and
so on. The more complete the database is, the more information can be derived when
reviewing in vivo dosimetry data (see Section 3.3.3).
1
Some R & V systems offer at present the possibility to record or enter manually the
measured in vivo signal.

36
CHAPTER 3 INTERPRETATION OF THE MEASUREMENT
3.1 DEFINING TOLERANCE A ND ACTION LEVELS
The choice of tolerance/action levels is very important since they will in practice determine
the number of "errors" detected and will influence the associated workload t o implement or
to maintain in vivo entrance dose measurements at a departmental level. If a too broad
tolerance window is adopted, some causes of erroneous treatment delivery may not be
detected (for instance a wedge 30° instead of a wedge 15°, presence of a tray etc.). If the
tolerance window is too small, a too large number of measurements will have to be repeated
(due to e.g. inherent statistical fluctuation or a too critical positioning of the diode in e.g.
wedged beams). Clearly, the value and the meaning of the levels are related to the
philosophy of the department regarding in vivo dosimetry. Some centres using in vivo
dosimetry as a routine check for every patient, distinguish the first level, the tolerance
level, from higher action levels. A deviation of the diode signal beyond the tolerance level,
but within the action levels, is considered as a warning, linked to a very limited action.
When in vivo dosimetry is used to check particular treatments, the value of the levels can
vary according to the treatment type. Treatments with high dose - high precision
techniques require narrow tolerance windows, while other treatments have less stringent
accuracy demands. In certain centres, it could be realistic to set higher tolerance/action
levels for patients treated with palliative intent in order to minimise the number of second
measurements, paying more attention to the patients treated with curative or adjuvant
intent.
The determination of the actual value of the level is based on different factors, first of all on
the uncertainty of the diode measurement method. According to Essers and Mijnheer
[
Essers 1999
]
, the theoretical uncertainty in measuring the entrance dose with diodes,
taking into consideration the uncertainties in the calibration factor, the correction factors
and the positioning of the diode, is 1.6 % (1 standard deviation (SD)). This means that
37
without any additional cause for deviation or error, 68% of the measurements would be
within 1.6 % and 95 % of the measurements would be within 3.2 % (2 SD) of the expected
dose. This seems to be in agreement with other results reported in the literature, although
such a level of accuracy is probably difficult to obtain for all types of irradiation, for
instance for treatments with tangential wedged beams. It also has to be stressed that this
high level of accuracy is attainable only if a very accurate estimate of diode correction
factors is accomplished. It has to be kept in mind that a choice of “minimum” correction
factors, which could be preferable in small and medium centres with a small physics staff,
means a larger uncertainty in dose estimation and, consequently, results in the necessity of
higher tolerance/action levels.
Other sources of uncertainty, which should be taken into account when choosing the
levels, are:
•
the physiological movements due to breathing and/or possible movements of the
patient during irradiation; the difficulty in firmly attaching the diode in some regions
due to the presence of hair
•
the use of ancillary equipment to set-up the patient (i.e.: head masks, head-rest,
immobilisation shells…) [Essers 1994]. In these cases the diode reading has to be
corrected to take the real SDD into account, which can be difficult to assess in some
situations. Moreover, some loss of backscatter may occur in many situations, which is
another source of uncertainty, as this is usually not taken into account by the TPS.
Also, it should be kept in mind that the positioning of the diode on immobilisation
shells (or on the back of the couch when treating with dorsal fields) results in a larger
uncertainty if the temperature dependence of the diode signal is accounted for in the
calibration factor (see Section 1.2.2)
•
the true SSD, if the diode reading is not corrected to take into account the difference
between the true SSD and the planned one. If the correction is performed, in some
situations, it is difficult to calculate the correction factor (for instance in posterior-
anterior fields or in some tangential fields)

38
•
the use of asymmetric fields, e.g. for tangential breast treatments (see Section 5.4.2)
•
possible fluctuations of accelerator output
As the in vivo measured entrance dose has to be compared with the expected one, which is
calculated by the TPS or by an independent formula, the uncertainty in the entrance dose
calculation is another factor that should be taken into account. This uncertainty depends
on:
•
the algorithms used for dose calculation
•
the method used for calculating MUs
•
the way in which inhomogeneities are taken into account
•
the way in which treatment unit data have been acquired (for instance the precision
with
which d
max
has been determined)
The majority of the radiotherapy centres have a 5 % action level for most treatments (see
Chapter 4 and Sections 5.4). The tolerance level usually coincides with this level, according
to the philosophy that any deviation larger than 5 % must be investigated. A procedure
recommended for establishing the narrow tolerance window required for high dose - high
precision techniques is to investigate the attainable measurement accuracy for the
particular technique and take twice the SD of the measurement uncertainty as the
tolerance/action level ([Essers 1993], [Essers 1994], [Lanson 1999]). In this case, however,
entrance dose measurements are usually combined with exit dose measurements to obtain
the target absorbed dose.
Once the tolerance and action levels have been established, the range of acceptable
variation of some of the parameters can be determined in order to facilitate the search for
the cause of an out-of-tolerance signal. Acceptable deviations in stated SSD versus
measured SSD (or SDD) for isocentric and fixed SSD techniques can be determined. The
importance of daily beam output variations can be assessed.

39
It is important to verify during a certain period whether the tolerance/action levels are
adequate for clinical routine. An important indicator is the rate of second measureme nts,
which is strictly related to the action level. A too small rate (for instance less than 2-3%)
should be regarded with caution because it might indicate that the action level is too high.
Inversely a too high second check rate (for instance larger than 15-20 %) could mean that
the level is too small. In
particular a high rate of second checks can generate distrust
concerning the real usefulness of in vivo dosimetry among the operators and the medical
staff. An alternative method for adjusting the tolera nce/action levels is to adapt it to the SD
of the measurements. This parameter can be determined by pooling the patients for a
certain period.
It is clear that the continuous monitoring of systematic in vivo dosimetry after its
implementation is mandatory in order to reduce the errors of the control process and
possibly to adjust tolerance/action levels in time if they appear to be inadequate (see
Section 3.3.3). Such a monitoring could also help defining differe nt tolerance/action levels
for different types of patient treatments and/or beam set-up. For instance, it could become
clear whether wedged beams need higher tolerance/action levels with respect to unwedged
beams because of the corresponding larger uncertainty.
3.2 WHICH ERRORS CAN BE DETECTED?
It is important to keep in mind that when a deviation is observed out of the tolerance level,
it is not necessarily an error in the treatment process but it may be linked to a
malfunctioning of the quality control process.
3.2.1 MALFUNCTIONING OF THE QUALITY CONTROL PROCESS
Deviations between measured and prescribed entrance dose due to an erroneous
measuring procedure at a departmental level can affect the confidence in in vivo dosimetry.
If, for instance, during a chart round a radiation oncologist finds out that most of the in
40
vivo measurements are out of tolerance (due to a problem in the QC process), it is rather
difficult to yet convince him that his patients are indeed correctly treated, and/or that in
vivo measurements are useful.
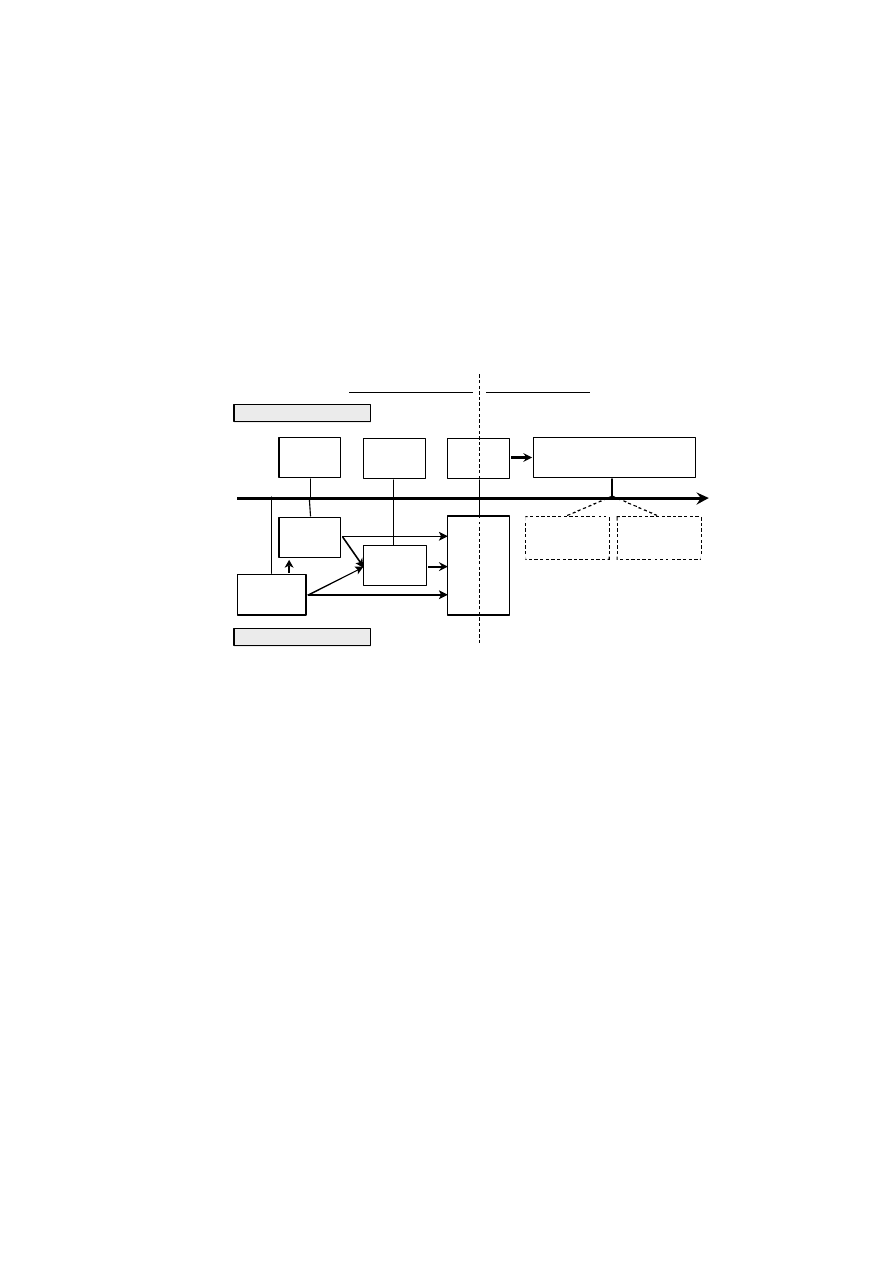
Malfunctioning of the QC process (Figure 3.1), may be present either at the departmental
level, leading to systematic errors (i.e. for all patients), or at the individual level. Systematic
errors are typically errors (or a shift) in the calibration factors of the diodes or an error in
the correction factors (or omitting some necessary correction factors). Systematic errors
may also be induced by erroneous calculation (with or without TPS) of the entranc e dose.
Depending on the procedures of the department, systematic deviations in the QC process
may increase the workload since one might start to look for a “real” dosimetric error and/or
one might request a new measurement to exclude other “individual” errors in the QC chain.
The individual
errors in the QC chain for entrance dose are mainly the following ones:
•
miscalculation of the expected diode signal from the entrance dose (use of wrong
calibration factor, correction factors), which irritates personnel
•
misrecording the SDD
•
erroneous read-out or record of the measured in vivo signal, which is sometimes
difficult to trace by the physicist/QA personnel
•
bad positioning of the diode: not in the centre, too close to shielding blocks, etc. (cfr.
Section 2.1)
•
bad fixation of the diode
systematic
•
determine
calibration
factor
determine
correction
factors
convert
read-out
signal/dose
calculate exp.
read-out
signal/dose
record SSD
position
diode
accessories
in the beam
shielding
blocks
wedge
read-out
electrometer
•
•
•
•
•
•
individual
41
treatment unit:
treatment machine + table
•
•
R & V
R & V
simulator
•
simulator
TPS
•
TPS
prescription
•
treatment unit
set-up
patient
set-up
treatment preparation
treatment delivery
equipment breakdown
human errors
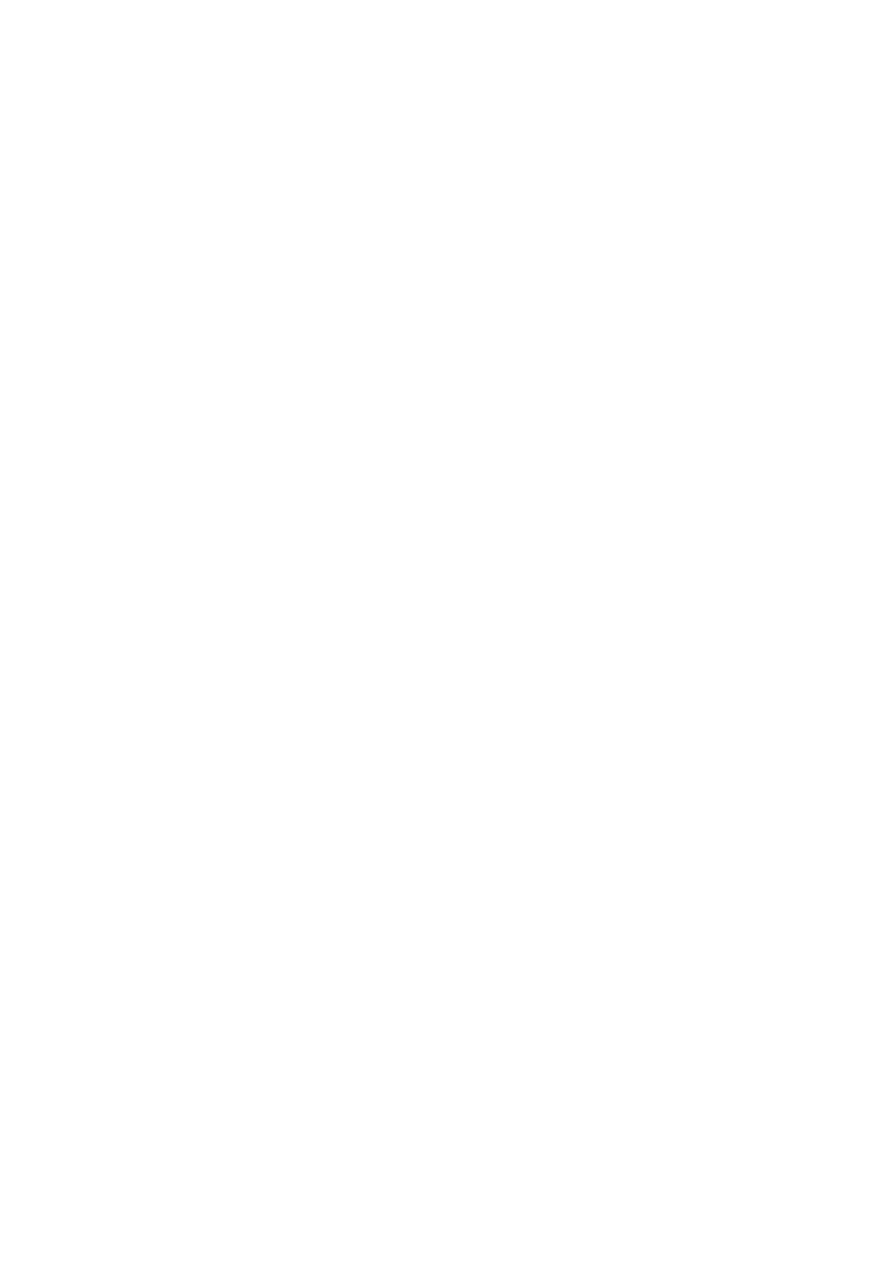
Figure 3.1 Schematic representation of error-prone steps in the quality control process
3.2.2 DEVIATIONS IN THE TREATMENT PROCESS (DOS IMETRIC ERRORS)
To facilitate the analysis of possible errors in the treatment chain, dosimetric errors are
divided into three categories:
•
human errors in data generation and data transfer
•
errors due to equipment breakdown or malfunctioning
•
positioning discrepancies between treatment planning and delivery
Figure 3.2 Schematic overview of the radiotherapy process.
3.2.2.1 ERRORS IN DATA GENERATION AND DATA TRANSFER (HUMAN ERRORS)
In Figure 3.2 a compact scheme is given of the radiotherapy process from prescription to
delivery. Each arrow in the diagram represents a transfer of data, which is error prone, and
every box may generate erroneous data. Depending on the organisation of the department
42
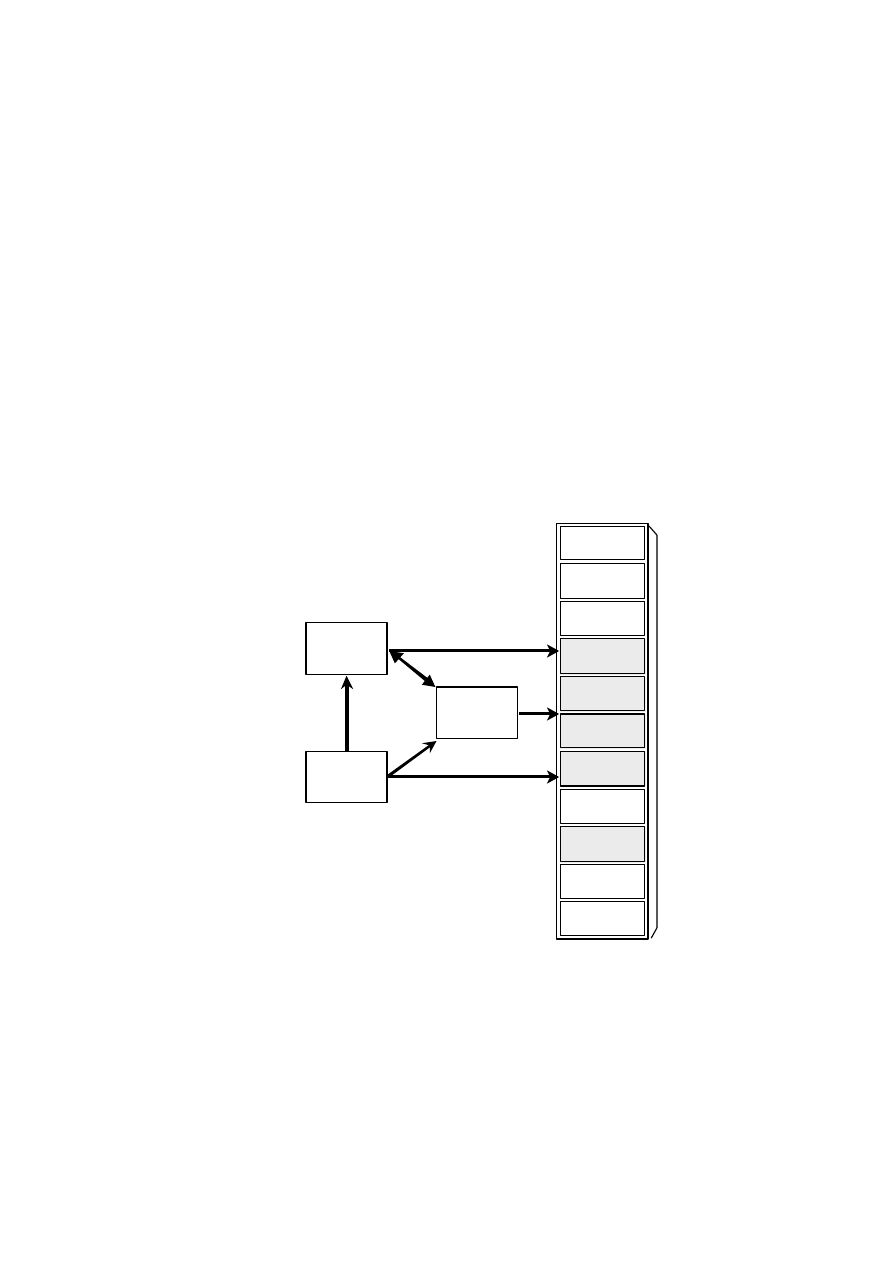
R & V
and/or
treatment chart
simulation
parameters
prescription
parameters
TPS
immobilisation
device
gantry angle
collimator
angle
field size
modality/
energy
MUs
(dose/fraction)
wedge
shielding
blocks
table
parameters
SSD
bolus
and on the possibilities of the available equipment, the practical information transferred
between the boxes may be different. At the end of the chain, before treatment delivery,
parameters are either recorded in a Record and Verify system (R & V) or written on the
treatment chart.
An erroneous transfer of prescribed dose from prescription to TPS can only be detected by
in vivo dosimetry if the entrance dose is calculated by hand or with an independent "home
made" system to predict the expected diode signal. If the planning target dose is - by
mistake - different from the prescribed target dose, the entrance dose calculated (manually)
with the prescribed dose will differ from the entrance dose calculated with the TPS, and
hence will be detected. The dark boxes in the last column of Figure 3.3 represent the other
parameters for

43
Figure 3.3 Overview of the parameters of the treatment preparation process
which errors can be detected by entrance in vivo dosimetry, whether or not the TPS is used
to calculate the entrance dose:
•
involuntary absence or presence of beam attenuators:
wedge
Presence or absence of the wedge in the beam can be considered as an important
cause of accidental treatment delivery (differences in absorption rates up to 60 %
for heavy wedges can occur). A discrepancy in the choice of the wedge (for
instance 45° instead of 30°) will also be detected by entrance in vivo dosimetry.
However, errors in the orientation of the wedge will not be detected by entrance in
vivo dosimetry (on the beam axis).
tray and blocks
Since the absorption rate of a tray holder is usually a few percent, its presence or
absence can be monitored. However, erroneous block positioning in the field is
unlikely to be detected by means of entrance in vivo dosimetry.
individual compensators
Errors in the positioning or in the choice of individual compensators may be
detected by in vivo entrance dose measurements.
•
treatment modality and energy
From a theoretical point of view, measuring the entrance dose is not a conclusive
method to detect errors in modality (photons, electrons) or in beam energy since
both the response of the diode and the dose rate of the various beams may be
different. However in practice these types of errors may also be detected as
reported for instance by Essers et al. [Essers 1999] for a dual energy linac.

44
Depending on the magnitude of the discrepancy between the prescribed field size and the
actual field size, the measured in vivo entrance dose theoretically shows an error in the
treatment delivery. In practice this error is so small that errors in field size are normally not
detected by in vivo dosimetry but only by portal imaging.
Before treatment execution, an independent check of data transfer (including MU
calculation) on the treatment chart and/or the R&V system should always be performed
[AAPM 1994]. It has been demonstrated that this simple tool significantly reduces the
incidence of human erro rs. However, even with this systematic check, in vivo dosimetry is
indispensable to trace a number of errors that otherwise would escape attention
([Calandrino 1997], [Duggan 1997], [Essers 1999], [Fiorino 2000]).
3.2.2.2 ERRORS DUE TO EQUIPMENT BREAKDOWN OR MALFUNCTIONING
As shown in Figure 3.2 radiotherapy departments may suffer from a breakdown or
malfunctioning of equipment at 4 levels which may translate into erroneous treatment
delivery: the simulator, the TPS, the R & V and the treatment unit (encompassing the
treatment unit itself, the treatment couch, fixation devices etc.). While a breakdown or
malfunctioning of the simulator is not so likely to be detected by in vivo dosimetry,
breakdown of the treatment unit and more specifically large variations in beam output can
easily be detected by in vivo entrance dose measurements. A typical other source of errors
which can be unveiled by entrance dose measurements is malfunctioning or incorrectly
used new software or a software upgrade for the calculation of MU ([Leunens 1993],
[Lanson 1999]). As far as the R & V system is concerned, malfunctioning is potentially very
dangerous if the system is also used for setting up the patient, and can be discovered by in
vivo dosimetry.

45
3.2.2.3 DISCREPANCIES IN PATIENT POSITIONING/GEOMETRY BETWEEN
TREATMENT PLANNING AND DELIVERY
Deviations in patient set-up at the time of treatment delivery can be due to random human
errors (especially if the treatment couch parameters are not verified by the R & V system
[Leunens 1993]) or to systematic machine-related errors (like a bad resetting of the “zero”
indicator of the simulator couch (Section 5.4 and [Fiorino 2000]), in which cases they
belong to the two previous categories of errors. Other sources of a wrong positioning,
however, are patient motion or a change in patient thickness due to swelling or shrinkage.
While entrance dose measurements give only direct information about the patient set -up
with respect to the beam (in particular an incorrect SSD), they also result in the detection of
patient thickness errors, if patient thickness is reassessed to trace the origin of a large
incorrect SSD.
3.3 EVALUATION OF IN VIVO DOSIMETRY DATA
3.3.1 ACTIONS AFTER THE FIRST MEASUREMENT
If the result of the first measurement is outside the tolerance/action level, a number of
controls should be activated (see Figure 2.2). This chain of controls involves checks in
order to reveal either quality control process errors (e.g. the immediate check of the diode
position, or the “a posteriori” recalculation of the expected signal) or real treatment process
errors (e.g. the immediate check of the patient position, or the data transfer control in the “a
posteriori” check).
First, an immediate check (i.e. with the patient on the treatment couch) of the treatment set -
up and treatment parameters must be performed. The most common errors are differences in
SSD and wrong positio ning of the diode, which can both be checked by the radiographers
on the spot. Differences in SSD due to the use of immobilisation devices or bolus should
be corrected by the appropriate inverse square law correction factor; in other cases the
SSD deviation signifies a real treatment process error (see Section 5.4). An evaluation of

46
the correct
positioning of the diode in the field centre can still be made afterwards on a
portal image (for treatment geometry verification), if this was taken simultaneously with the
diode measurement ([Essers 1994], [Lanson 1999]).
If no explanation of the discrepancy is found, further “a posteriori” checks should be
performed, possibly the same day as the in vivo control. The “a posteriori” check should
concern the data transfer control, checking the congruence of all technical and dosimetry
data of the treatment planning/simulator chart to the corresponding data on the treatment
chart (and/or R&V system). It must include the agreement between the effectively delivered
MU against the planned ones, the correctness of MU calculation and the correct use of
wedges and blocks. If the in vivo dose with blocked fields is lower than the expected one,
the diode position should be checked especially if the block is near the irradiation field
centre. In any case, it is a good practice to perform a second in vivo control check, also if
no apparent errors are found.
Tolerance levels generally coincide with action levels in most institutions. If t his is not the
case, performing merely a second in vivo dose measurement could be a limited, time -saving
action related to an out-of-tolerance deviation within the action level. A similar approach
can be followed if two different action levels are defined (“low” and “high”, for instance: 5
and 10 %). If the measurement is outside the “low” level, but still within the “high” action
level, the immediate check may for instance be avoided and just an “a posteriori” check
could be performed by the physicist.
3.3.2 PERSISTING DEVIATIONS: INTERPRETATION OF THE RESULT
A number of papers report that a lot of deviations exceeding the action level might not be
related to proven human errors or errors due to equipment breakdown ([Cozzi 1998],
[
Essers 1999
]
, [Heukelom 1991a], [Leunens 1990a], [Leunens 1991], [Loncol 1996], [Mangili
1999], [Millwater 1998], [Mitine 1991], [Noel 1995],
[
Voordeckers 1998
]
). On the other side a
second measurement reduces the probability of some quality control process errors such

47
as bad diode positioning. So, in the chain of control checks following in vivo dosimetry,
some deviations might not be attributed to a treatment process error nor to a quality
control process error. For such a situation the data should be discussed by the
physics/QA team and the origin should be traced.
In order to facilitate the search for the cause of the persistent deviation, an entrance dose
measurement with the diode and an ionisation chamber in a solid phantom in the same
clinical treatment conditions (SSD, field size , gantry and collimator rotation, block,
wedge…) may be useful. This is particularly true during the first phases of implementation
of systematic in vivo dosimetry procedures, when the accuracy of in vivo dosimetry in the
various clinical situations may not fully be assessed. If the deviation between the phantom
entrance dose measured with the diode and the calculated one is acceptable, the in vivo
deviation could be attributed to a difficulty in the diode positioning on the patient’s skin. If
the dose meas ured with the ionisation chamber is in agreement with the expected one, but
the diode reading is not correct, the deviation of the diode signal could be explained by a
bad calibration or wrong correction factors. If the phantom entrance dose measured with
the ionisation chamber is not in agreement with the expected dose, dose calculation
mistakes might be present.
In general, the main causes of persistent deviations are:
•
difficulties in setting up the patient: these are more likely to be detected if diode
readings are not corrected by inverse square correction factors
•
uncertainty in diode reading due to critical positioning (tangential beams, wedged
beams,…) or to lack of correction factors
•
bad electrometer/diode calibration
•
erroneous calculation of the entrance dose by the TPS
When the cause of the discrepancy is identified, an action may be required for the single
patient such as checking patient positioning at the simulator and/or checking the patient’s
thickness. If persistent deviations sytematically occur for a certain configuration of beams
(for instance wedged fields), more accurate assessment of diode correction factors or

48
further investigations on the accuracy of dose calculation may be required. After reviewing
a large set of data, a high rate of second checks/persistent deviations for a certain
configuration of fields may also suggest a modification of the tolerance/action level for
such a category.
3.3.3 MONITORING IN VIVO DOSIMETRY WITH TIME
After implementing a procedure for systematic in vivo dosimetry, it is very important to
continuously monitor the adequacy and the efficacy of the system. A periodic review of
the database of in vivo dosimetry data with some statistical analysis is very useful to drive
the physicist and the clinician in adjusting the procedures to the real local conditions. An
important goal is the verification of the adequacy of tolerance/action levels: a too high rate
of second checks may have a negative impact on the operators and efforts should be made
to reduce the additional wo rkload, while maintaining an acceptable action level.
Continuous monitoring of in vivo dosimetry data may therefore indicate the need for
adjustment with time of tolerance/action levels.
Statistical analysis of the deviations between expected and measured entrance dose may
give information suggesting possible fields of investigation and/or possible improvements
of the quality control process (for instance, more accurate assessment of diode correction
factors, new schedule for diode calibration etc.).
Although some errors or inaccuracies may also be detected on an individual basis, they
will be clearer with a statistical approach because of the existence of fluctuations in the
measuring procedures. Subgroups of patients can be pooled for instance breast, hea d &
neck, brain, etc. The distribution of the deviations has been shown to reveal systematic
errors linked to specific treatment techniques or to calculation methods. Some relevant
examples concerning large cohorts of patients are given in the literature [Noel 1995],
[Leunens 1990a], [Leunens 1990b], [Leunens 1991] and [Fiorino 2000] and in the single
institution’s experiences as reported in Chapter 5. It should be realized that this very

49
interesting and useful type of evaluation also requires considerable manpower, if no
computerized support is available for statistical analysis.
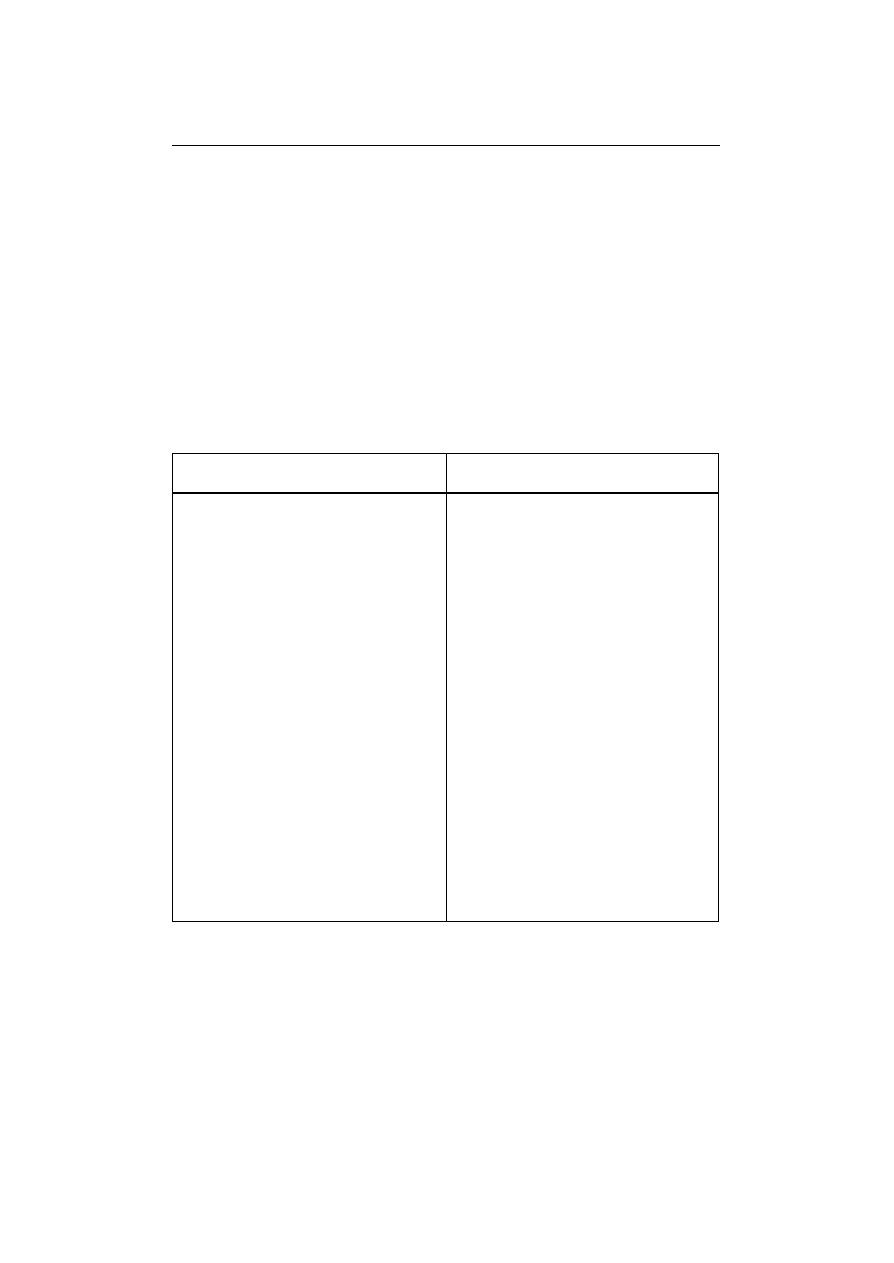
50
CHAPTER 4 TECHNIQUES AND PROCEDURES IN DIFFERENT
RADIOTHERAPY CENTRES
The following information concerning clinical in vivo dosimetry procedures (not
exclusively oriented towards entrance dose measurements) is the result from a
questionnaire that has been sent to centres having experience with routine in vivo dose
measurements. Apart from the institutions which have co-operated for this booklet, the
‘Nederlands Kanker Instituut’ from Amsterdam and the ‘Centre Alexis Vautrin’ from Nancy
have provided information (see also [Essers 1993, 1994, 1995a and 1995b], [Heukelom
1991a, 1991b, 1992, 1994], [Lanson 1999] for Amsterdam and [Noel 1995] for Nancy).
4.1 WHAT EQUIPMENT DO YO U USE TO CARRY OUT ROUTINE IN VIVO DOSE
MEASUREMENTS?
LEUVEN
BARCELONA
Irradiation equipment
- X-rays : 6, 18 MV
(Saturne 40, 42, GE, Clinac 2100, Varian)
Irradiation equipment
- X-rays 6, 18 MV / e
-
6 - 16 MeV
(Clinac 1800, Varian)
In vivo dosimetry equipment
DPD6, DPD3, DPD510 (TBI) electrometer
(Scanditronix)
- Diodes (Scanditronix)
6 MV
EDP-20, EDP-20+1 mm Cu
18 MV
EDP-20, EDP-20+1 mm Cu
TBI
EDE
In vivo dosimetry equipment
- DPD510 electrometer (Scanditronix)
- Diodes
6 MV
EDP-10 (Scanditronix)
18 MV
EDP-30 (Scanditronix)
QED 1116 (Sun Nuclear)
P30 (Precitron)
Isorad-p 1164 (Sun Nuclear)
electrons
EDD-2 (Scanditronix)
TBI
EDP-30 (Scanditronix)

51
NANCY
COPENHAGEN
Irradiation equipment
-
60
Co (Th780, AECL)
- new multimod. LINAC
(X-rays 6, 10, 25 MV, Saturne 43, GE-CGR),
(X-rays 6, 10 MV, SL15, Elekta),
(X-rays 6, 25 MV, Clinac 23EX, Varian)
Irradiation equipment
X-rays 4, 6, 8 and 18 MV
(Varian Clinac 600C, Clinac 2100C, Clinac
2300CD)
In vivo dosimetry equipment
- DPD3, DPD5 or DPD6 electrome ter
detection and diodes assembly
(Scanditronix)
- Diodes
p-type diodes except for two n -type
diodes with additional correction factors:
60
Co
cobalt
6 MV
HE or -10 (Scanditronix)
10 MV
EDP-10 (Scanditronix)
25 MV
EDP-20 (Scanditronix)
(electronic equilibrium if necessary
obtained with bolus)
- Apollo5, Apollo10 electrometer detection
and diodes assembly (Precitron AB) for
TBI
In vivo dosimetry equipment
- electrometers:
Apollo 5 (Precitron)
- Diodes
4 MV
P10 (Precitron),
6 MV
P10 (Precitron),
QED 1115 (Sun Nuclear)
Isorad-p 1163 (Sun Nuclear)
8 MV
P20 (Precitron)
Isorad-p 1163 (Sun Nuclear)
18 MV
P30 (Precitron)
QED 1116 (Sun Nuclear)
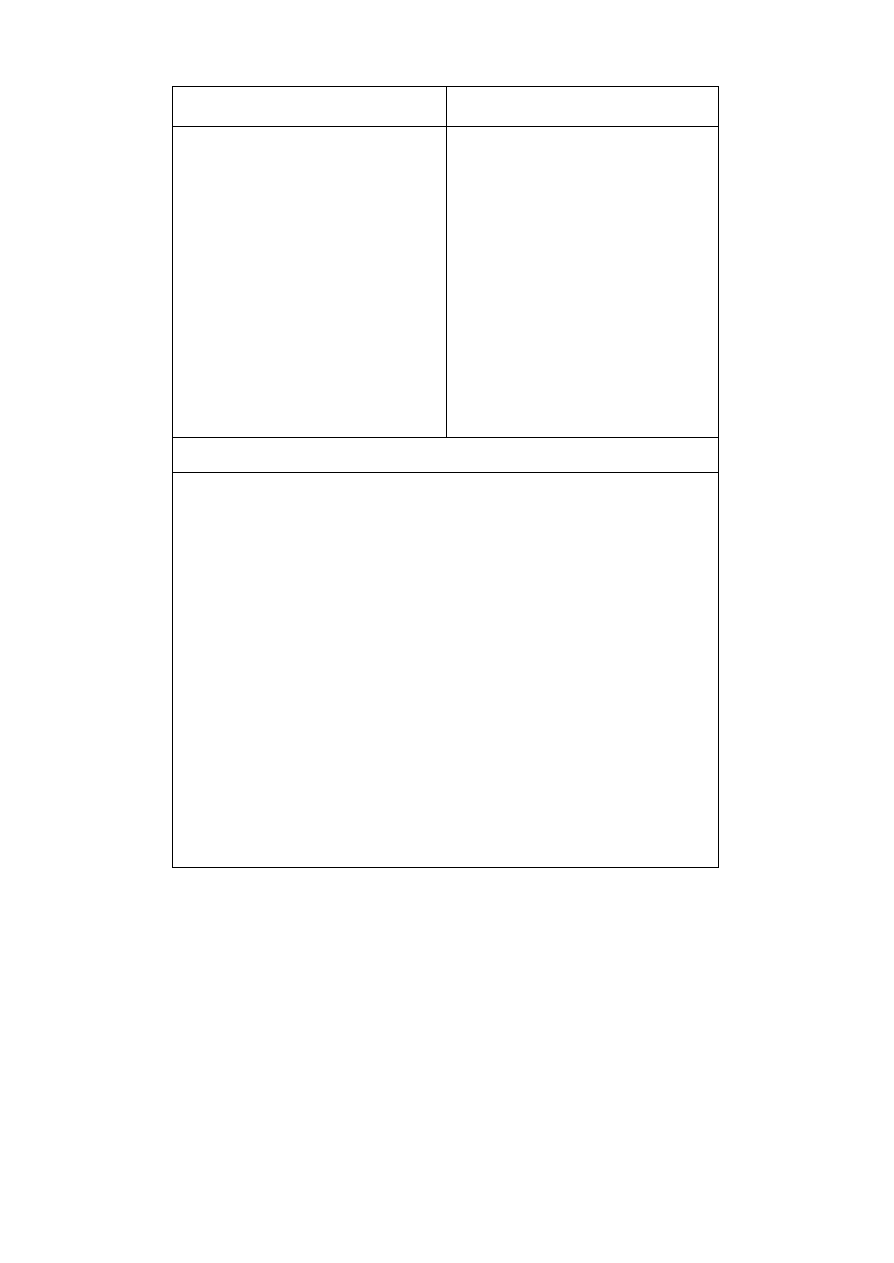
52
AMSTERDAM
MILANO
Irradiation equipment
in vivo dose measurements performed for
- X-rays 6 and 8 MV (Philips SL15/SL25)
- X-rays 4 MV (ABB)
Irradiation equipment
- X-rays 6 MV (Linac 6/100)
- X-rays 18 MV (Linac 1800, in vivo
dosimetry to be implemented)
In vivo dosimetry equipment
- p-type diodes (Scanditronix EDP-20)
coupled to a custom-built diode measuring
system (hardware (electrometer) and
software (diode measurement files)
In vivo dosimetry equipment
- DPD510, DPD3 electrometer
(Scanditronix)
- Diodes
EDP-10, EDP-30 (Scanditronix)
EDINBURGH
Irradiation equipment
X-rays 6, 8, 9, 15, 16 MV / e
-
5-20 MeV
(Varian 600, 600CD, ABB CH6, CH20, RDL Dynaray 10)
In vivo dosimetry equipment
DPD6, DPD3, DPD510 electrometers (Scanditronix)
Diodes (Scanditronix)
6 MV:
EDP-10, EDP-10 + 0.6 mm brass
8,9 MV:
EDP-20
15, 16 MV:
EDP-20, EDP-20 + 1.2 mm brass, copper
electrons
EDE, EDD-5, EDD-2
Mounting: home -built quick-swing ceiling mounted system; being rolled out to all
machines as new machines being installed
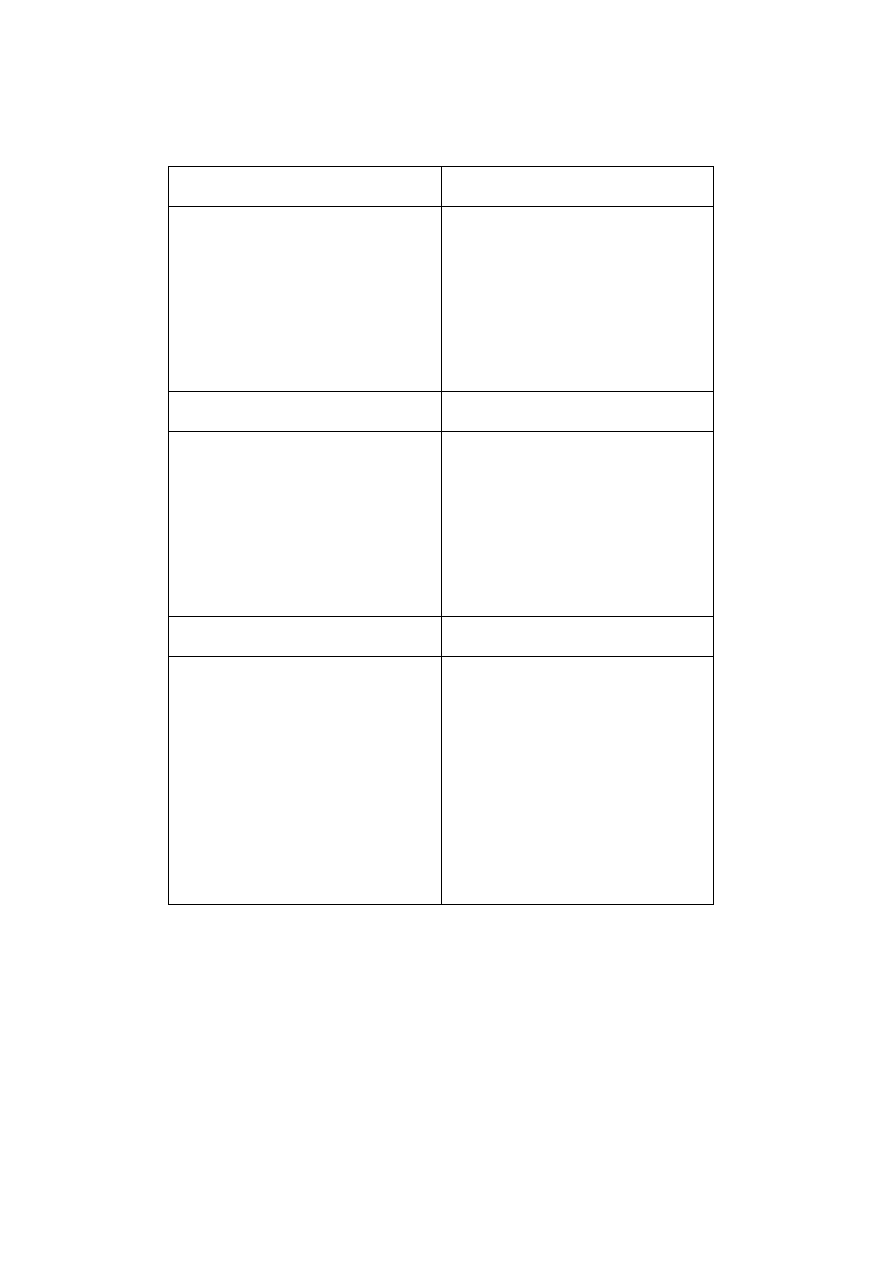
53
4.2 PHILOSOPHY OF YOUR DEPARTMENT CONCERNING THE USE OF IN VIVO
DOSIMETRY?
4.2.1 WHEN DO YOU USE IN VIVO DOSIMETRY?
LEUVEN
BARCELONA
- for every patient at first treatment session
(simultaneous with portal film)
during treatment when major changes in
irradiation parameters take place (after a
new monitor unit calculation)
- TBI treatments: first session
- for every patient treatment at the second
treatment session, and when there is a
treatment modification (first fraction:
portal film)
- TBI treatments: all sessions
NANCY
COPENHAGEN
- for every patient at the second or third
session (first fraction: portal film)
- during treatment whenever major changes
in irradiation parameters take place
(reduction of field size, blocks, wedge)
- TBI treatments: all sessions
- intention of including every patient
(achieved to 90%, still in the
implementation phase)
- within the third treatment session
AMSTERDAM
MILANO
- for two special treatment techniques with
high dose/high precision protocols:
parotid gland and prostate irradiation;
measurements are performed during two
different treatment sessio ns
- in the near future, all treatment techniques
will be checked systematically one by one
- for every patient, within the first week of
treatment. during treatment whenever
major changes in irradiation parameters
take place (reduction of field size, blo cks,
wedge)
- TBI treatments: first treatment
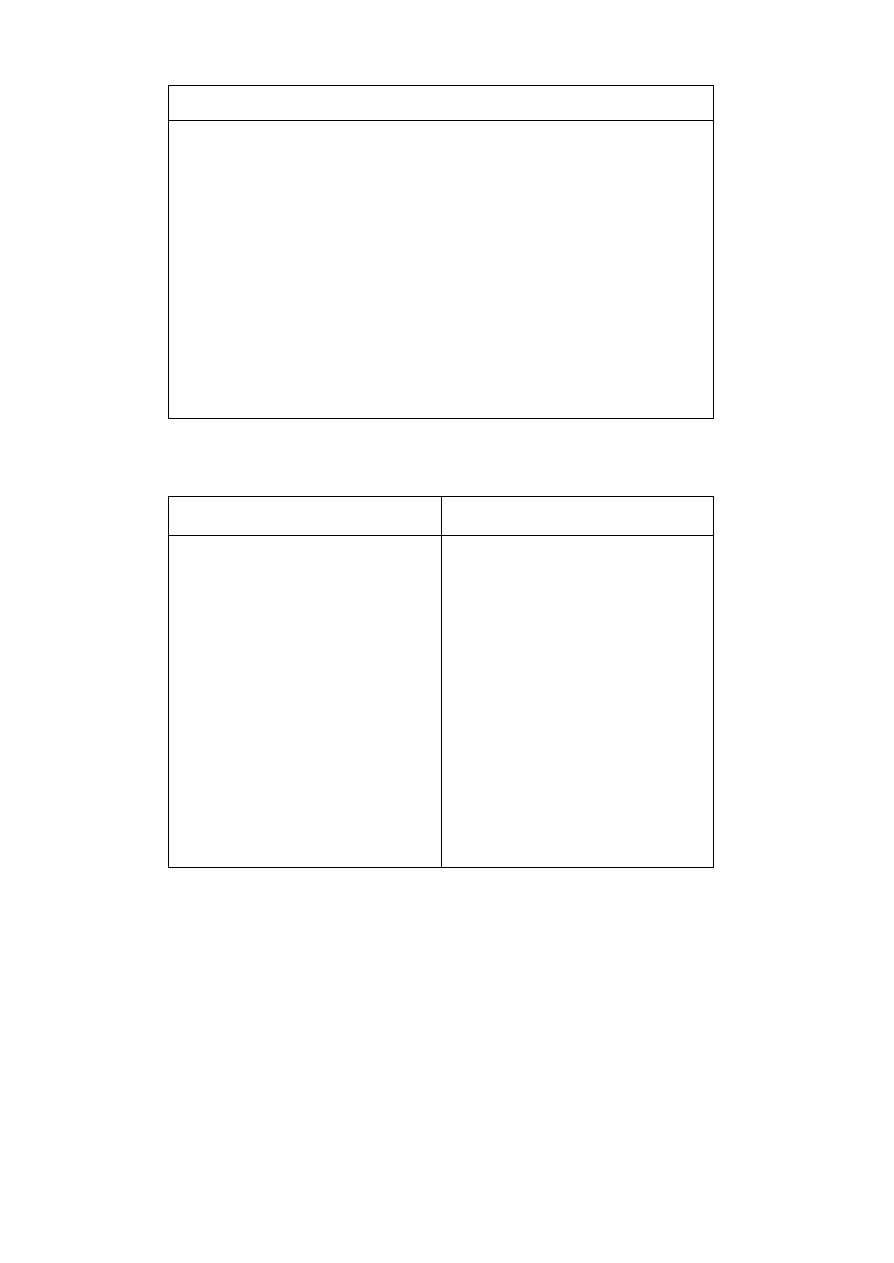
54
EDINBURGH
- all treatment machines and treatment techniques are systematically checked in detail on
sufficient patient numbers to give a statistically valid study. From this systematic
deviations are identified and corrected, random deviations are quantified; decisions are
then taken on how to implement in routine use
- in routine use, typically for every patient within the first week, or after significant
changes in treatment. Currently not on all machines; this is being rolled out to all
machines as new machines are installed
- plus, infrequent audits on a selection of patients for a given machine, site and
technique, which repeat the initial pilot studies on a small group of patients
- electron measurements ju st beginning
4.2.2 WHAT DO YOU MEASURE?
LEUVEN
BARCELONA
- entrance dose
- for opposed photon beams: target
absorbed dose by measurement of
entrance and exit doses. For each beam
the target dose is calculated from midplane
dose using a ratio of PDD. The midplane
dose is calculated as the mean multiplied
by an experimental correction factor or by
a Rizzotti approach [Rizzotti 1985]
- for non-opposed photon beams: entrance
dose
- for electrons: entrance dose measurements
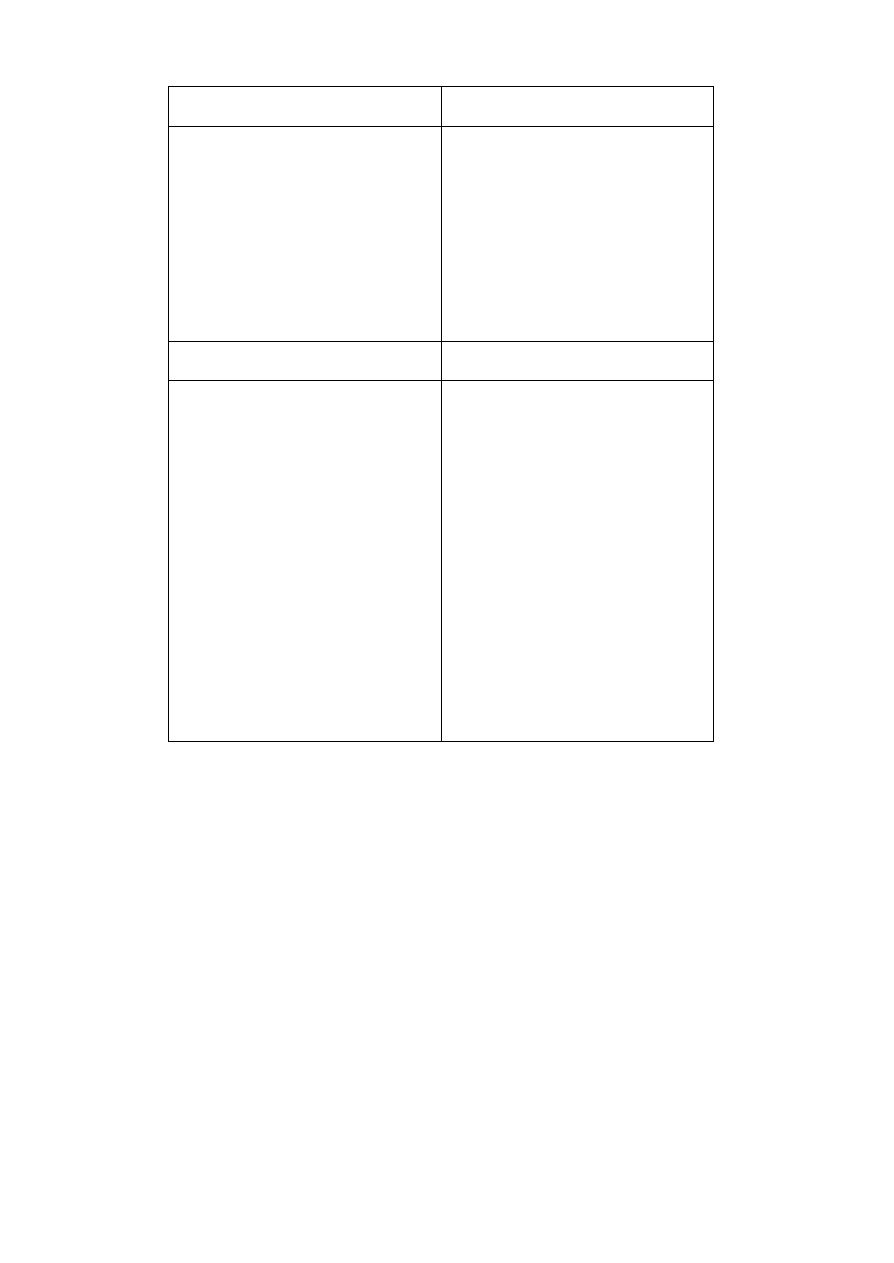
55
NANCY
COPENHAGEN
- target absorbed dose by measurement of
entrance and exit doses
- usually midline dose is calculated; else the
midline dose is for each beam converted to
the dose at the specified point using
PDDs before summing the contributions
of the different beams
- entrance dose
AMSTERDAM
MILANO
- target absorbed dose by measurement of
entrance and exit doses
- for prostate treatments, the target
absorbed dose is converted to midline
dose by using a modified Rizzotti
approach [Rizzotti 1985] and then the dose
in the prescription point is calculated by a
simple PDD algorithm. The contributions
of the different beams are summed
- for parotid gland: target absorbed dose by
measurement of entrance dose plus PDD
correction
- entrance dose
- TBI: midline dose distribution (chest,
abdomen, pelv is) by combining diodes
and portal films (transit dosimetry) data
EDINBURGH
- for initial systematic studies, entrance and exit doses, where possible; typically at the
centre of the field. From these values, target absorbed dose deviations are estimated
- for routine use, typically entrance doses only
- for breast patients, combined entrance and exit doses are measured routinely at a point
midway between field centre and the inner beam edge
- for the repeated test audits, full entrance and exit measureme nts are taken and target
dose deviations estimated
- for electron beams, entrance doses at field centre
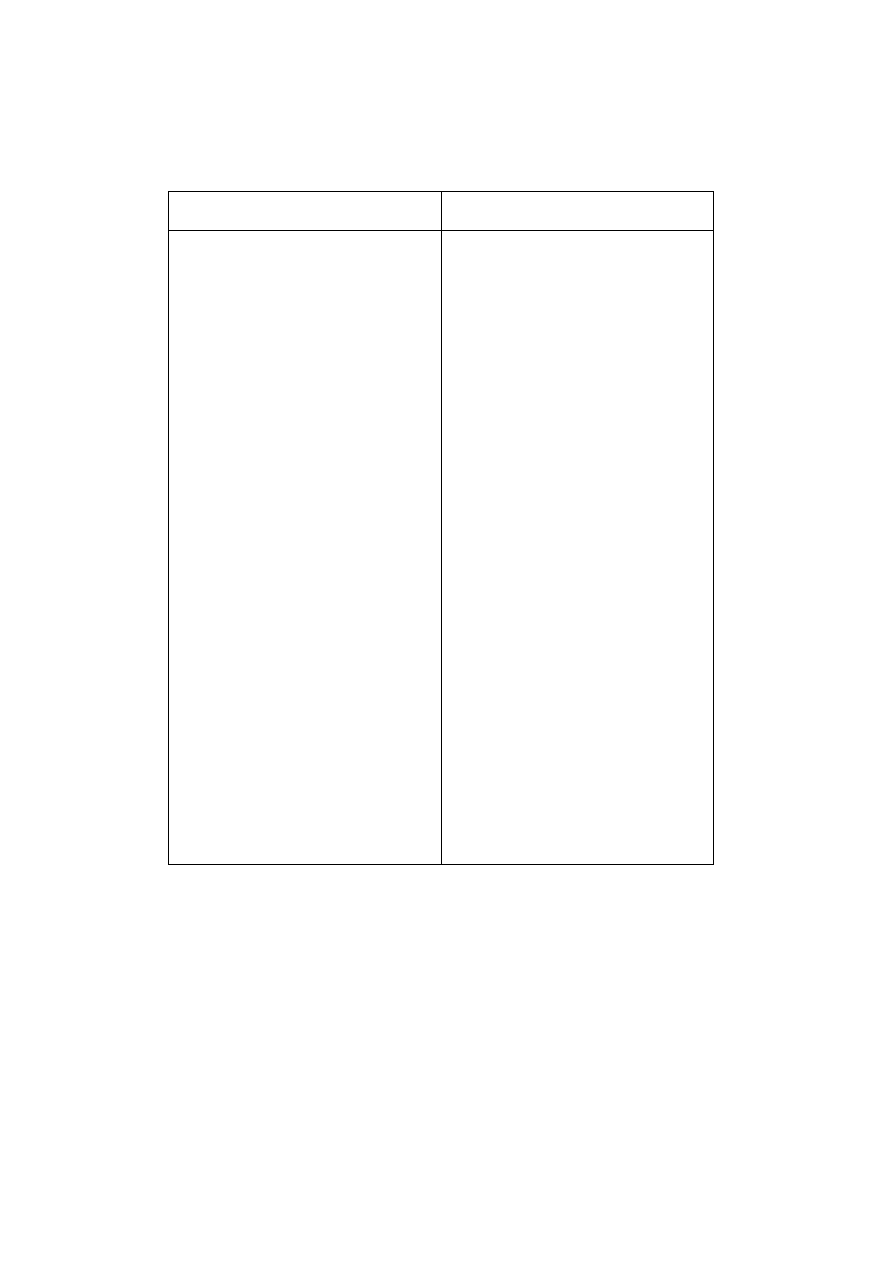
57
4.3 PROCEDURE FOR IN VIVO DOSIMETRY?
4.3.1 CALIBRATION PROCEDURE? WHICH CORRECTION FACTORS ARE USED?
LEUVEN
BARCELONA
Equipment
- polystyrene phantom
Calibration
- ref. conditions:
SSD 100 cm,
field size 10 x 10 cm
2
- for absolute dose determination with the
ionisation chamber, the Dutch (NCS)
protocol is used, however, without
displacement factor (see Section 1.2)
- TBI: calibration factors in TBI conditions
Correction for
- temperature (only for TBI)
- SSD, field size, wedge, tray
Equipment
- polystyrene phantom
- Plastic Water
TM
phantom (CIRS)
- water phantom equipped with thermostat
Calibration
- ref. conditions: SSD 100 cm, 22.5°C
field size 10 x 10 cm
2
- for absolute dose determination with the
ionisation chamber, the Spanish protocol
is used, however, without displacement
factor (for calibration of entrance dose
measurements) (see Section 5.1.2)
- TBI: entrance and exit calibration factors in
TBI conditions
Correction for
- temperature (only for TBI)
- entrance: field size, SSD, tray, wedge,
directional dependence
- exit: none (< 1%)
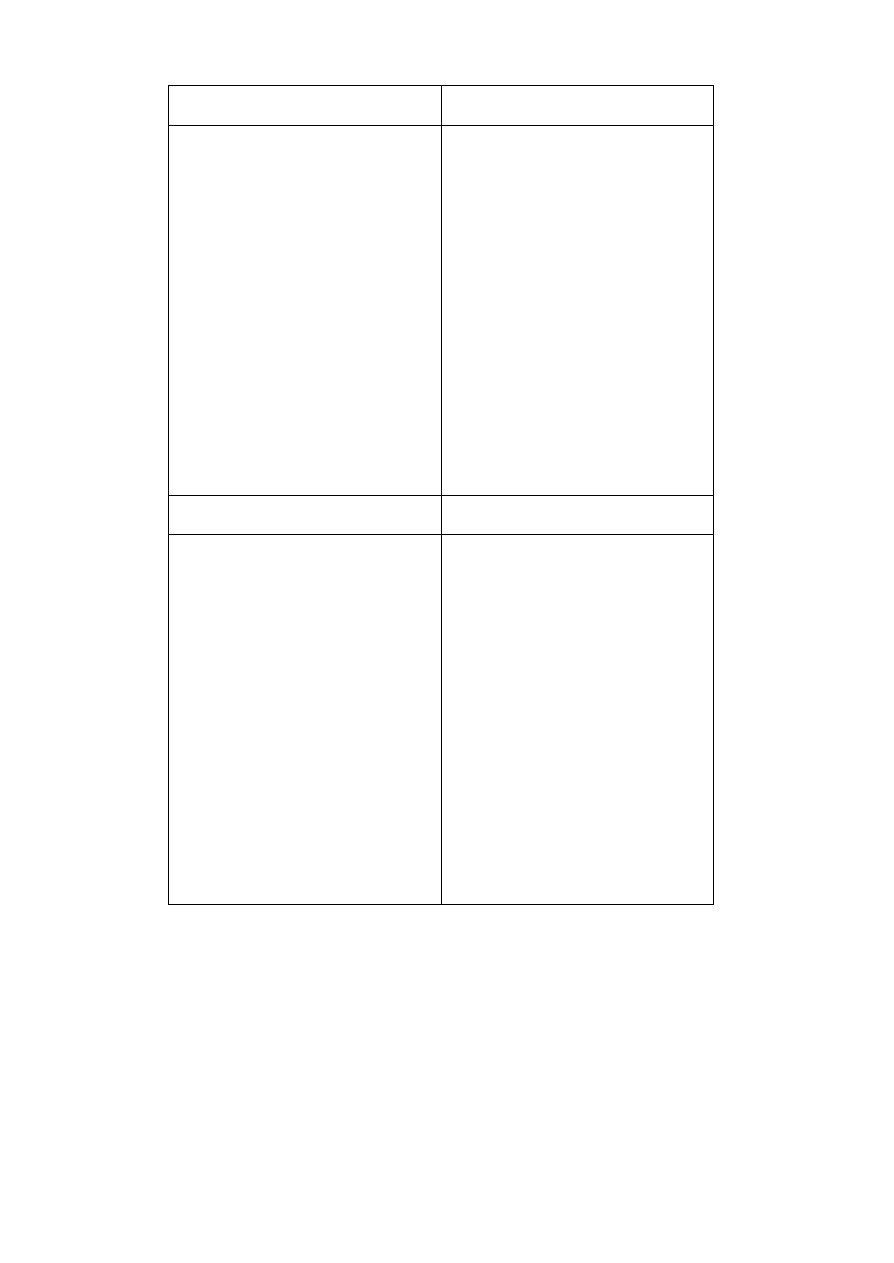
NANCY
COPENHAGEN
Equipment
- polystyrene phantom
Calibration
- ref. conditions:
SSD 100 cm,
SSD
60
Co 80 cm
field size 10 x 10 cm
2
- TBI: entrance calibration factors in TBI
conditions
Correction for
- variation of response of exit detector with
dose rate
- wedge correction fa ctor
Equipment
- Solid Water
TM
phantom ( RMI 457)
Calibration
- initially against NE Farmer chamber
- periodic calibrations: against the Clinac
monitor chamber in connection with
output check of the treatment machine
Correction for
- field size, SSD, tray, layers of
compensation filter, temperature and
directional dependence (no wedge
correction because of dynamic wedges)
AMSTERDAM
MILANO
Equipment
- polystyrene phantom
Calibration
- ref. conditions: SSD 100 cm
field size 15 x 15 cm
2
15 cm thick phantom
- Dutch (NCS) protocol without
displacement factor
Correction for
- patient thickness, SSD, field size, wedge +
shift of measurement point in wedge
direction [Essers 1994], angle, air gap,
Equipment
- acrylic phantom
Calibration
- ref. conditions: SSD 100 cm,
field size 10 x 10 cm
2
- TBI: treatment conditions
Correction for
- SSD, field size, wedge, tray,
directional dependence, (temperature)
- TBI: off-axis
59
carbon fibre table, temperature
EDINBURGH
Equipment
- Solid Water
TM
phantom (RMI 457)
Calibration
- ref. conditions, 100 SSD, 15 x 15 cm
2
field, 15 cm thick phantom
- absolute dose determination using calibrated ionisation chamber using UK protocol:
for entrance dose calibration, take out the displacement correction
for exit dose calib ration, add in an average ‘build -down’ correction
Correction for
- measured for every parameter: e.g. SSD, field size, phantom/patient thickness, directional
dependence, temperature, wedge, tray, (for both entrance and exit initially)
- build-up caps used on diodes to minimise the range of values of correction factors
- detailed correction factors used for initial systematic studies and for audits
- for routine use, mid -range correction factors for the irradiation parameters used for a
specific technique and treatment machine are combined into ‘generic’ correction factors
to be applied for that particular treatment and machine
4.3.2 WHICH MEASURED AND EXPECTED DOSES ARE COMPARED?
LEUVEN
BARCELONA
- the expected entrance dose is the dose
calculated by the TPS
- the expected doses (entrance, exit and
ICRU point) are the doses calculated by
the TPS;
- for electrons, the expected dose is the
dose calculated at dose maximum (which is
also the prescribed dose)
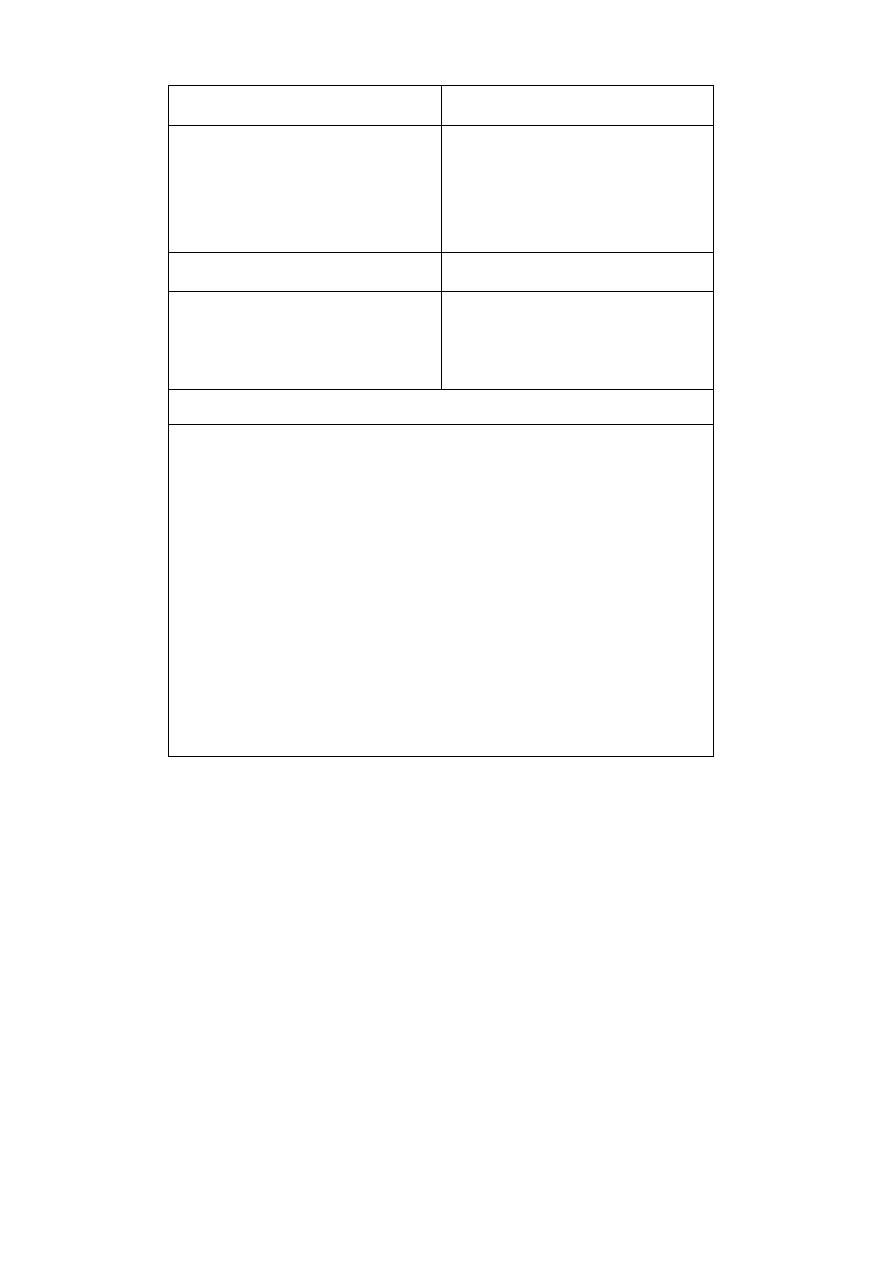
NANCY
COPENHAGEN
- the expected dose is the dose calculated at
the ICRU dose specification point, or the
prescribed dose, if there is no isodose
distribution available
- the expected entrance dose is the dose
calculated either with an independent
spread sheet program or by the TPS
AMSTERDAM
MILANO
- the exp ected dose is the target absorbed
dose, calculated with the TPS
- the expected entrance dose is calculated
by an independent formula
(implemented on PC)
EDINBURGH
- the expected entrance dose is either that from the TPS, or calculated manually,
dependin g on treatment
- the expected exit dose is from the TPS, or calculated manually depending on treatment
- the expected target volume dose is that calculated at the specification point, or the
prescribed dose if there is no isodose distribution (including electrons)
- for breast the expected dose is taken from the plan at 1.5 cm below the diode
measurement point
- for routine use, expected diode reading ranges (expected reading is expected dose
divided by calibration factor and by generic correction factor) are supplied to the
treatment machine by physics/planning, so that the radiographers only have to tick a
box that the reading is within range or not
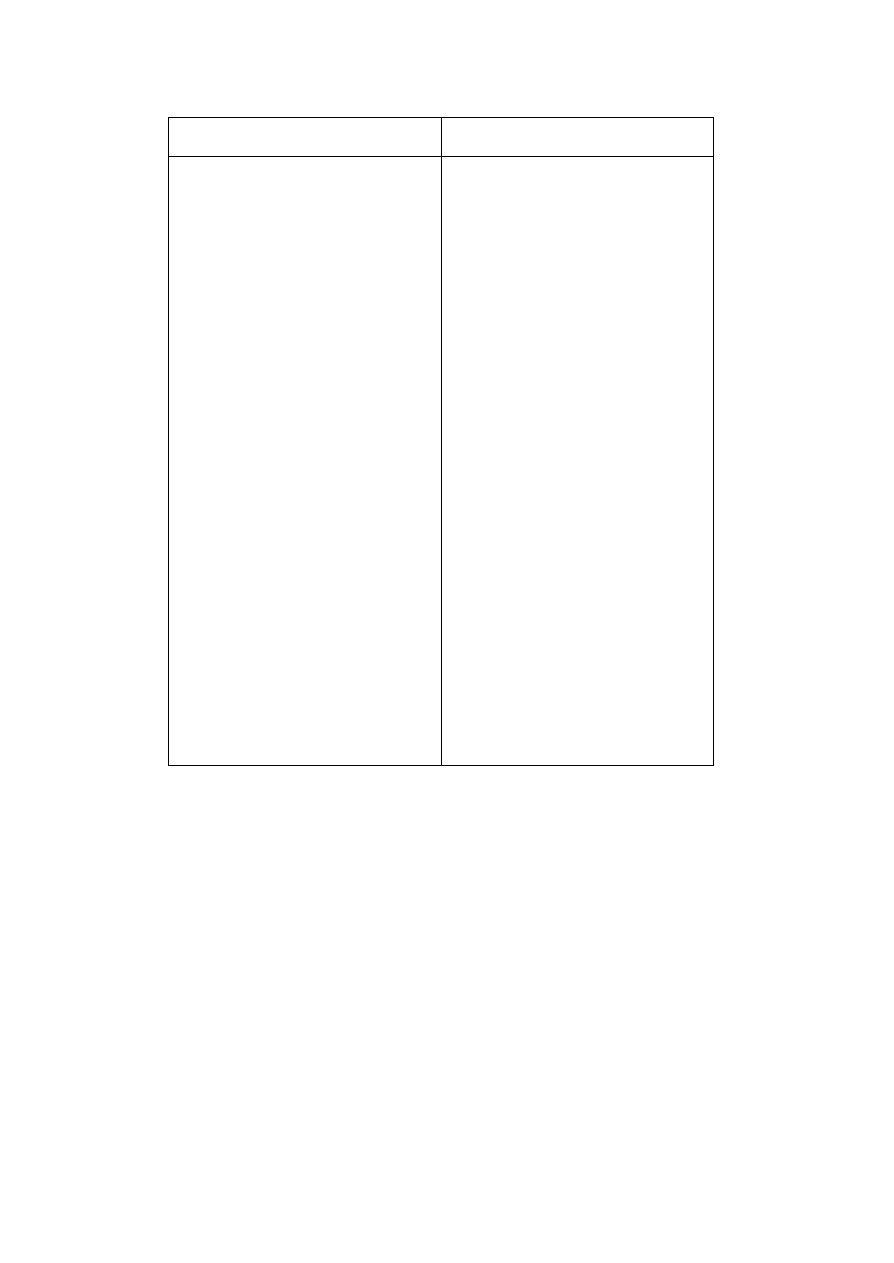
61
4.3.3 VALUE OF TOLERANCE AND ACTION LEVELS + ACTIONS UNDERTAKEN
LEUVEN
BARCELONA
Tolerance level:
5 % for 6 MV
10 % for 18 MV
1st action level:
5 % for 6 MV
10 % for 18 MV
2nd action level:
10 % for 6 MV
15 % for 18 MV
Actions
Cfr. Flow chart of Figure 2.2
Tolerance level: 5 %
Action level: 5 %
Actions
immediate action:
∆ ≥ 5 %
- radiographer
- immediate check of treatment parameters
(MU, field geometry, patient position,
movement of diode)
a posteriori action
∆ ≥ 5 %
- check of all parameters
- IVD at the next treatment session
- if
∆
≥
5 % persists: simulation of treatment
with Plastic Water
TM
phantom, with diode
and ionisation chamber at the same time
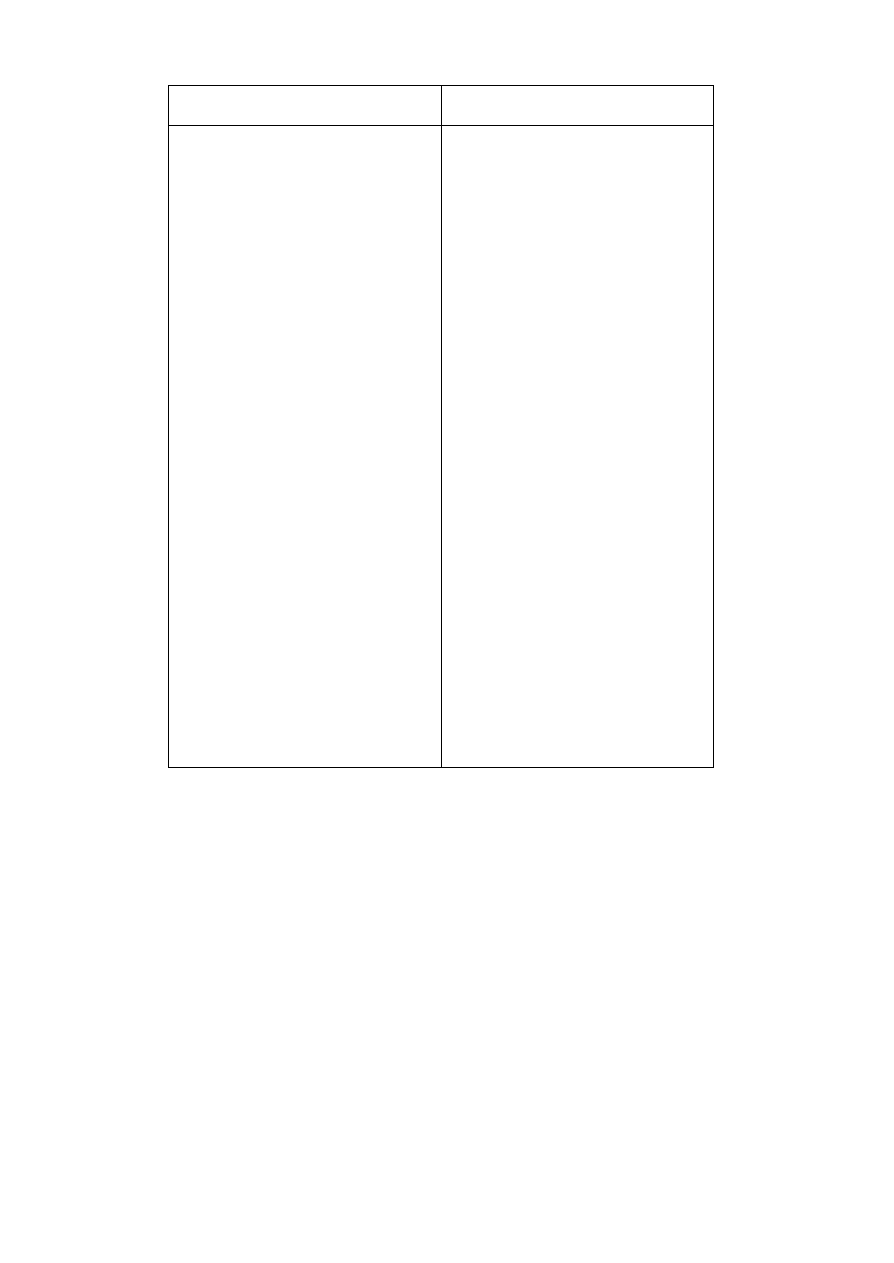
NANCY
COPENHAGEN
Tolerance level:
5 %
1st action level: 5 %
2nd action level: 10 %
Actions
Immediate action:
∆ (entrance dose) ≥ 10 %
- radiographer (+ physicist)
- immediate check of treatment parameters
a posteriori action (physicist):
∆ (target dose) ≥ 5 %
∆
≤
10 %
- verification of the MU calculation
- thorough investigation of all treatment
parameters
request for IVD at the next treatment
session
∆
≥
10 %
request for IVD at the next treatment
session in presence of physicist
Tolerance level: 5 % or 8% depending on
complexity of treatment
Tolerance and action levels coincide.
Actions
- check of quality control pro cess
(calculation of the expected dose,
positioning of the diode, practical
problems)
- check of treatment preparation process
(dose calculation and treatment chart data)
- repeat diode measurement
- if deviation persists: simulation of
treatment with Solid Water
TM
phantom,
with diode and ionisation chamber at the
same time.
AMSTERDAM
MILANO
Tolerance level:
- 2.5 % for the prostate
- 4.0 % for the parotid gland
Action level:
- 2.5 % for the prostate
- 4.0 % for the parotid gland
Actions
- immediate check of treatment parameters
- a third measurement is performed if only
one measurement, and the average, is
exceedingthe action level
- if deviation persists: patient dose (MUs) is
always corrected for the other treatment
fractions and the origin is traced by
additional phantom measurements and
calculations with the TPS
Tolerance level:
- 5 %
- 7 % for tangential wedged fields
Action level:
- 5 %
- 7 % for tangential wedged fields
(see Section 5.5)
Actions
immediate check (technician):
- always an independent check of treatment
parameters (including SSDs): the operator
performing the check is different from the
radiographer who sets up the patient
a posteriori action (physicist):
∆ ≥ 5 %
(7 % for tangential wedged fields)
- check of all parameters (data transfer, dose
and MU calculation)
- IVD at the next treatment session
if
∆
≥
5 % persists, possible measurement
in acrylic phantom with ionisation
chamber (and diode)

64
EDINBURGH
Tolerance and action level:
- 5% for genera l routine use for individual entrance measurement
- 8% for individual exit dose
- 5% for target dose from combination of beam measurements
- 2.5% for conformal radiotherapy treatments (prostate)
For routine use, the expected reading range is the appropriate tolerance applied above
and below the expected reading, as in question 3b.
Actions
- immediate check of treatment parameters (radiographer and physicist)
- check that not significantly non-standard, such that generic correction may not apply
(physicist)
- before next treatment check plan, MU calculation, treatment record, treatment data,
etc. (physicist)
- carry out repeat diode measurement on next treatment fraction, check diode position,
problems of set-up, positioning, etc.
- if deviation persists, test diode measurement against ion chamber in phantom
65
4.3.4 TIME PERIOD BETWEEN CHECKS OF CALIBRATION AND CORRECTION
FACTORS
LEUVEN
BARCELONA
Calibration
- every month
Correction factors
- once a year
Calibration
- every 50 Gy of accumulated dose
- TBI: every four TBIs
- electrons: in evaluation
Correction factors
- temperature: every 6 months
- FS, tray, wedge, angle: every year
NANCY
COPENHAGEN
Calibration
- once a week
- TBI: before every first session
Calibration
- every third month
Correction factors (in evaluation)
AMSTERDAM
MILANO
Calibration
- every two weeks, depending on the
amount of accumulated dose
Correction factors
- twice a year
Calibration
- every month
Correction factors
- once a year
EDINBURGH
66
Calibration
test calibration quarterly; but beginning to use diodes as routine daily treatment machine
dose consistency check. In this case, checked versus ion chamber weekly
Correction factors
annually, or if unexpected changes in calibration
4.4 WHAT SYSTEM DO YOU USE FOR THE RECORDING OF IN VIVO DOSE
MEASUREMENTS?
LEUVEN
BARCELONA
- manual recording of the diode signal on a
separate in vivo sheet
- manual recording of the measurements on
a separate in vivo sheet (not included in
patient record) with relevant information:
- field size, wedge, tray, SSD
- ICRU point depth
- PDD at ICRU point depth
- PDD at entrance
- PDD midplane
- PDD at exit
for pelvic treatments and TBIs, the
measurements are entered in a “Excel
Book” containing the correction factors,
with the irradiation parameters and the
expected doses;
the corrected doses and the deviations
between expected and measured entrance,
exit and prescribed doses are calculated
automatically; statistical analysis of the
data is performed automatically
67
NANCY
COPENHAGEN
- manual recording of the measurements in
the treatment chart (relevant information
entered in a file by the physicist):
-
localisation
-
treatment unit
- manual recording of the measurements
and relevant beam data in a database for
statistical evaluation
-
treatment technique
-
beam geometry
-
wedge
-
immobilisation technique
-
ratio meas./calc. entrance dose for
each field
-
ratio meas./calc. target absorbed
dose for whole treatment session)
future implementation of recording in record
and verify system
TBI: measurements are recorded in real time
from the electrometer and measured
absorbed doses at 7 points of interest
are computed by home -made PC
software
AMSTERDAM
MILANO
- the diode measurement system prepares a
diode measurement file for every patient
field, containing beam, patient and diode
parameters (for instance calibration and
correction factors are determined for each
- manual recording of the in vivo dosimetry
results with a number of relevant
information (see Section 5.5)
- periodic update of Excel files for statistical
analysis
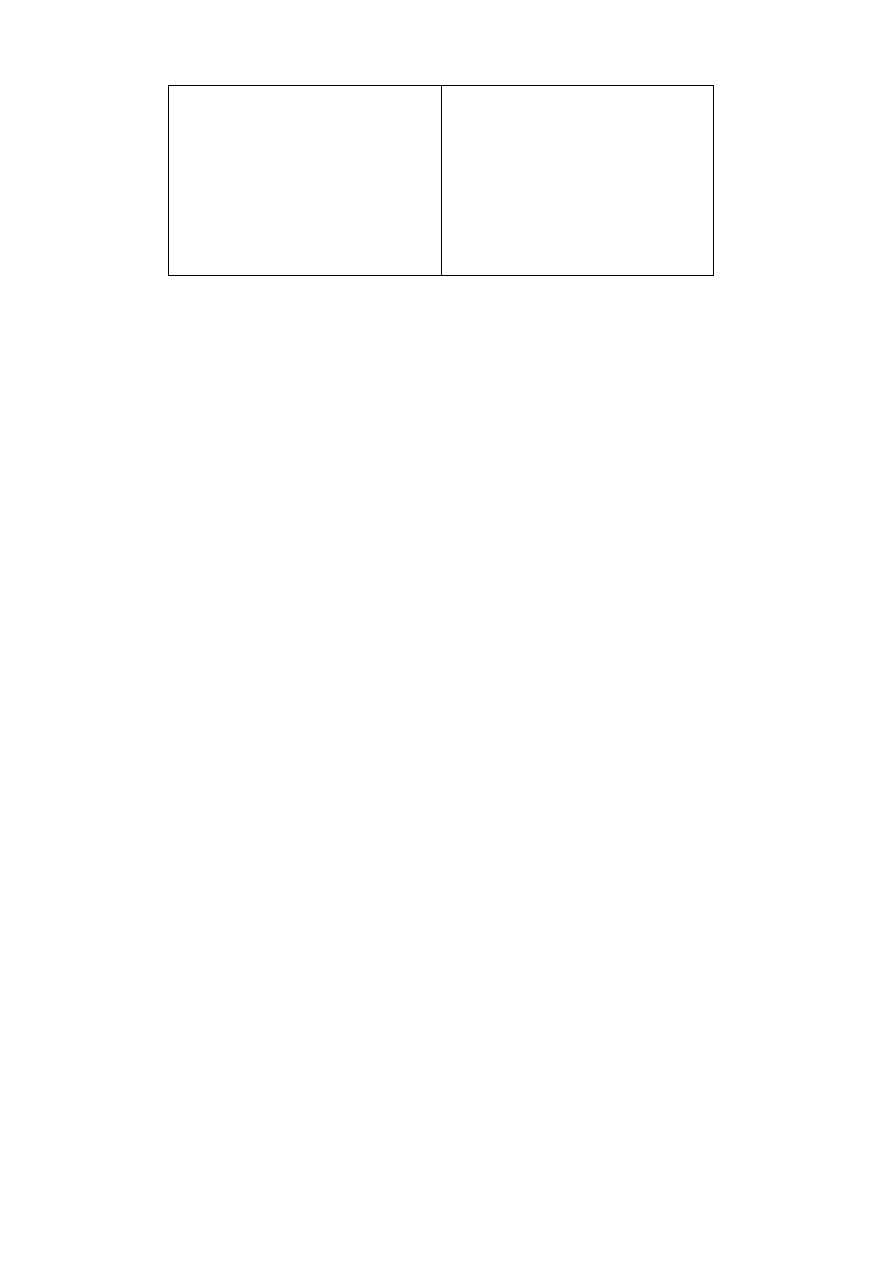
68
diode using look-up tables and simple
formulas e.g. ISQL for the presence of air
gaps)
- these diode measurement files are stored
on hard disk
analysis
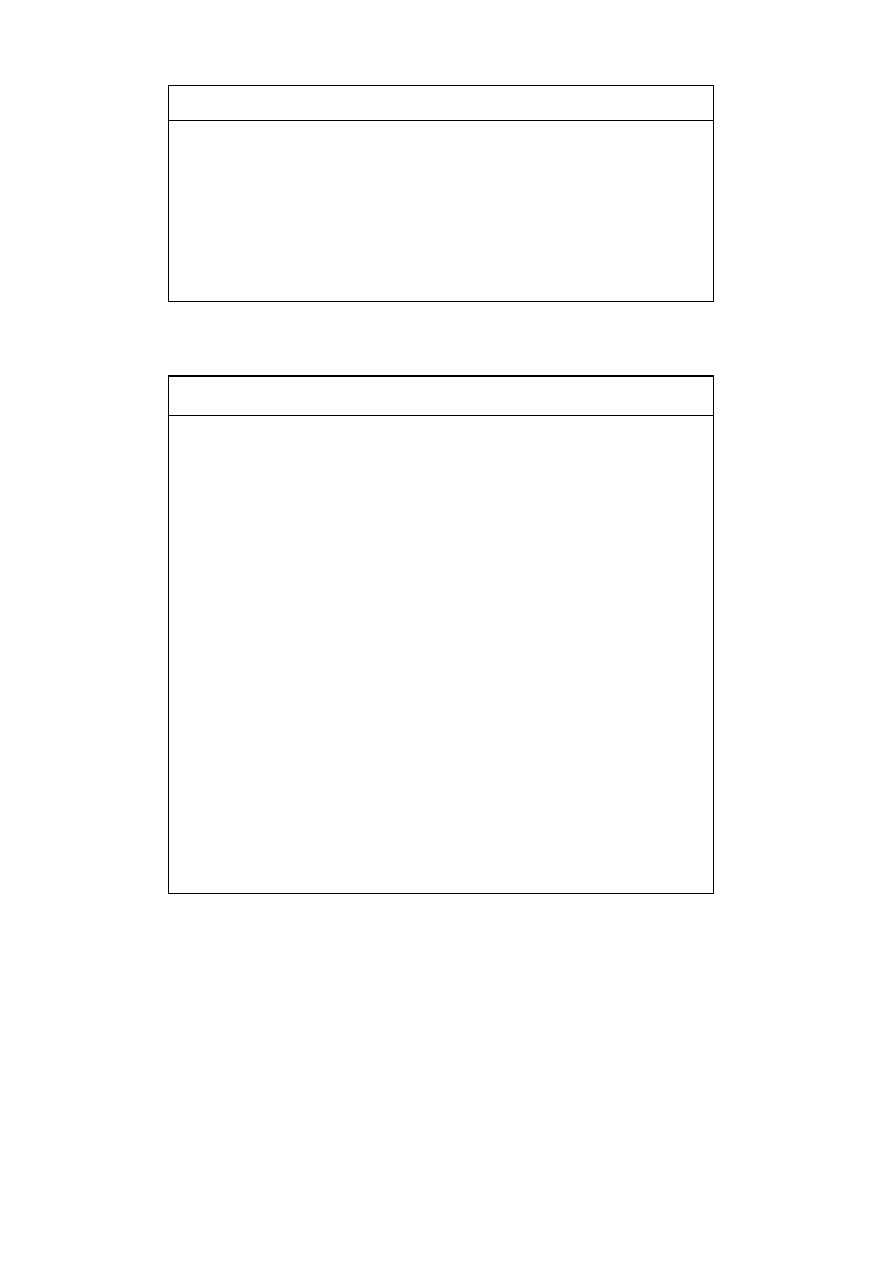
EDINBURGH
- for systematic measurements and for full audits, manual recording of results on
separate in vivo sheet
- for routine use, expected reading range is recorded on the treatment sheet (in a short
in vivo section) and the radiographers check a tick box
If not within the expected range, the sheet is drawn to the attention of the physics
group
4.5 WORKLOAD? SPECIFIC TASKS OF PEOPLE INVOLVED?
LEUVEN
- implementation/ maintenance related tasks
- initial acceptance/calibration/
QA person in charge
10 hours/diode
correction factors
- periodic calibration
QA person in charge
45 min/diode
- periodic determination
QA person in charge
4 hours/diode
of correction factors
- training of radiographers
QA person in charge
- patient related tasks
- calculation of expected
dosimetrist
3 min/patient
diode signal
- measurements
radiographer
3 min/patient
- out-of-tolerance analysis
QA person in charge
1 hour/week
+ physicist
for 2000 patients/year
- TBI (single)
physicist
1 hour
- TBI (fractionated)
physicist
5 min/session

70
BARCELONA
- implementation/ maintenance related tasks
- initial acceptance/calibration/
physicist
4 hours/diode
correction factors
- periodic calibrations
physicist
30 min/2 weeks
- training of radiographers
physicist
and dosimetrists
- patient related tasks
- recording in in vivo sheet for
dosimetrist
10 min/patient
every field FS, ICRU point depth,
PDD at ICRU point, at entrance,
at midplane, and at exit
- measurements
radiographer
3 min/patient
- recording of data in Excel book
physicist
5 min if there are
and daily evaluation
no problems
- TBI (hyperfractionated)
physicist
45 min during 3 days
NANCY
- patient related tasks
- measurements
radiographer
3 min/patient
- evaluation
physicist
1 hour/day
- TBI
physicist
10 min/session
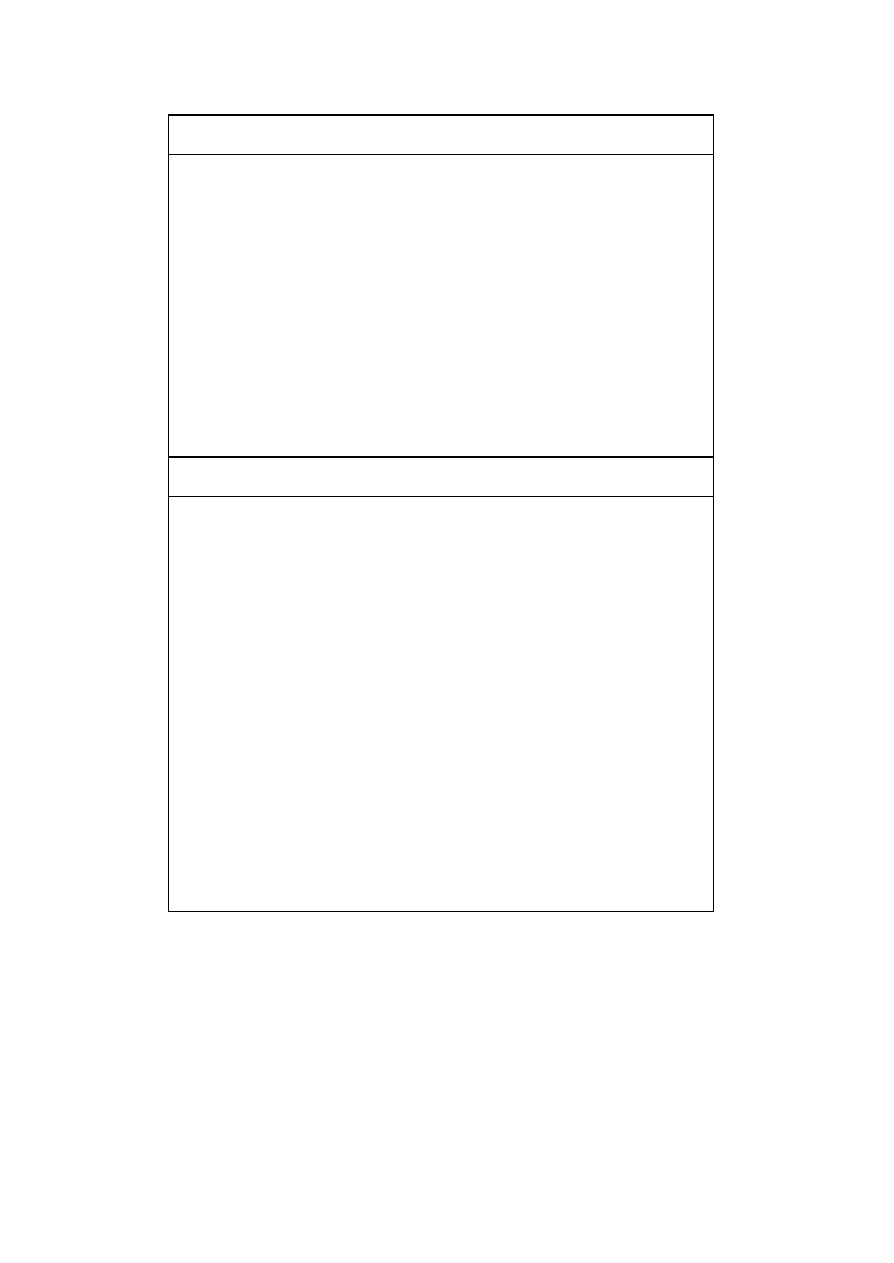
71
COPENHAGEN
- implementation/ maintenance related tasks
-
initial calibration procedures
QA physicist
5 hours/diode
-
periodic calibration
QA physicist
10 min/diode
-
training of involved personnel QA physicist
30 min/month
- patient related tasks
-
calculation of expected signal dosimetrist
5 min/patient
-
measurements
radiographer
3 min/patient
- out-of-tolerance analysis,
physicist
average 5 min/patient
documentation, evaluation
AMSTERDAM
- total workload
0.4 full time equivalent (2 days work/week)
- time per patient
4.4 hours
- making appointments
12 min
- measuring (twice) + waiting;
120 min
the measurement itself takes up to
5 min
- analysis
30 min
- additional measurements
18 min
- storing of data
30 min
- implementation of corrected MU
6 min
- analysis of discrepancies
48 min
- additional time per week
- phantom tests
2 hours
- administration
1 hour
- consultation with co-workers
2 hours

72
- consultation with co-workers
2 hours
MILANO
- implementation/ maintenance related tasks
-
initial calibration procedures
physicist + t echnician
4-6 hours/diode
-
periodic calibration
physicist + technician
10-15 min/month/diode
- patient related tasks
-
patient data collection
technician
5-10 min/patient
-
measurements
technician
5-15 min/patient
-
entrance dose calculation,
physicist
average 5 min/patient
comparing to measured dose
- data analysis
physicist + technician
up to 1 hour/patient
(including transit dosimetry,
routinely for TBI patients)
- TBI measurement
technician
1 hour/patient
EDINBURGH
- implement ation/ maintenance related tasks
- initial acceptance/calibration/ physicist/physics technician
5 hours/diode
correction factors
- periodic calibrations
physicist/physics technician
1 hour/quarter
year/diode
- patient related tasks (routine use)
- calculate expected signal
physics/planning personnel a few minutes
measurements
radiographer
less than 5 min/patient*
- Co-ordination currently by part -time research radiographer/dosimetrist seconded to
the
physics group.
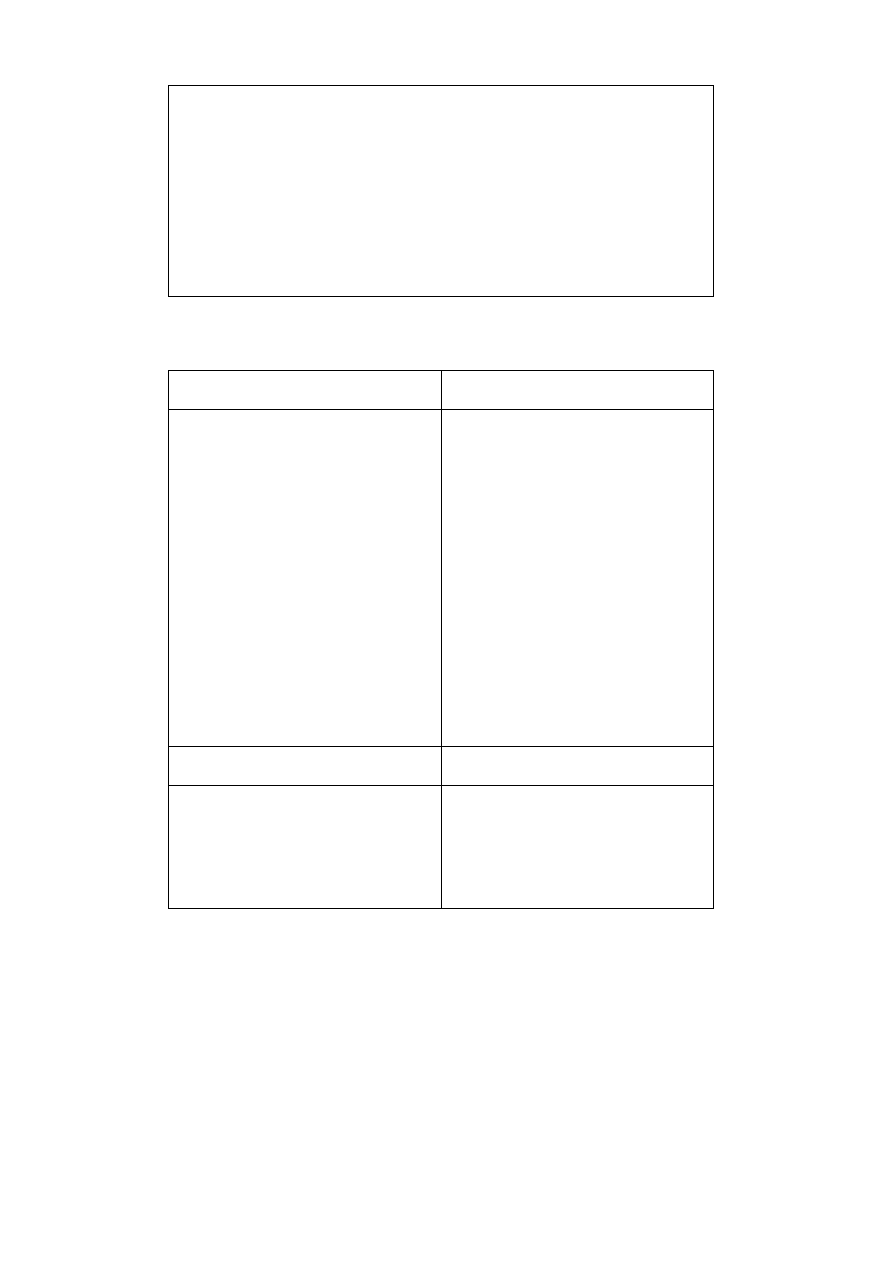
73
the
physics group.
-* methodology designed so that this is in parallel with other tasks, i.e. adds minimal
time
to patient treatment
- systematic studies and audits
Physicists and seconded trainees/project students (including physics, radiographers,
radiation oncologists). Significant times involved.
4.6 EXAMPLES OF PRACTICAL PROBLEMS?
LEUVEN
BARCELONA
- wrong entrance dose calculation by TPS
- some important errors are not traced by in
vivo dose measurements (for instance
errors in TPS target dose, since the
expected entrance dose is the one
calculated with the TPS)
- use of a polystyrene phantom (for
calibration, determination of correction
factors, determination of Rizzotti curves
and of correction factors for midplane
calculation) instead of a water phantom
- use of cerrobend (block) correction factor
- exit correction factors: how can they be
measured to guarantee independence of
factors and independence of the phantom
thickness?
- non-symmetric heterogeneities
NANCY
COPENHAGEN
- positioning of diodes:
- chest wall irradiation
- in presence of immobilisation
device, use of support (head support, ...)
- positioning of diodes:
- presence of immobilisation
- near blocks
- half-beam technique with wedges
74
- near blocks
- small fields (exit diode)
- estimation of midline dose:
-
presence of wedge
-
presence of heterogeneities
-
isocenter not situated at mid -depth
-
non-opposed beams
-
different X-ray energy used for the
same patient (ant 6 MV/post10
MV)
- mounting of equipment:
convenient handling of the diodes and the
cables
- calibration:
difficulties with narrow sensitivity range
of electrometers => improper matching to
the diode sensitivity (during
implementation)
AMSTERDAM
MILANO
all encountered problems turned out to be
real problems with the treatment planning
system or the performance of the linear
accelerator
action level for tangential wedged beams
modified with time after statistical analysis
EDINBURGH
- positioning on some surfaces, particularly on steep angles
- measurement problems when the beam is incident through the couch or head support,
etc.
- what temperature correction should be applied in certain situations
- measurements below bolus
- measurements close to blocks (particularly CRT blocks), asymmetric fields, etc.
- limitation of resolution of electrometer in small reading situations, particularly for small
wedged components of fields on motorised wedge machines
- handling of diodes and cables in rooms where our ceiling mounted support is not yet
installed: particularly connector failures

75

76
CHAPTER 5
EXPERIENCES FROM DIFFERENT RADIOTHERAPY
CENTRES
In order to provide more detailed examples regarding the implementation and the
functioning of in vivo dosimetry in clinical routine, we have selected contributions from the
authors’ institutions about an aspect of in vivo dosimetry that they have worked on
specifically. Some contributions offer reference data concerning basic procedures, from
diode calibration to evaluation of the measurements; others contain specific suggestions
for improvement or refinement of procedures. More details and data can be found in [Jornet
2000], [Lööf 2001], [Georg 1999] and [Fiorino 2000].
5.1 CALIBRATION AND MEASUREMENT PROCEDURES – THE BARCELONA
EXPERIENCE
This section lists detailed examples of methods and results of the calibra tion procedures,
as explained in Section 1.2, performed in the radiotherapy department of the Hospital Santa
Creu I Sant Pau in Barcelona. A recent study [Jornet 2000] concentrates on the
performance of p-type and n-type diodes in high energy beams, which will be elucidated in
some detail in this overview (see also Section 5.2).
5.1.1 TESTS PERFORMED BEFORE DIODE CALIBRATION
Due to the way diodes are made, two diodes even from the same fabrication batch may
behave differently when irradiated. Therefore it is recommended to perform some tests
before using them in routine. The results of these tests should be compared with the
technical specifications provided by the manufacturers.
The tests performed whenever a new diode is received in our centre are:
1. Signal stability after irradiation
2. Intrinsic precision
3. Study of the response/dose linearity
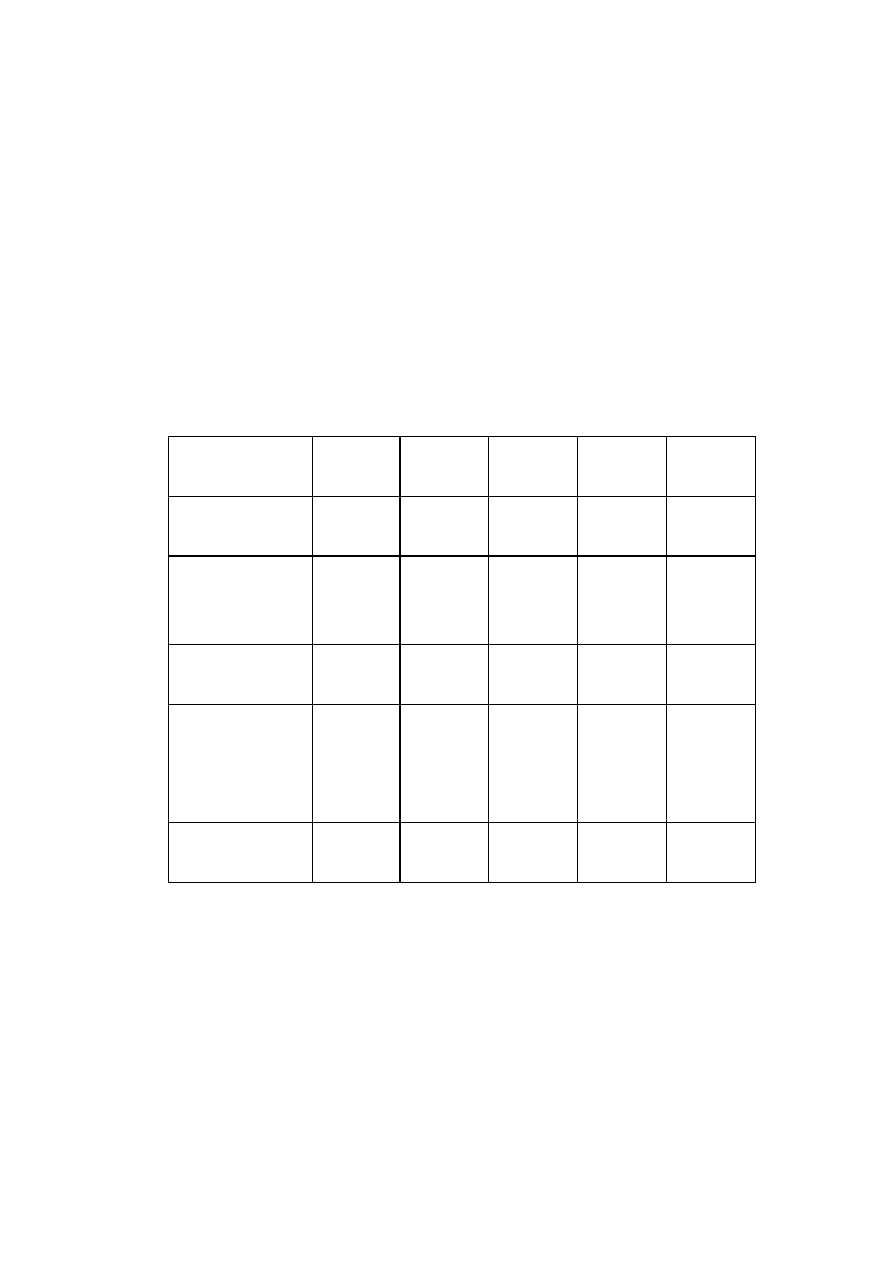
77
4. Verification of the equivalent water depth of the measuring point (water
equivalent thickness of the build -up cap)
5. Perturbation of the radiation field behind the diode
Some tests (4 and 5) are only performed for the first 3 or 4 diodes of a particular type. All
diodes are connected to the same channel of the electrometer to avoid drifts and loss of
signal, which depends on the channel to which they are connected. All channels of the
electrometer are checked regularly. The measurements corresponding to these tests are
performed at reference conditions (i.e. collimator opening 10 cm x 10 cm, phantom surface at
the isocentre). For most of the tests the diode is fixed on the surface of a plastic phantom,
i.e. a Plastic Water
TM
phantom (CIRS).
The results of the tests for different diodes are summarised in Table 5.1.
EDP-10
(6 MV)
EDP-30
(18 MV)
P30
(18 MV)
QED
(18MV)
Isorad-p
1
(18MV)
1 stability after
irradiation (5 min)
0.3 %
-0.58 %
0.33 %
-0.06 %
-0.20 %
2. intrinsic precision
(SD)
(10 irradiations)
0.06 %
0.16 %
0.05 %
0.07 %
0.10 %
3. linearity
response/dose (r
2
)
1.0000
(0.2 - 7 Gy)
1.0000
(0.2 – 7 Gy)
1.0000
(0.2 - 3.5 Gy)
1.0000
(0.2 - 7 Gy)
1.0000
(0.2 – 7 Gy)
4. depth of diode
measuring point
(water equivalent
depth)
0.80 cm
1.4 cm
3.0 cm
2.2 cm
3.3 cm
5. dose decrease at 5
cm depth
6 %
3 %
9 %
6 %
14%
1
designed with a cylindrical build -up cap

78
Table 5.1 Overview of the results of the initial tests for different types of diodes
5.1.1.1 SIGNAL STABILITY AFTER IRRADIATION
The signal immediately aft er irradiation is compared to the signal five minutes after the end
of the irradiation. Five minutes is considered as the average of the time periods
encountered in clinical practice.
5.1.1.2 INTRINSIC PRECISION
The standard deviation of 10 readings of 100 MU each is calculated.
5.1.1.3 STUDY OF THE RESPONSE/DOSE LINEARITY
We verify that the response is linearly proportional to the absorbed dose for clinical
significant doses. As we verify the linearity between MU and dose regularly, we verify the
linearity of the system diode-electrometer between 15 and 600 MU.
5.1.1.4 VERIFICATION OF THE WATER EQUIVALENT DEPTH OF THE MEASURING
POINT
The diode is fixed on the surface of the Plastic Water
TM
phantom and covered with a
special Plastic Water
TM
slab to avoid air gaps (Figure 5.1). Irradiations with X-rays are
performed while adding Plastic Water
TM
slabs on top of the diode until the reading reaches
a maximum. As the depth of dose maximum in water at these irradiation conditions is
known, the water equivalent thickness of the build -up cap can be calculated (Figure 5.2).
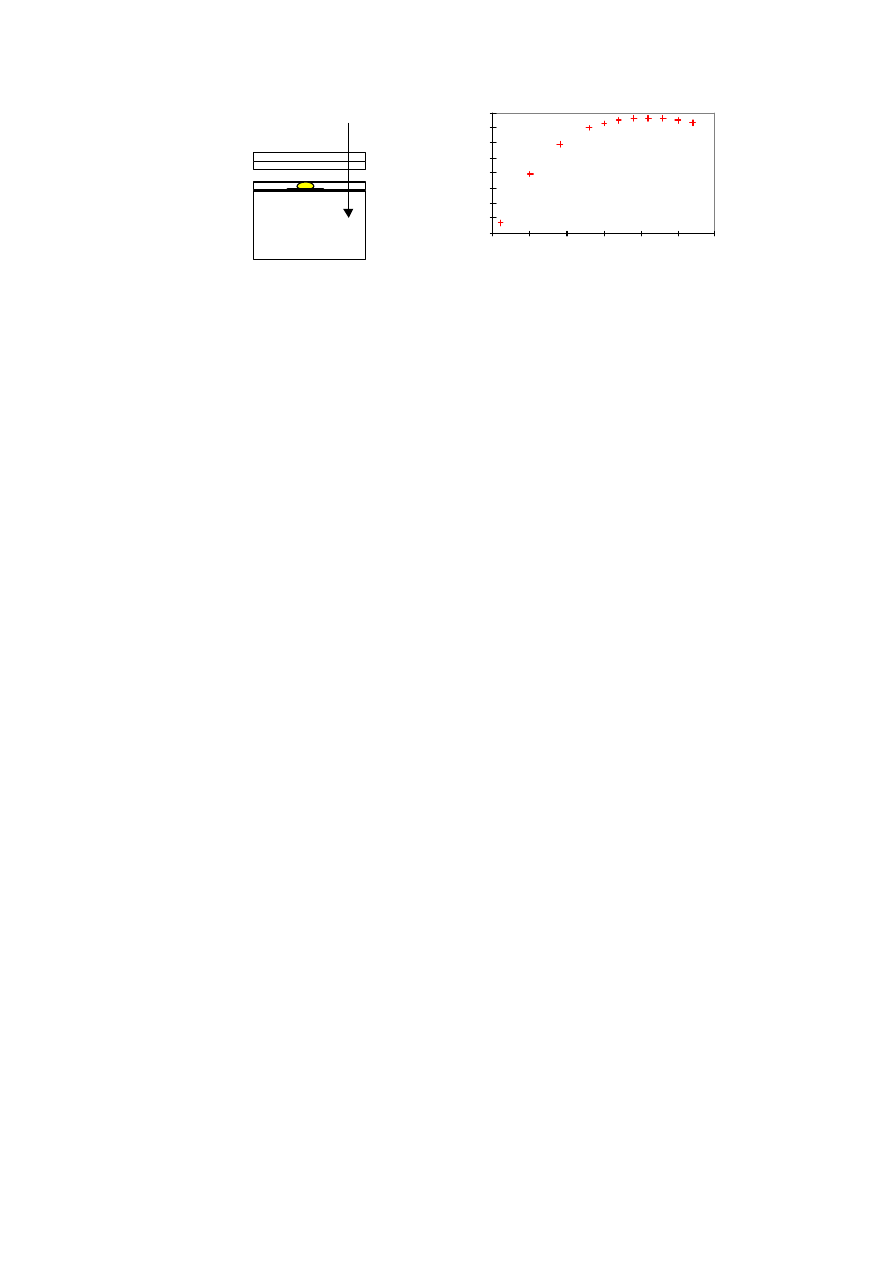
79
Figure 5.1 Experimental set-up for the
determination of the water equivalent
thickness of the build-up cap
Figure 5.2 Diode signal at 18 MV as a
function of the thickness of the Plastic
Water
TM
slabs on top of an EDP-30 diode.
The depth of dose maximum for a 10 x 10
cm
2
field and 18 MV X-rays is 3.5 cm, so
the water equivalent thickness of the
build-up cap of EDP30 is 1.4 cm
5.1.1.5 PERTURBATION OF THE RADIATION FIELD BEHIND THE DIODE
One X-Omat V Kodak film is placed inside a Plastic Water
TM
phantom at 5 cm depth. The
diode is fixed on the surface of the phantom and an irradiation is performed. Another film is
exposed under the same conditions, but without the diode. The dose decrease at 5 cm
depth underneath the diode is calculated by comparing the two beam profiles at this depth.
We use a film scanner (Scanditronix, an option of our field analyser RFA -300) to obtain
beam profiles. It has a spatial resolution of 0.1 mm.
5.1.2 DIODE CALIBRATION (ENTRANCE DOSE)
Diodes are calibrated against an ionisation chamber placed at the depth of dose maximum
inside a plastic phantom (polystyrene or Plastic Water
TM
). The cylindrical ionisation
1.46
1.48
1.5
1.52
1.54
1.56
1.58
1.6
1.62
0
0.5
1
1.5
2
2.5
3
plastic water thickness on top of diode (cm)
diode reading
SSD = 100 cm

80
chamber (0.6 cm
3
) (IC) has a calibration factor traceable to the National Standard Dosimetry
Laboratory in Spain. The diodes are taped on the surface of the phantom near the field
centre, in such a way that they do not perturb the response of the ionisation chamber.
The calibration is performed in reference irradiation conditions (field size at the isocentre 10
x 10 cm
2
, SSD = 100 cm) (see Section 1.2). As the accelerator rooms are equipped with air-
conditioner, the room temperature is always between 21ºC and 22ºC. First, the reading -in-
plastic is converted to a reading-in-water by multiplying the reading-in-plastic with an
experimentally determined factor (in the case of Plastic Water
TM
, this factor is 1). To
determine absolute dose-to-water, the Spanish dosimetry protocol is used. This includes
the application of a displacement factor for entrance dose. As the measurements are not
performed on the exponential part of the curve but at the depth of dose maximum, this
factor is not applied. The calibration factor F
cal
is determined as the ratio of the absorbed
dose determined with the ionisation chamber and the diode reading (see Section 1.2.2).
As the sensitivity of the diodes depends on dose rate, energy and temperature, some
correction factors will have to be applied to the diode reading when measuring conditions
differ from calibration conditions. Some of the correction factors depend, in addition, on
the diode calibration methodology. Since the diode is fixed on the patient’s skin, the scatter
conditions seen by the diode are obviously not the same as the scatter conditions seen by
the ionisation chamber. Therefore a field correction factor, for example, will have to be
applied even if the diode build -up cap is thick enough to guarantee electronic equilibrium.
Furthermore, as the dose rate sensitivity dependence may change with accumulated dose,
the correction factors that account for this dependence, such as the SSD correction factor,
will have to be checked regularly.
We determine the following correction factors:
1. Field size correction factor (CF
field size
)
2. Tray correction factor (CF
tray
)

81
3. Wedge correction factor (CF
wedge
)
4. SSD correction factor (CF
SSD
)
5. Angle correction factor (CF
angle
)
6. Temperature correction factor (CF
temperature
)
In addition, for some types of diodes, we performed tests to assess the importance of the
following issues:
7. Influence of the dose rate on the diode’s sensitivity
8. Sensitivity variation with accumulated dose
The results of the measurements of the entrance correction factors are given in Table 5.4
and Table 5.5
5.1.2.1 FIELD SIZE CORRECTION FACTOR (CF
FS
)
The field size correction factor is defined as:
)
c
(
OF
)
c
(
OF
CF
diode
ic
FS
=
(5)
where OF is:
)
cm
10
(
)
(
)
(
R
c
R
c
OF
=
(6)
with c the side of the square field in cm, and R the reading.
If the measurements of OF
diode
are performed at the same time as the measurements of OF
ic
using a plastic phantom, attention should be paid to OF
ic
because it may differ from OF
ic
measured in water, so a factor to convert reading-in-plastic to reading-in-water should be
applied. This factor will probably depend on field size. To simplify things, one can measure
OF
diode
and compare it with OF
ic
measured in water at the depth of dose maximum.
Field size correction factors obtained for different diodes in different beam qualities are
shown in Figure 5.3 and Figure 5.4.
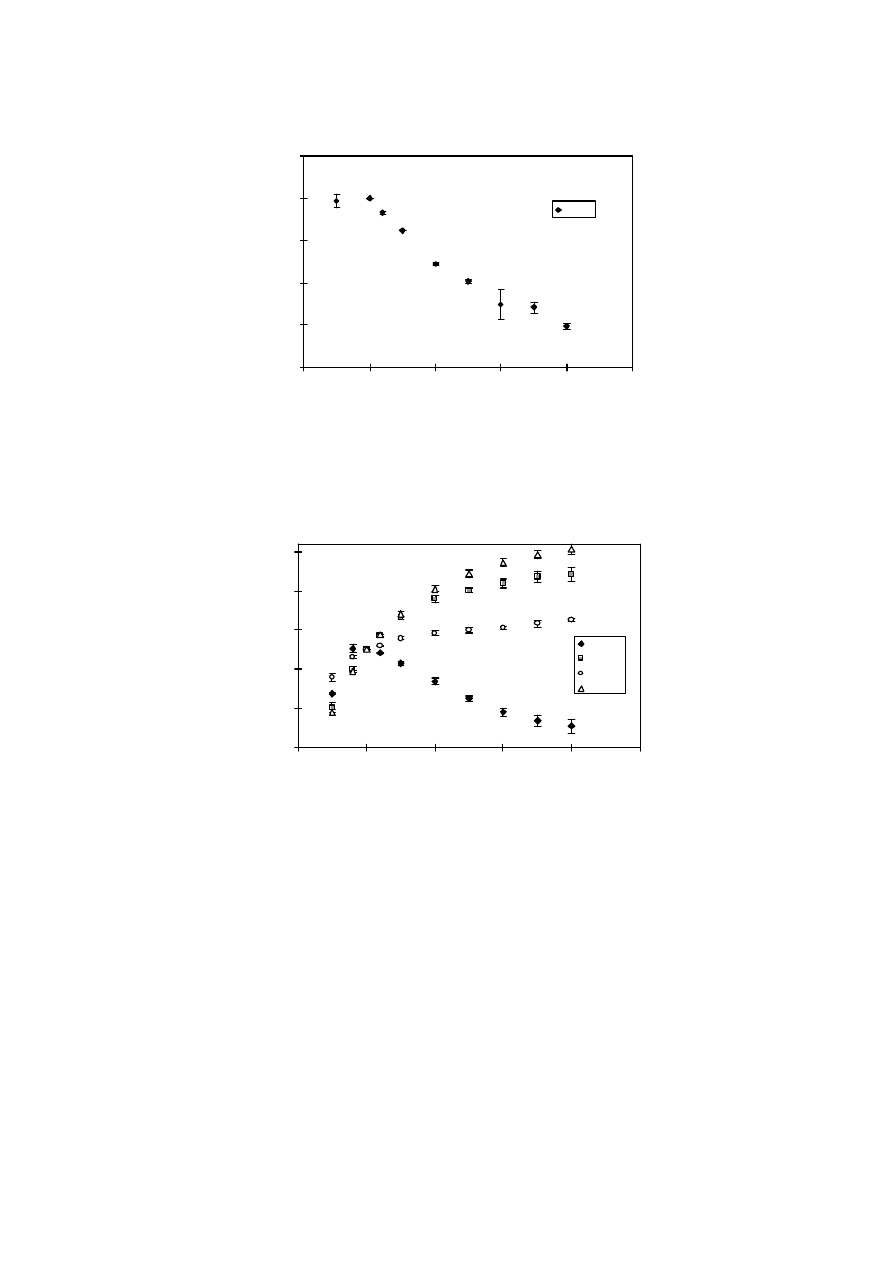
82
Figure 5.3 CF
FS
for EDP-10 diodes and 6 MV X-rays. The mean and SD of measurements
performed with ten diodes are given.
Figure 5.4 CF
FS
for EDP-30, P30, QED and Isorad-p diodes in an 18 MV X-ray beam. The
mean and SD for three diodes of each type and three measurements are shown.
0.980
0.985
0.990
0.995
1.000
1.005
0
10
20
30
40
50
side of square field (cm)
CF
field size
EDP10
0.950
0.970
0.990
1.010
1.030
1.050
0
10
20
30
40
50
side of square field (cm)
CF
field size
EDP30
P30
QED
Isorad-p

83
5.1.2.2 TRAY CORRECTION FACTOR (CF
tray
)
Shielding blocks are positioned on a tray attached to the treatment head. In our hospital,
the tray for the Clinac accelerator is made of PMMA of 0.5 cm thickness. Inserting a tray
between the source and the patient changes the amount of electrons that reaches the
patient’s skin. Therefore, if the diode does not have an appropriate build -up cap, the tray
correction factor varies with field size.
To determine CF
tray
, we measure the tray transmission for different field sizes at the depth
of dose maximum, first with an ionisation chamber and then with the diodes taped to the
surface of the plastic phantom. The transmission factors measured with the ionisation
chamber and with the diodes are compared, and CF
tray
as a function of field size is obtained
(Figures 5.5 and 5.6).
)
c
(
on
transmissi
)
c
(
on
transmissi
CF
diode
ic
tray
=
(7)
Where the transmission is defined as:
)
c
(
R
)
tray
,
c
(
R
)
c
(
on
transmissi
=
(8)
with c the side of the square field in cm, and R the reading.
5.1.2.3 WEDGE CORRECTION FACTOR (CF
wedge
)
Inserting a wedge in the beam results in a decrease of the dose rate and a hardening of the
spectrum of the beam. Therefore, as the sensitivity of the diode depends on both dose rate
and energy, a correction factor different from 1 is expected when using wedges.
The wedge correction factor is defined as the ratio between the wedge transmission factor
for a 10 x 10 cm
2
field, measured with the ionisation chamber placed at the depth of dose
maximum, and the wedge transmission factor for the same field size, meas ured with the
diode placed at the field centre taped on the surface of the phantom.
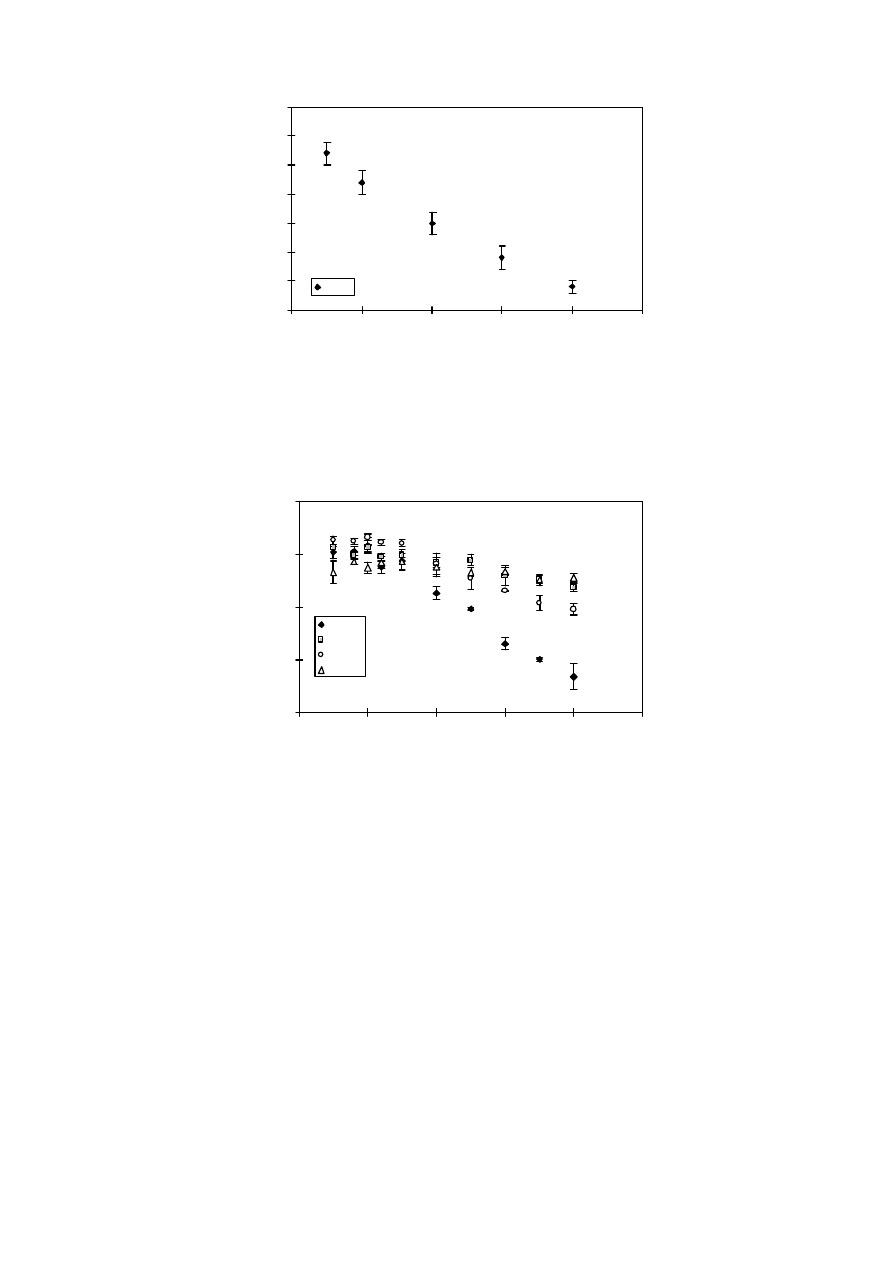
84
Figure 5.5 CF
tray
for EDP-10 diodes and 6 MV X-rays. The mean and SD of CF
tray
determined for 10 EDP-10 diodes are given.
Figure 5.6 CF
tray
for EDP-30, P30, QED and Isorad-p diodes in an 18 MV X-ray beam.
The mean and SD for three diodes of each type and three measurements are
shown.
0.975
0.98
0.985
0.99
0.995
1
1.005
1.01
0
10
20
30
40
50
side of the square field (cm)
CF
tray
EDP10
0.970
0.980
0.990
1.000
1.010
0
10
20
30
40
50
side of square field (cm)
CF
tray
EDP30
P30
QED
isorad-p
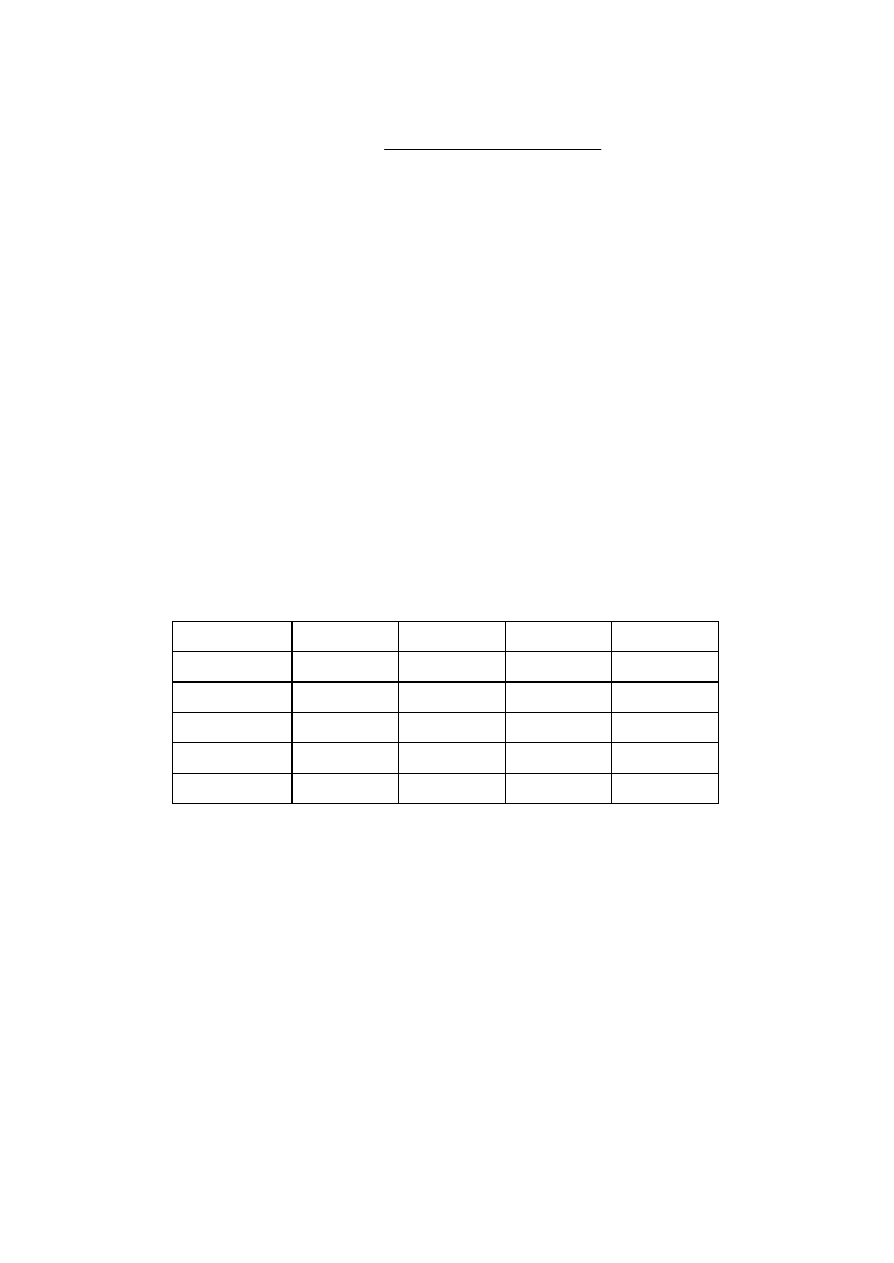
85
diode
2
IC
max
2
wedge
)
cm
10x10
,
w
(
on
transmissi
)
z
,
cm
10x10
,
w
(
on
transmissi
CF
=
(9)
with w the wedge angle.
For 6 MV X-rays CF
wedge
was determined for 10 EDP-10 diodes, three times each and for
different field sizes. The estimated uncertainties associated with the determination of this
factor are up to 1% for the different wedges. These uncertainties correspond to 1 SD of 5
measurements performed with the same diode on different days. For the EDP-10 diodes and
6 MV X-ray beams the dependence on field size of CF
wedge
is of the same order as the
uncertainty in the factor itself. Therefore, CF
wedge
is considered independent of field size
and CF
wedge
determined for a field size of 10x10 cm
2
is used.
In Table 5.2, the correction factors for the EDP-10, EDP-30, P30, QED and Isorad-p diodes
are shown for the different wedges. For the EDP-30, P30 and Isorad-p diodes, the mean of 5
measurements for three different diodes of the same type is given. In the case of the QED
diode, the correction factor is determined once for one diode.
Wedge angle (º)
15
30
45
60
CF
wedge
EDP-10
1.009
1.013
1.018
1.035
CF
wedge
EDP-30
1.002
1.004
0.998
1.009
CF
wedge
P30
0.994
0.998
0.998
1.041
CF
wedge
QED
1.005
0.999
1.012
1.015
CF
wedge
Isorad-p
0.993
0.989
0.978
1.010
Table 5.2 CF
wedge
for different wedges for a 10 x 10 cm
2
field and for 6 MV X-rays (EDP-
10) or 18 MV x-rays (EDP-30, P30, QED and Isorad-p).
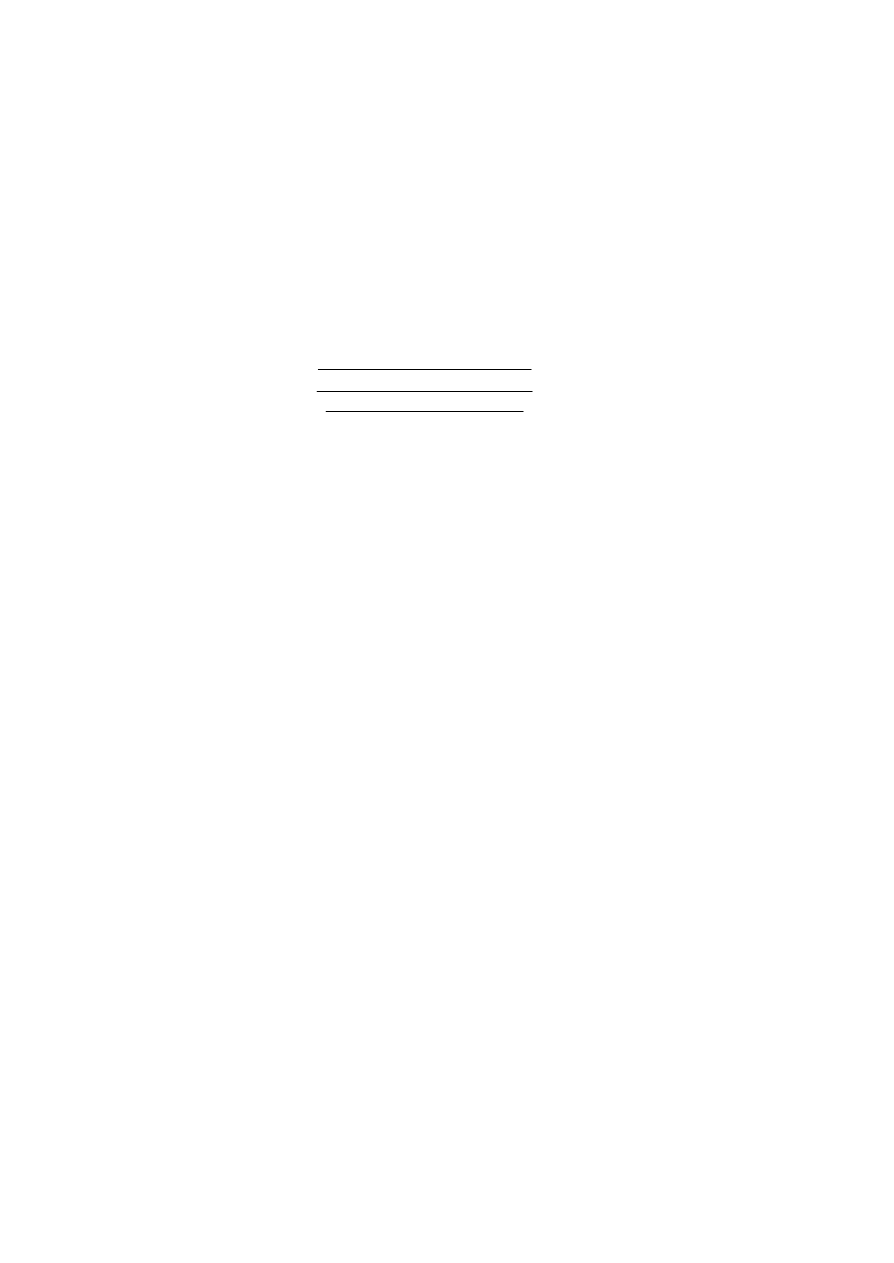
86
5.1.2.4 SSD CORRECTION FACTOR (CF
SSD
)
When the SSD is changed, the dose per pulse and the electronic contamination change.
First, the sensitivity of the diodes depends on dose per pulse. Secondly, if the build -up cap
of the diode is not thick enough an overestimation of dose at short SSD can be due to
electronic contamination that would be “seen” by the diode but not by the ionisation
chamber placed at the depth of dose maximum. Therefore, a SSD correction factor different
from 1 is expected.
The correction factor for SSD is defined as:
cm)
100
SSD
,
cm
10x10
(
SSD)
,
cm
10x10
(
cm)
100
SSD
,
cm
10x10
,
(
SSD)
,
cm
10x10
,
(
2
2
2
max
2
max
=
=
=
diodes
diodes
ic
ic
SSD
R
R
z
R
z
R
CF
(10)
The diode is taped on the surface of a Plastic Water
TM
phantom. The field size is fixed to 10
x 10 cm
2
at the isocentre. The reading of the diode measurement at different SSD normalised
to the reading of the diode measurement 100 cm SSD is compared to the same ratio
measured with an ionisation chamber placed inside a Plastic Water
TM
phantom at the depth
of dose maximum.
In Figure 5.7
CF
SSD
for different types of diodes and for an 18 MV X-ray beam is shown.
87
Figure 5.7 CF
SSD
for EDP-30, P30, QED and Isorad-p diodes for an 18 MV X-ray beam.
The mean and standard deviation for three diodes of each type and three
measurements are shown.
5.1.2.5 ANGLE CORRECTION FACTOR (CF
angle
)
To measure the directional dependence of the diodes they where placed with the
measuring point (considered to be at the b asis of the diode) at the isocentre on the surface
of the Plastic Water
TM
phantom. The variation of the diode response with gantry angle for
a 10 x 10 cm
2
field was measured with the diode long axis perpendicular (axial symmetry)
and parallel (tilt symmetry) to the gantry rotation (Figure 5.8). The results of the
measurements are shown in Figures 5.9 and 5.10.
Figure 5.8 Design of a P30 diode. The plane containing x is the plane of gantry rotatio n
for tilt symmetry. The plane containing y is the plane of gantry rotation for
axial symmetry.
x
y
0.940
0.960
0.980
1.000
1.020
1.040
1.060
70
80
90
100
110
120
130
SSD (cm)
CF
SSD
EDP30
P30
QED
Isorad-p
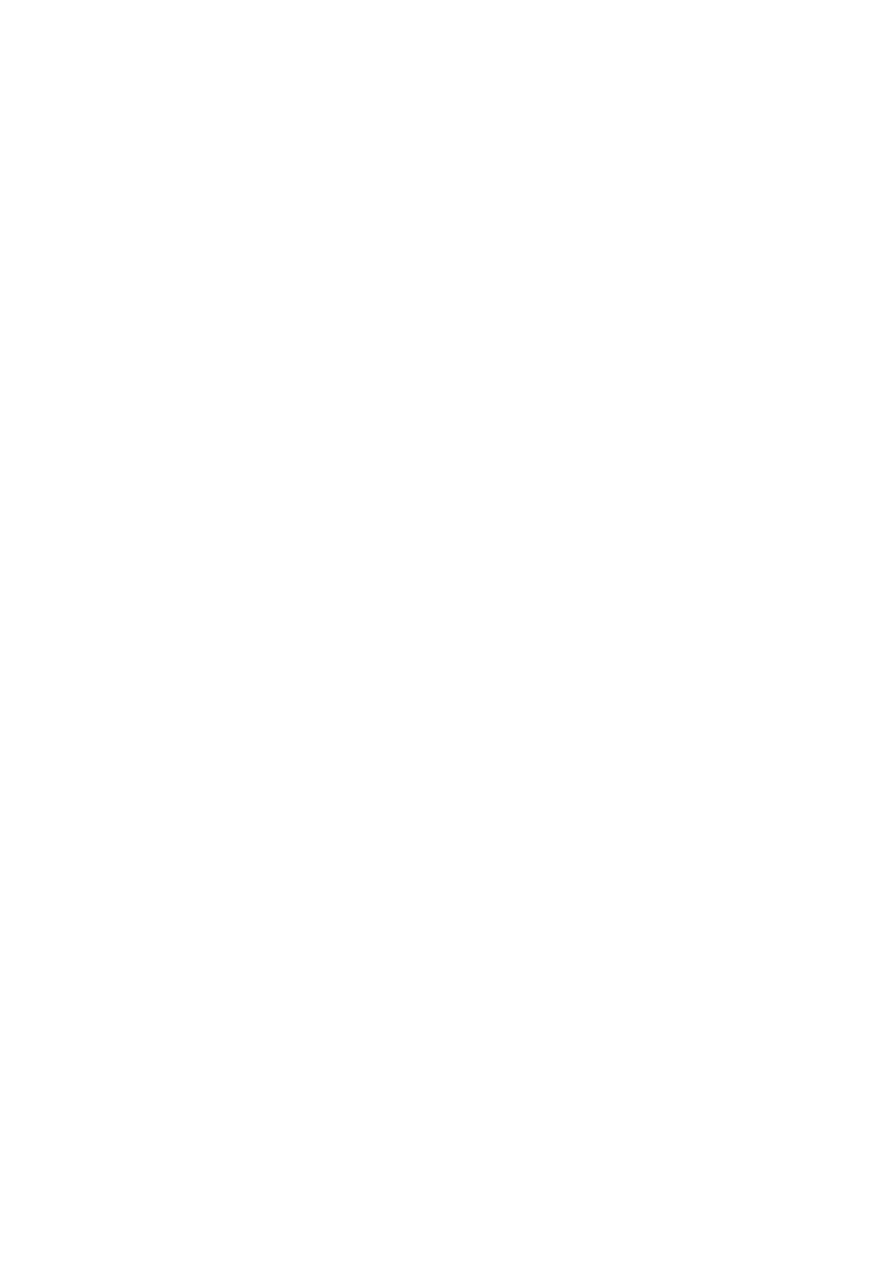
88
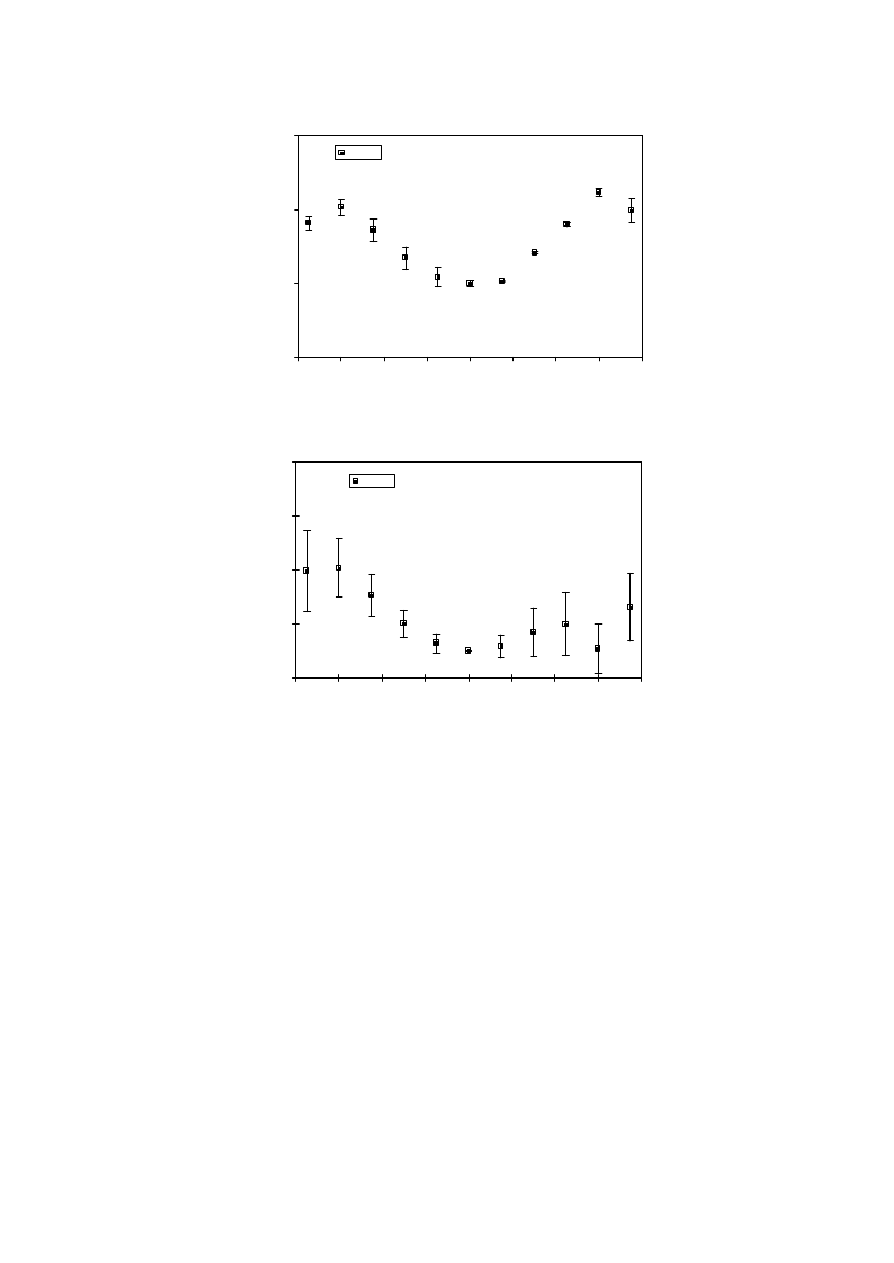
89
Figure 5.9 Axial and tilt symmetry for EDP-10 diodes, for 6 MV X-rays.
0.980
1.000
1.020
1.040
-80
-60
-40
-20
0
20
40
60
80
angle (°)
CF
axial angle
EDP10
0.990
1.010
1.030
1.050
1.070
-80
-60
-40
-20
0
20
40
60
80
angle (°)
CF
tilt angle
EDP10
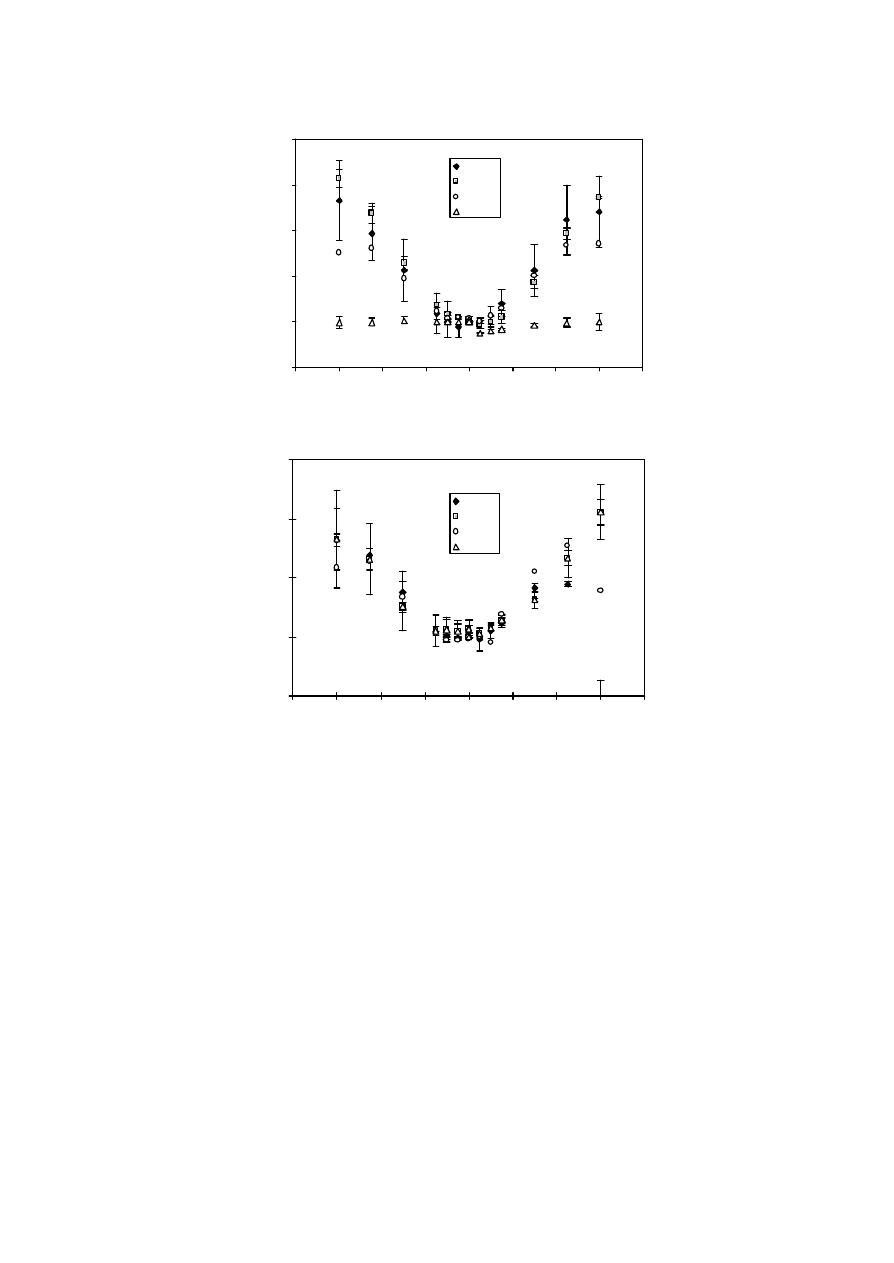
90
Figure 5.10 Axial and tilt symmetry for EDP-30, P30, QED and Isorad-p diodes for 18 MV
X-rays.
0.980
1.000
1.020
1.040
1.060
1.080
-80
-60
-40
-20
0
20
40
60
80
angle (°)
CF
axial angle
EDP30
P30
QED
Isorad-p
0.980
1.000
1.020
1.040
1.060
-80
-60
-40
-20
0
20
40
60
80
angle (°)
CF
tilt angle
EDP30
P30
QED
Isorad-p

91
5.1.2.6 TEMPERATURE CORRECTION FACTOR (CF
temperature
)
To study the influence of temperature on the diode signal a water phantom equipped with a
thermostat is used. The diodes are taped on a thin slab of Perspex, which is in contact with
the water. The temperature, measured with a digital thermistor provided with an immersion
probe, is slowly increased from 22.5 ºC to 32 ºC. The sensitivity of the diodes is determined
at different temperatures and expressed relative to that at 22.5 ºC. Each temperature is
maintained approximately 20 minutes in order to reach full thermal equilibrium between the
surface of the phantom and the diodes. The procedure is performed twice, when the diodes
are received and after some time of use (1kGy of accumulated dose).
The temperature correction factor is defined as:
(
)
)
5
.
22
)
(
.
(
1
C
C
T
SVWT
CF
e
temperatur
°
−
°
−
=
(11)
if the temperature at which the diodes have been calibrated (T
cal
) is 22.5°C.
SVWT is the sensitivity variation with temperature.
If T
cal
differs from 22.5ºC, the temperature correction factor is defined as:
(
)
( )
(
)
)
5
.
22
.
(
1
)
5
.
22
)
(
.
(
1
C
T
C
SVWT
C
C
T
SVWT
CF
cal
e
temperatur
°
−
°
−
°
−
°
−
=
(12)
For 10 EDP-10 diodes the variation of sensitivity (in percentage) per ºC varies from 0.26 to
0.34. Table 5.3 shows the sensitivity variation per ºC for different EDP-30 diodes, new and
after some time of clinical use. In Figure 5.11 the variation of sensitivity of EDP-30, P30,
QED and Isorad-p diodes is shown.
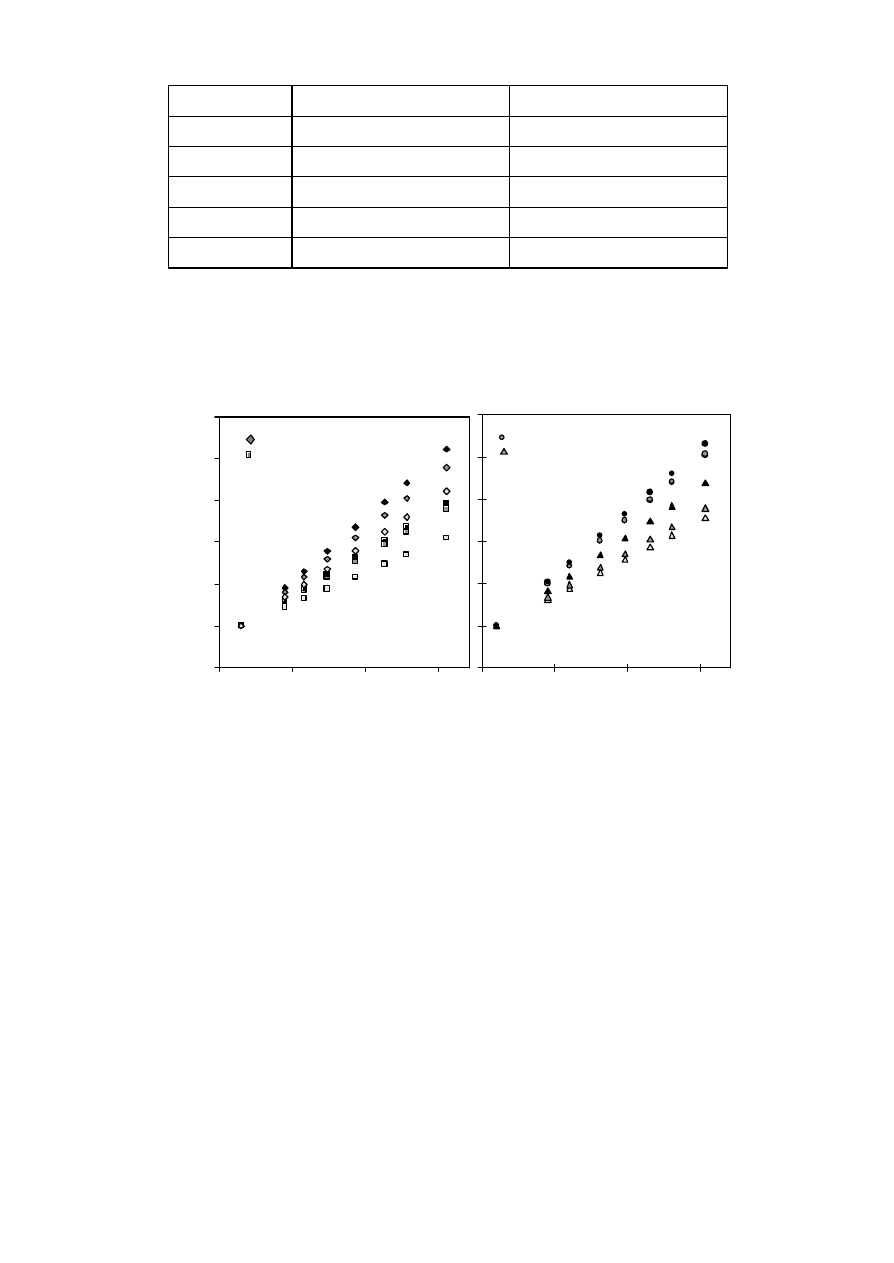
92
Diode number
new variation(%/ºC)
post-irradiation variation (%/ºC)
1
0. 290
0. 275
2
0. 293
0. 291
3
0. 320
0. 340
4
0. 216
0. 274
5
0. 281
0. 273
Table 5.3 Variation of sensitivity (SVWT) in % per ºC for EDP-30 diodes, when the diodes
are new and after some time of use.
Figure 5.11 Variation of sensitivity with temperature of (a) three EDP-30 and three P30
diodes, and (b) three QED and three isora d-p diodes. 21.5ºC was chosen as
normalisation temperature.
0.99
1
1.01
1.02
1.03
1.04
1.05
20
25
30
35
temperature t (ºC)
signal at tºC/signal at 21.5ºC
EDP30
P30
20
25
30
35
temperature t (ºC)
QED
isorad-p
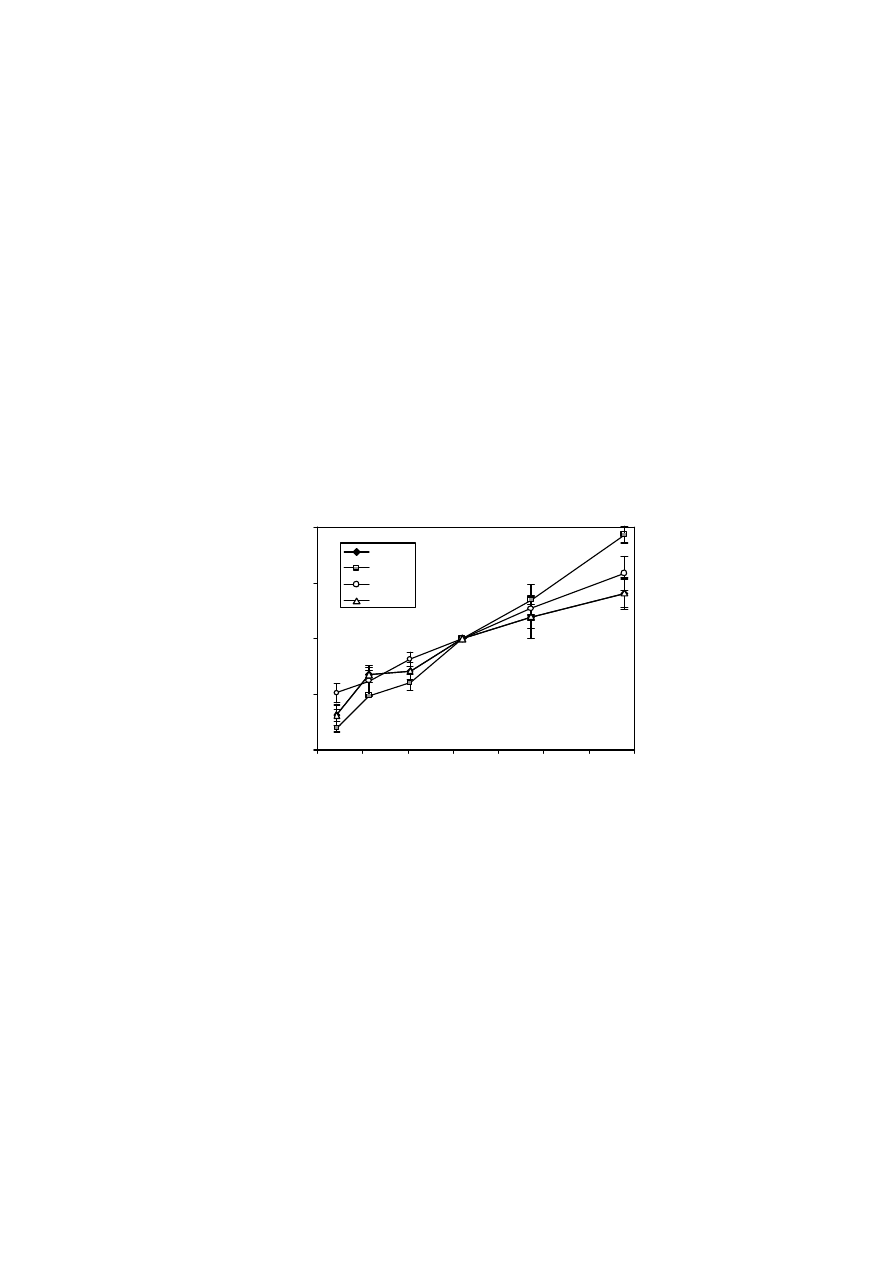
93
5.1.2.7 INFLUENCE OF THE DOSE RATE ON THE DIODE’S SENSITIVITY
A Clinac 1800 (Varian) accelerator changes the dose rate by varying the number of pulses
per unit of time and not the dose per pulse. Therefo re, to test the intrinisic influence of
dose per pulse on the diode sensitivity, the following experiment was designed. In order to
exclude electron contamination, the diodes are inserted in a Plastic Water
TM
phantom at 10
cm depth. Their flat surface is facing the beam. In this way, the measurements are not
affected by differences in build -up caps. The source-surface distance is then varied from 80
cm (0.56 mGy/pulse) to 130 cm (0.23 mGy/pulse). The field size is chosen constant and in
such a way that the phantom is completely irradiated at any distance. The test has been
performed for EDP-30, P30, QED and Isorad-p diodes. Results are shown in Figure 5.12.
In this experiment, no wedges are used to reduce the dose rate as by doing so, not only
dose rate would be modified but also the energy spectrum. The results of such an
experiment would mix up dose rate dependence with energy dependence.
Figure 5.12 Influence of dose rate on diode signal. Relative sensitivity is defined as the
ratio of the response of the diode at any dose per pulse to the response at the
dose per pulse corresponding to a SSD of 100 cm.
0.980
0.990
1.000
1.010
1.020
0.200
0.250
0.300
0.350
0.400
0.450
0.500
0.550
dose rate (mGy/pulse)
relative diode signal
EDP30
P30
QED
Isorad-p
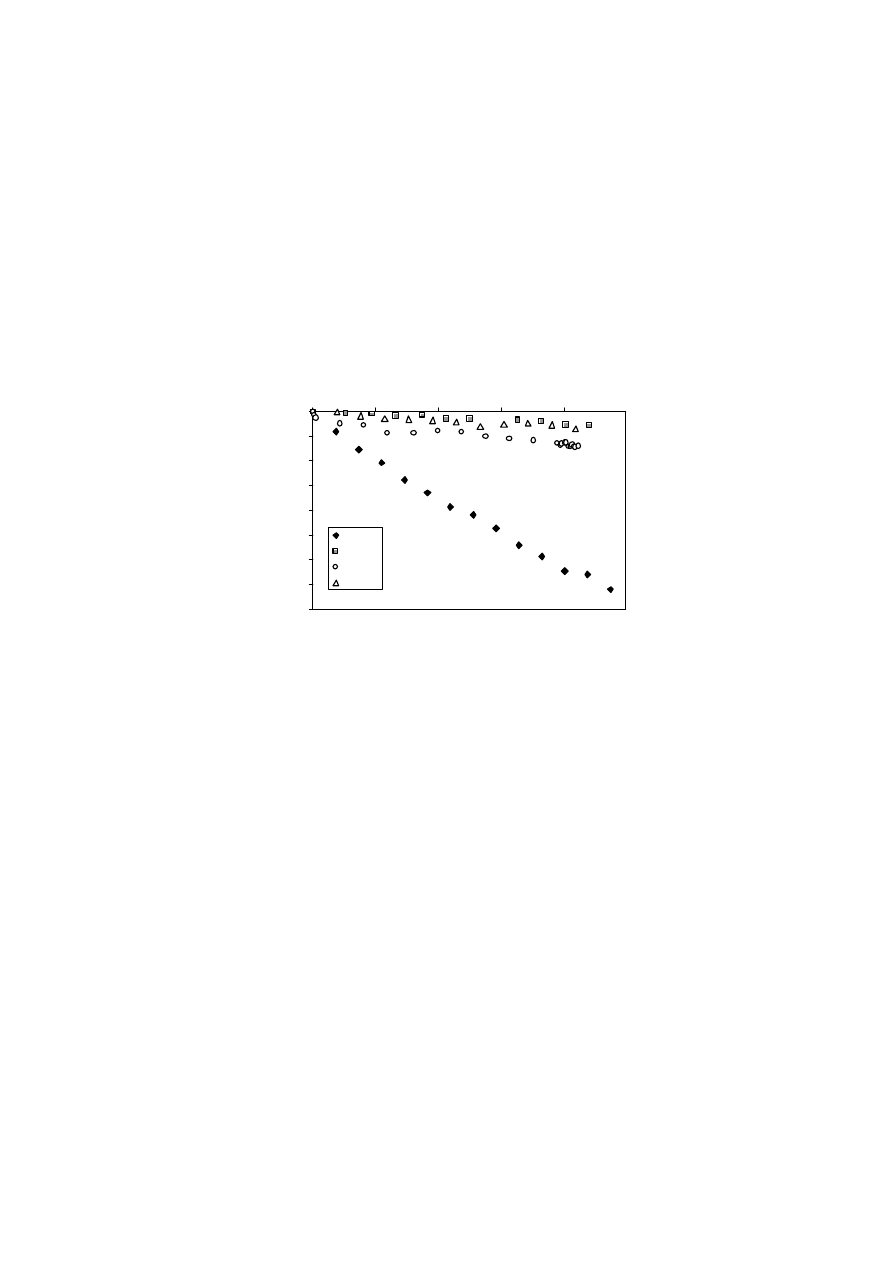
94
5.1.2.8 SENSITIVITY VARIATION WITH ACCUMULATED DOSE (SVWAD)
The loss of sensitivity with accumulated dose has been studied for EDP-30, P30, QED and
Isorad-p diodes. Readings for 177 MU have been obtained after irradiations of 1500 MU (17
Gy) at 240 MU/min (dose rate used in clinical practice) in an 18 MV X-ray beam. A
monitoring ionisation chamber is used to avoid accelerator fluctuations influencing the
results of the study.
Figure 5.13 shows the loss of sensitivity with accumulated dose for the different diodes.
For
the EDP diodes the SVWAD can vary substantially. Much smaller values have been
reported [Meijer 2001], which are more in agreement with the specifications in Table 1.1.
Figure 5.13 Sensitivity loss with accumulated dose for EDP-30, P30, QED and Isorad-p
diodes
-8%
-7%
-6%
-5%
-4%
-3%
-2%
-1%
0%
0
50
100
150
200
accumulated dose (Gy)
loss of sensitivity
EDP30
P30
QED
Isorad-p
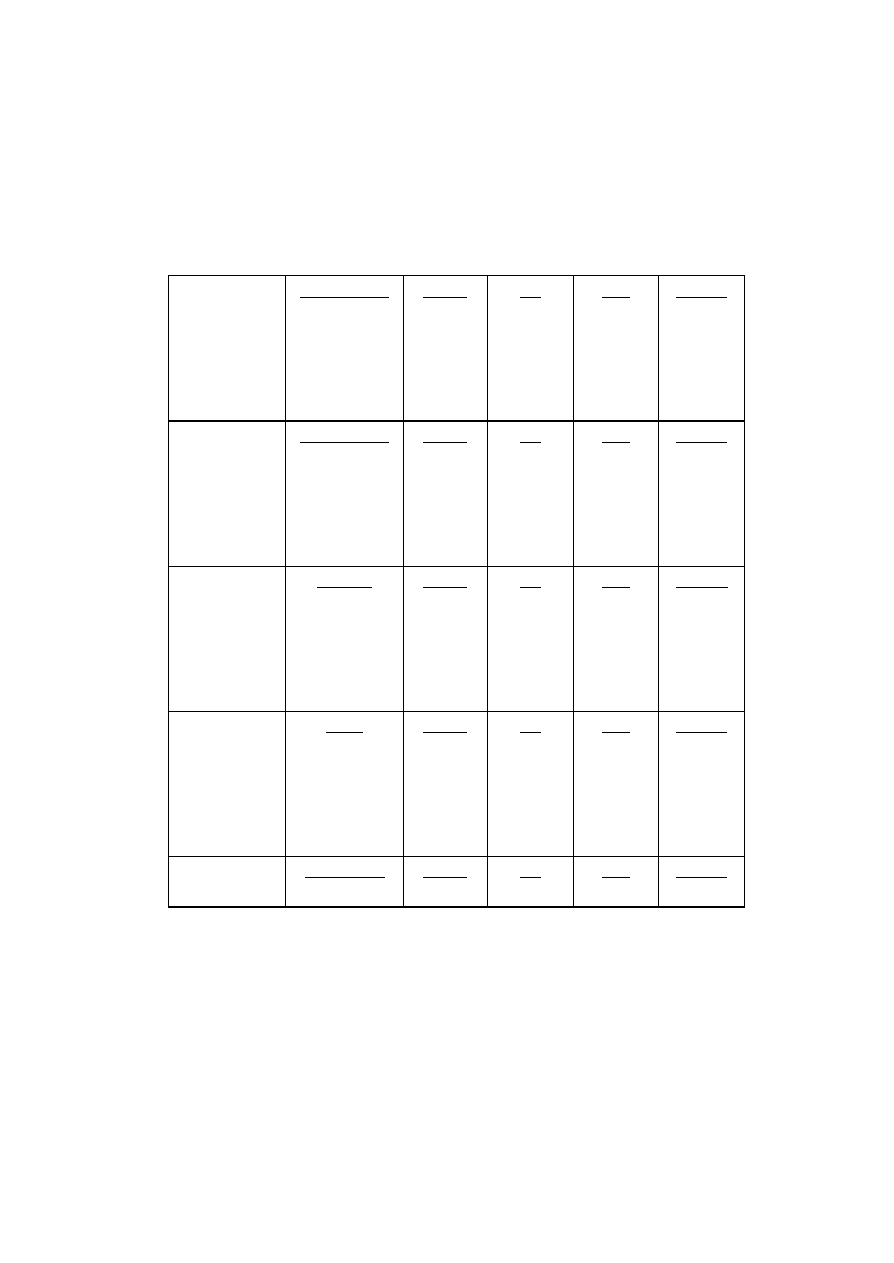
95
Table 5.4 Summary of entrance correction factors for EDP-30, P30, QED and Isorad-p
diodes, for 18 MV X-rays. For EDP-30, P30 and Isorad-p diodes, the mean of
three diodes of each type and three determinations for each diode is given. For
QED diodes the mean of one measurement and three diodes is given, with the
exception of CF
wedge
and CF
angle.,
for which the results of one diode and one
measurement are given.
CF
FS
SSD = 100 cm
Open field
Field size (cm
2
)
5 x 5
10 x 10
15 x 15
20 x 20
30 x 30
EDP-30
0.978
1.000
0.993
0.984
0.968
P30
0.970
1.000
1.016
1.026
1.034
QED
0.986
1.000
1.006
1.008
1.011
Isorad-p
0.968
1.000
1.018
1.031
1.044
CF
tray
SSD = 100 cm
Field size (cm
2
)
5 x 5
10 x 10
15 x 15
20 x 20
30 x 30
EDP-30
1.000
1.002
0.999
0.993
0.983
P30
1.001
1.001
1.000
0.998
0.996
QED
1.003
1.003
1.002
0.998
0.993
Isorad-p
0.997
0.997
0.999
0.998
0.997
CF
SSD
Field size
= 10 x 10 cm²
Open field
SSD (cm)
80
90
100
110
120
EDP-30
0.973
0.992
1.000
1.010
1.021
P30
0.965
0.985
1.000
1.014
1.031
QED
0.964
0.987
1.000
1.012
1.025
Isorad-p
0.969
0.992
1.000
1.019
1.035
CF
angle
(Axial symmetry)
SSD = 100 cm
Field size
= 10 x 10 cm
2
Open field
Angle
0º
10º
30º
45º
60º
EDP-30
1.000
1.002
1.022
1.042
1.050
P30
1.000
1.002
1.022
1.044
1.058
QED
1.000
1.002
1.020
1.033
1.033
Isorad-p
1.000
1.000
1.000
1.000
1.000
CF
wedge
Wedge angle
15º
EDP-30
1.002
P30
0.994
QED
1.005
Isorad-p
0.993
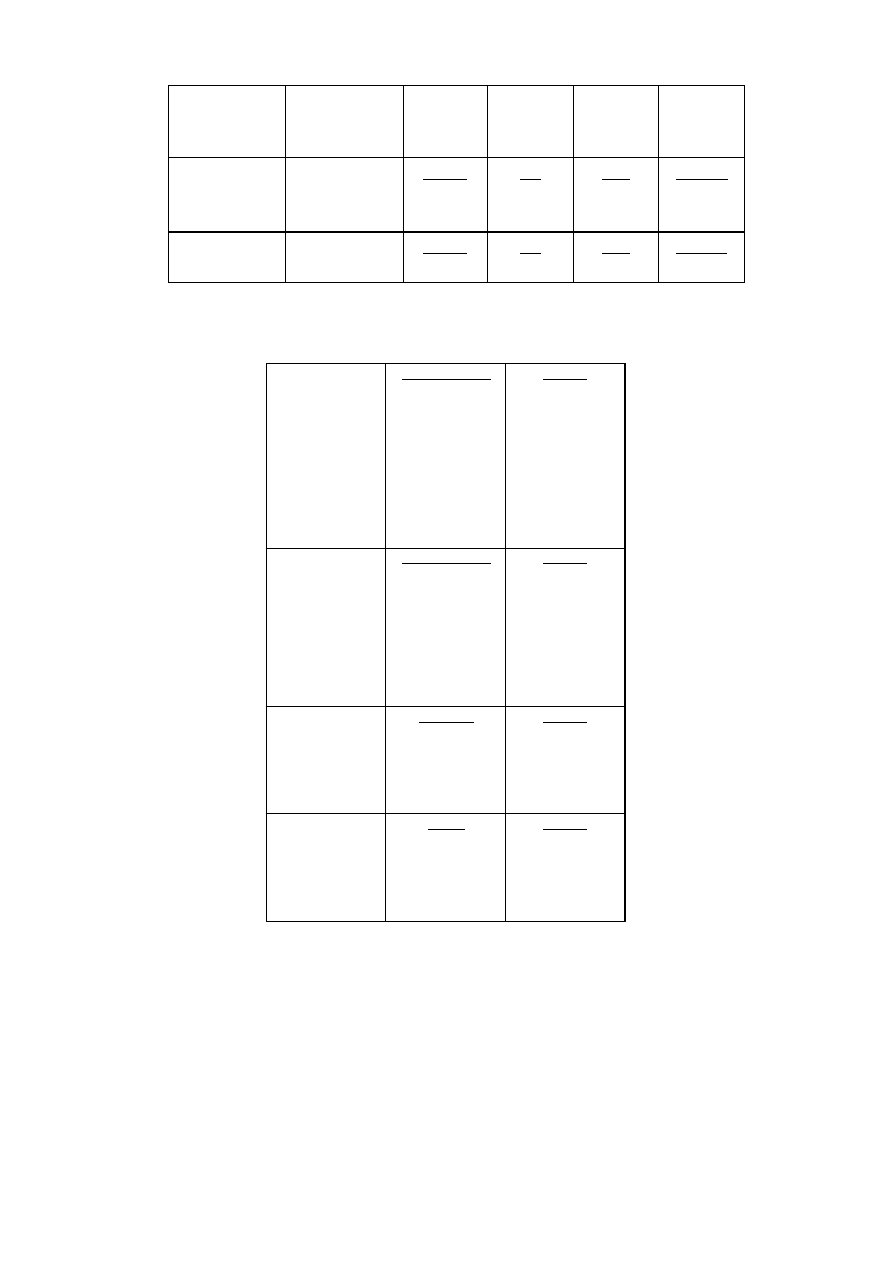
96
SSD =100cm
Field size
= 10 x 10 cm
2
30º
45º
60º
1.004
0.998
1.009
0.998
0.998
1.041
0.999
1.012
1.015
0.989
0.978
1.010
SVWT
EDP-30
0.23-0.30
%/ºC
P30
0.15-0.21
%/ºC
QED
0.29-0.30
%/°C
Isorad-p
0.19-0.25
%/ºC
SVWAD
EDP-30
3.4%/100Gy
P30
0.2%/100Gy
QED
0.8%/100Gy
Isorad-p
0.3%/100Gy
Table 5.5 Summary of entrance correction factors for EDP-10 diodes for 6 MV X-rays. The
mean of ten diodes is given.
CF
FS
SSD = 100 cm
Open field
Field size (cm
2
)
5 x 5
10 x 10
15 x 15
20 x 20
30 x 30
40 x 40
EDP-10
1.000
1.000
0.996
0.992
0.987
0.985
CF
tray
SSD = 100 cm
Field size (cm
2
)
5 x 5
10 x 10
15 x 15
20 x 20
30 x 30
EDP-10
1.002
1.000
0.996
0.992
0.987
CF
SSD
Field size 10 x 10
Open field
SSD (cm)
80
90
100
EDP-10
0.982
0.991
1.000
CF
angle
(Axial symmetry)
SSD = 100 cm
Field size 10 x 10
Angle
0º
10º
30º
EDP-10
1.000
1.002
1.008
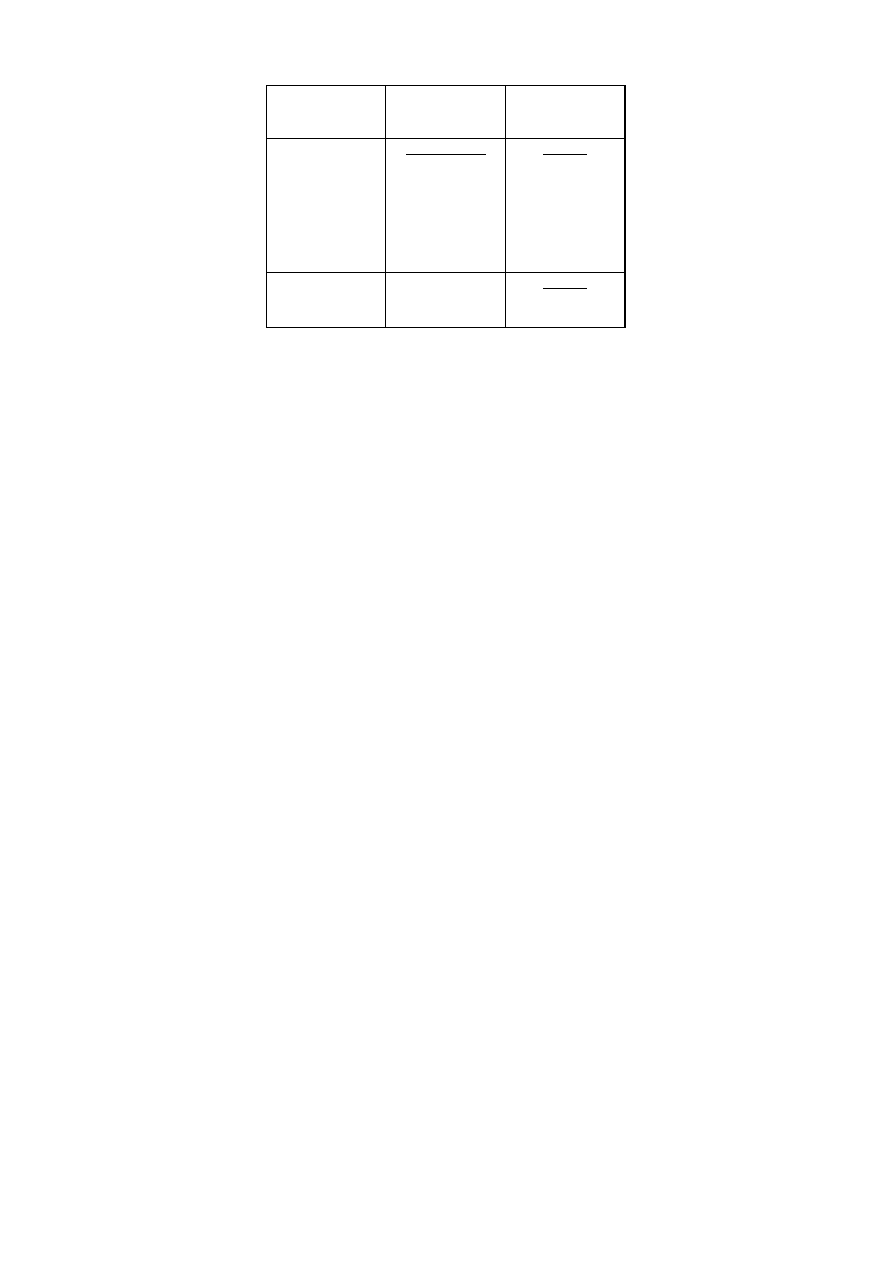
97
Open field
45º
60º
1.015
1.023
CF
wedge
SSD =100cm
Field size 10 x 10
Wedge angle
15º
30º
45º
60º
EDP-10
1.009
1.013
1.018
1.035
SVWT
EDP-10
0.26-0.34%/ºC

98
5.2 PERFORMANCE OF SOME COMMERCIAL DIODES IN HIGH ENERGY
PHOTON BEAMS – THE LEUVEN EXPERIENCE
5.2.1 INTRODUCTION
For entrance dose measurements, in vivo diodes are covered with a build -up cap to enable
measurements at a certain depth. Firstly, in any case (unless for surface dose
measurements) some build -up is necessary in order to avoid the initial steep dose gradient.
Secondly, the build -up region is influenced by the variation in the amount of electron
contamination with different treatment geometries i.e. different source-surface-distance or
field size, or the presence of beam modifiers [Biggs 1979]. Depending on the cap thickness,
the diode will reflect this variation to a certain degree, in particular in high-energy photon
beams, where the influence of the contaminating electrons in the build -up region is larger,
mainly due to their increased range [Sjögren 1996]. Therefore, the build -up cap of the diode
should ideally have the same thickness as the build -up layer covering the ionization
chamber during the calibration, i.e. the build -up cap thickness should be equal to the depth
of dose maximum of the photon beam quality in use.
On the other hand, thicker build -up caps cause a larger perturbation of the treatment field
(which is however of only limited relevance if the diode is applied during only one or two
seesions). Commercially available diodes have different build -up cap thicknesses; some of
them are designed with a thinner cap to minimise field disturbance . With regard to the
diode correction factors to be used in non-reference conditions, this has important
consequences that may jeopardise the accuracy of in vivo dosimetry at high energies: i)
The magnitude of the correction factors will be larger. ii) In a clinical situation where it is
preferable to limit the number of factors, the factors have been established independently
and are used together for various combinations of beam setting. This may no longer be
straightforward if the degree of electron contamination, which will be depend on the
specific combination of accessories and beam set-up parameters, has a considerable
influence on the diode signal.

99
This problem is addressed in some recent studies performed in Leuven [Georg 1999],
Barcelona [Jornet 2000], Copenhagen [Lööf 2001], and Amsterdam [Meijer 2001]. Only
limited information is available describing the correction factor variation and/or the
achievable accuracy for in vivo dosimetry methods in the ‘high’ energy range (16 – 25
MV). Therefore, the first aim of these studies was to assess and analyse the variation of
diode correction factors for entrance dose measurements at higher photon beam energies.
For the investigations performed in Barcelona and Copenhagen commercially available n -
type as well as p-type diodes have been included. The dosimetric characteristics of n -type
diodes have been published in [Jornet 2000]. The results of the comparative study of EDP-
30, QED (p-type diodes) and P30 (n -type diode) in Barcelona are shown Section 5.1, and are
substantiated by the results obtained in Copenhagen [Lööf 2001] and Amsterda m [Meijer
2001].
Results of the study performed in Leuven ([Georg 1999]) will be presented in this
contribution. In addition to determining the correction factors for commercial diodes, the
total build-up thickness of the diodes is modified in order to min imise the correction factor
variation.
5.2.2 MATERIAL AND METHODS
5.2.2.1 MATERIAL
The Scanditronix p-type diodes that are recommended for in vivo dosimetry in high energy
photon beams have been investigated: two different EDP-20 diodes - “old” and “new” type
- and EDP-30 diodes. The specifications of these diodes are listed in Section 1.1.4, Table
1.3. The main difference between old and new EDP-20 diodes is the higher doping level of
the new type, which was introduced in order to improve the dose rate properties with
accumulated dose. The EDP-30 also has a high doping level
.
Furthermore the new EDP-20
type is covered with a thin (0.2 - 0.3 mm) plastic layer. The old type EDP-20 diode, which is
no longer produced, is included in this study since it is still in clinical use.

100
For all measurements diodes are connected to commercially available or home made
electrometers with a low input impedance [Rikner 1987]. Additional build -up caps have
been manufactured in the hospital’s mechanical work-shop. These build -up caps have
(nominally) thickness equivalent in attenuation to 10, 15, 20 and 30 mm water, and are made
from either copper, lead, or iron. The build -up caps can easily be added to and removed
from the diode without any damage. Whenever modified with an additional build -up cap,
the diode is described by adding as an index the total build -up thickness of the (modified)
diode, and the build -up cap material is indicated by its chemical symbol, e.g. measurements
made with an EDP-20/30(Cu) diode indicate that the EDP-20 diode has been modified by a
copper build -up cap equivalent in thickness to 10 mm water. For EDP-30, the thickness of
the commercial (Tantalum) build -up cap corresponds to approximately 14 mm water
equivalent material [Jornet 1996 and Section 5.1.1.4]. Although this value is apperently not
fixed, but depends on the head-scatter spectrum of the accelerator [Meijer 2001, Sjögren
1998], we have assumed it to be around 15 mm. Therefore, e.g. EDP-30/30(Cu) means that
an additional copper build -up cap equivalent in thickness to 15 mm water has been added.
Ionisation chamber measurements are performed using a cylindrical ionisation chamber (NE
2571, volume 0.6 cm
3
). All diode correction factors are determined in a large polystyrene
phantom consisting of plates of different thicknesses.
The diode characteristics are investigated in 18 MV, 23 MV and 25 MV photon beams,
provided by different linear accelerators: a Philips SL20 (18 MV, QI = 0.78), a GE Saturne
43/Series 800 (18 MV, QI = 0.77, 25 MV, QI = 0.786), two GE Saturne 42/Series 700 (18 MV,
QI = 0.77 and 0.78), and a GE Sat II+ (23 MV, QI = 0.79). The GE Sat 43/800 is equipped with
an integrated multileaf collimator wh ile all other machines have conventional collimators.
The main difference between the Philips and the GE accelerators is the treatment head
geometry, especially the collimator design and the flattening filter material and position.
The influence of a wedge filter on the different diode types has been investigated in the
beams of the Saturne 43 linac. The internal tungsten alloy wedge (nominal wedge angle

101
60°) is located between the monitor chamber and the upper pair of jaws. The maximum
wedged field size in the wedge direction is limited to 20 cm.
The influence of a 0.8 cm PMMA block tray is determined for the photon beams of the
same accelerator with a source-to-tray distance of about 62 cm. Block correction factors are
measured for beams of the Philips SL 20, the GE Sat 42 and GE Sat II+ accelerators with
source-to-tray distances between 67 and 68 cm.
Perturbation effects are determined using film dosimetry. Therefore Kodak X-Omat films are
irradiated at the depth of maximum dose, at 5 cm and 10 cm depth in a polystyrene
phantom. All films are evaluated with a Vidar Scanner and film dosimetry software
(Poseidon, Precitron, Sweden) running on a PC. Optical densities are converted into
relative dose values using calibration curves.

102
5.2.2.2 METHODS
The entrance dose is measured with the diodes using the methodology described in
Section 1.2 and Section 5.1. Field size correction factors are assumed to be independent of
SSD and SSD correction factors are assumed t o be independent of field size:
C(FS, SSD)
≈ C
FS
(FS, 100 cm) • C
SSD
(10 x 10 cm
2
, SSD).
(13)
In order to verify equation (13) at higher photon energy, where electron contamination can
have a significant influence, several measurements are performed at 80 and 120 cm SSD for
large and small field sizes (5 x 5 cm
2
and 30 x 30 cm
2
), at 18 and 25 MV. If this assumption
would not be valid in the energy range under consideration, a two -dimensional correction
factor table should have to be determined, requiring tedious measurements.
Assuming the validity of equation (13), field size correction factors C
FS
are measured for
square fields ranging from 5 x 5 cm
2
to the maximum field size of 40 x 40 cm
2
at reference SSD
(100 cm). Source-surface-distance correction factors C
SSD
are measured for SSDs varying
from 80 to 120 cm for the reference field size (10 x 10 cm
2
).
Wedge correction factors C
wedge
are measured at reference SSD for square fields of 5 cm, 10
cm and 20 cm field size. Since the wedge position is critical, measurements with wedge are
performed for collimator orientations of 90
°
and 270
°
, and C
wedge
is determined as the
average value. A tray correction factor C
tray
is determined repeating all C
FS
and C
SSD
measurements for a block tray. Block correction factors C
block
are measured for a fixed
collimator opening of 20 x 20 cm
2
for blocks defining square fields of 5 cm, 8 cm, 10 cm, 14.1
cm, and 17.3 cm side length (at the isocenter plane). The block-to-isocentre distance varies
between 32 and 38 cm for different linacs.
The variation of correction factors for diodes from the same batch is estimated from C
FS
and C
SSD
measurements for three EDP-30 and two new type EDP-20 diodes.
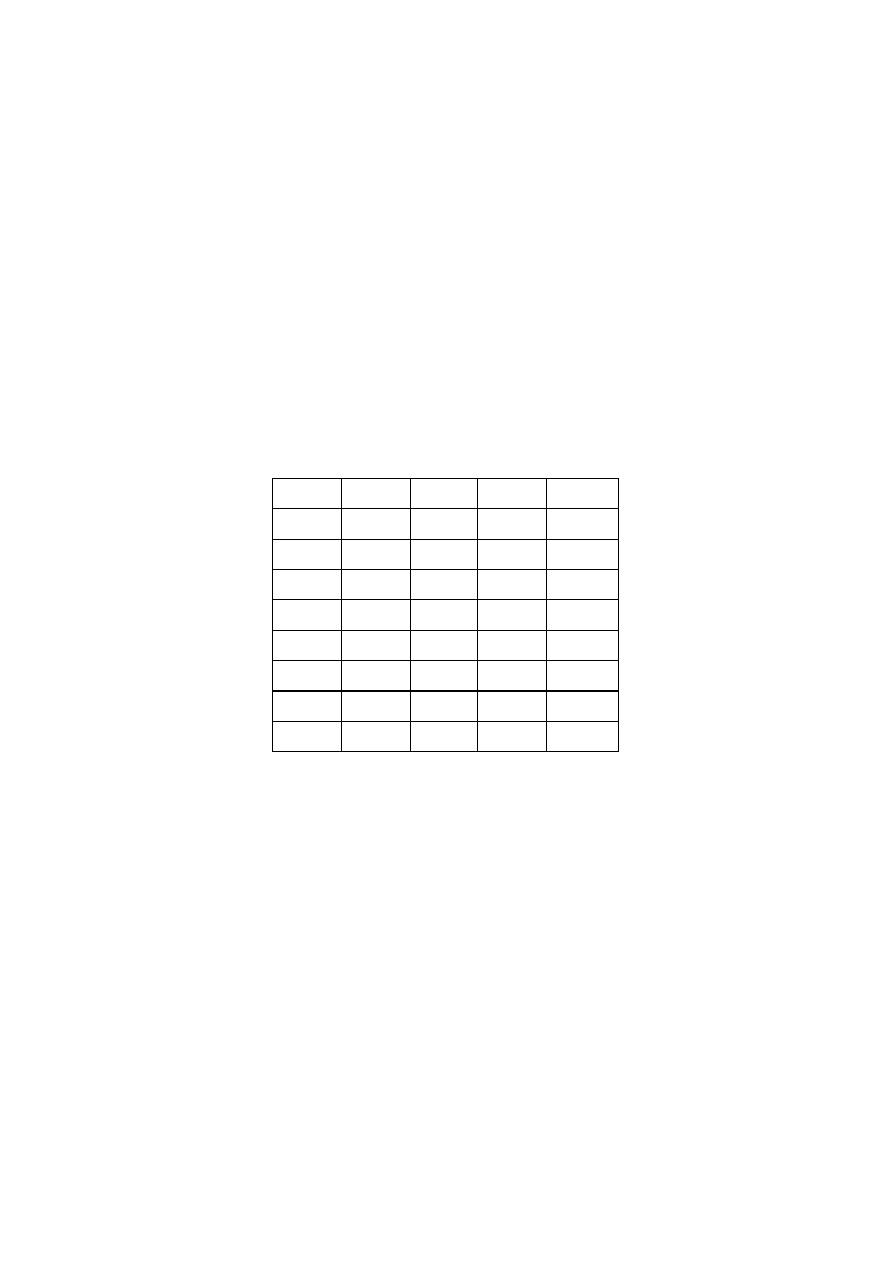
103
5.2.3 RESULTS
5.2.3.1 INDEPENDENCE OF FIELD SIZE AND SSD CORRECTION FACTORS
Equation (13) has been checked for old and new type EDP-20 and EDP-30 diodes in 18 MV
and 25 MV photon beams provided by GE linacs (SAT 42 and 43). The agreement between
the measured correction factor C(FS,SSD) and the correction factor calculated from C
FS
and
C
SSD
is between 1 - 1.5 % for modified and unmodified old type and new type EDP-20
diodes. The larger deviations around 1.5 % are observed for a 5 x 5 cm
2
field size either at 80
or at 120 cm SSD. For the modified EDP-30/30(Cu) diodes deviations do not exceed 1.5 %,
while for unmodified EDP-30 diodes maximum deviations around 2 % are observed for a 5 x
5 cm
2
field at 80 cm SSD. Total build -up thickness larger than 30 mm (e.g. old type EDP-
20/40(Cu) or EDP-30/35(Cu)) did not improve these results.
Centre
Charleroi
Leuven
Leuven
St. Jean
Unit
Ph SL 20 GE Sat 43 GE Sat 42 GE Sat 42
FS [cm]
QI=0.78 QI=0.77
QI=0.77
QI=0.78
5 / 6
1.003
1.006
1.006
1.013
10
1.000
1.000
1.000
1.000
15
0.994
0.989
0.990
0.981
20
0.986
0.981
0.979
0.970
25
0.987
0.973
0.972
0.963
30
0.986
0.962
0.960
0.955
Table 5.6 Field size correction factor variation for unmodified old type EDP-20 diodes at
18 MV photon beams measured in different Belgian radiotherapy centers.

104
5.2.3.2 FIELD SIZE CORRECTION FACTOR C
FS
WITHOUT TRAY
Field size correction factors for unmodified old type EDP-20 diodes are shown in Table 5.6
as a function of square field size for 18 MV photon beams provided by different linacs. For
field sizes between 5 x 5 cm
2
and 30 x 30 cm
2
C
FS
varies by only 1.7 % on the Philips SL 20
linac, and around 5 % on GE linacs.
Old type EDP-20 diodes without additional build -up show the largest field size correction
factor variation. In a field size range between 5 x 5 cm
2
and 40 x 40 cm
2
C
FS
varies by about
4-6 % in 18 MV and 25 MV photon beams provided by the GE Sat 43 and 42 accelerators.
When adding build -up caps, the variation could be substantially reduced. For example, for
modified old type EDP-20/30(Cu), for the same field size range and energies, C
FS
varies
only between 1 - 1.5 %.
New EDP-20 diodes without additional build -up show a much smaller C
FS
variation than
the old ones: 2.2 and 2.5 %, respectively, in 18 MV and 25 MV beams provided by the Sat
43 linac. Only a slightly smaller variation of 2 % could be obtained at 18 MV for the
modified new type EDP-20/30(Cu), but the C
FS
variation of 2.5 % at 25 MV could not be
improved when modifying the build -up thickness for this type of diode. For both types of
EDP-20 diodes the C
FS
variation increased when a total water equivalent build -up
thickness of more than 30 mm is used.
EDP-30 diodes without additional build -up show a larger variation of C
FS
than new type
EDP-20 diodes. When increasing the FS from 5 x 5 to 40 x 40 cm
2
the difference between
maximum and minimum C
FS
values reaches 4 % and 4.4 % at 18 MV from the Sat 42 and 43,
but is only 2.4 % at 25 MV. For the EDP-30/30(Cu) the C
FS
variation decreases to 0.5 % for
the 18 MV beam of the Sat 42 accelerator and to less than 1.5 % for the 18 MV beam of the
Sat 43 accelerator, but it increases slightly at 25 MV. For the EDP-30/35(Cu) and EDP-
30/45(Cu) the C
FS
variation increased as compared to the EDP-30/30, this increase is more
pronounced at 25 MV. Figure 5.14 shows the variation of field size correction factors as a
function of field size, dependent on build -up thickness for the different diodes in a 18 MV
photon beam provided by the GE Sat 43 accelerator.
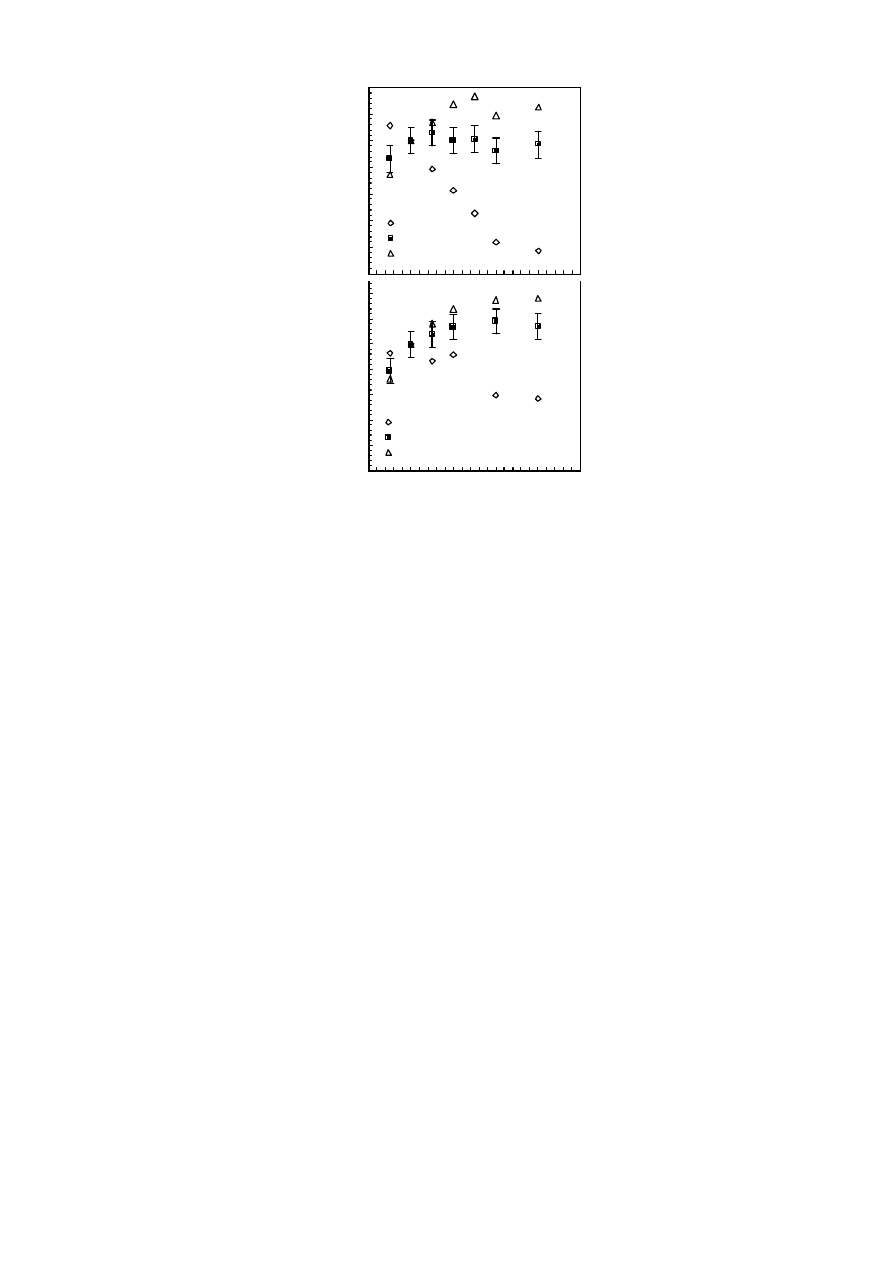
105
Figure 5.14 Variation of the field size correction factor C
FS
for different types of diodes
with and without additional build-up in 18 MV photon beams provided by a
GE Sat 43 linac: (a) old type EDP-20, (b) new type EDP-20, (c) EDP-30. All
results are obtained with copper build-up caps. The error bars indicate the
accuracy of
± 0.5 % in the determination of diode correction factors.
0.95
0.96
0.97
0.98
0.99
1.00
1.01
1.02
C
FS
NEW EDP-20
NEW EDP-20/30
NEW EDP-20/40
(b)
0.95
0.96
0.97
0.98
0.99
1.00
1.01
1.02
C
FS
OLD EDP-20
OLD EDP-20/30
OLD EDP-20/40
(a)
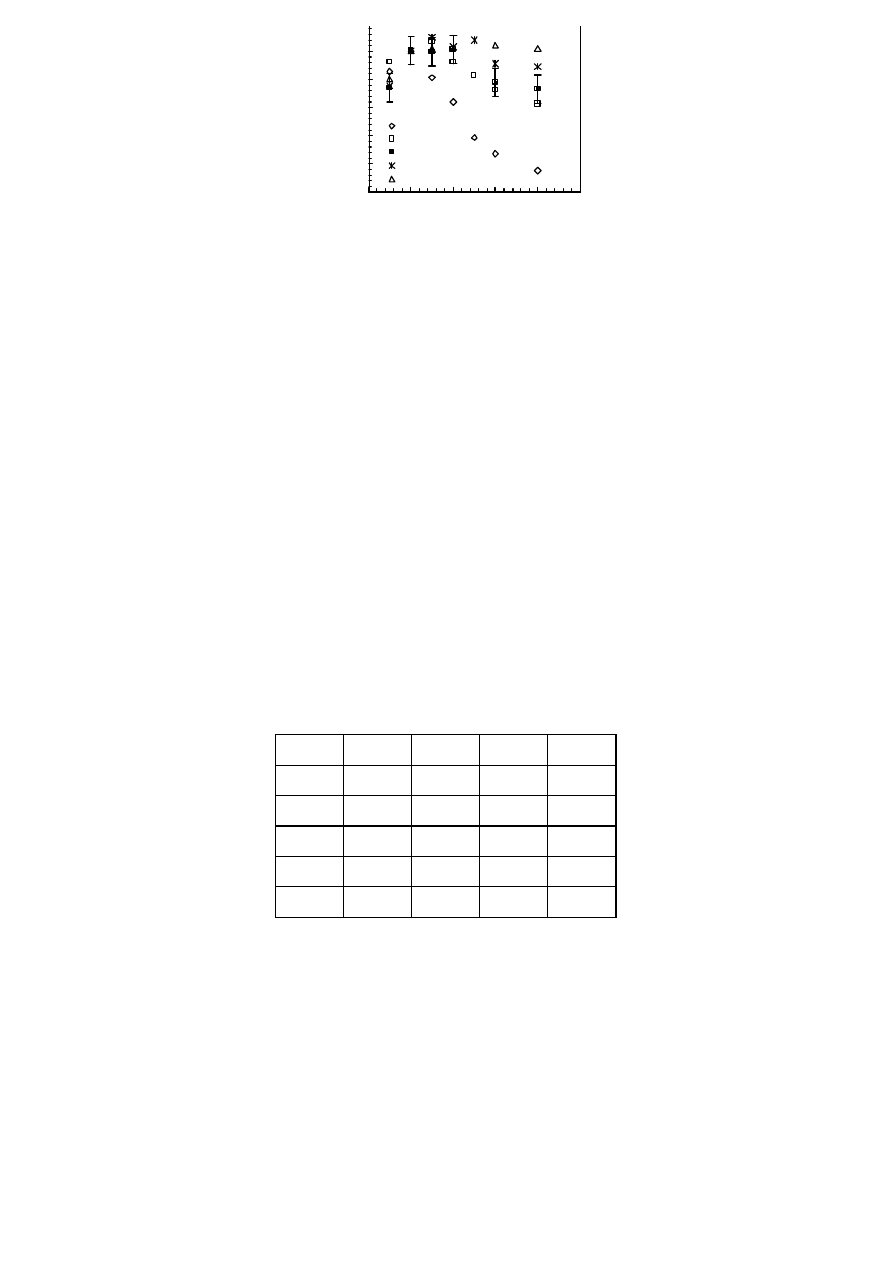
106
5.2.3.3 SSD CORRECTION FACTOR WITHOUT TRAY
Table 5.7 shows the variation of C
SSD
for different linacs fo r unmodified old type EDP-20
diodes. For the same quality index the difference in SSD correction factors (at a given SSD)
reaches 1 % at maximum at small SSDs. When decreasing the SSD from 100 to 70 cm, C
SSD
decreases by about 7 % for 18 MV photon beams with a QI = 0.78, and around 10 % for a
QI = 0.77.
In 18 MV and 25 MV photon energies provided by the GE Sat 43 and/or Sat 42 linacs, SSD
correction factors without tray are almost independent of build -up cap thickness for all
types of diodes. If the total build-up cap thickness does not exceed 30 mm, C
SSD
for the
same diode with and without additional build -up varies by less than 1 % at a given SSD.
Maximum deviations of more than 1.5 % between C
SSD
of unmodified and modified diodes
(at a given SSD) are observed only if the total build -up thickness reaches 40 or 45mm.
Centre
Charleroi
Leuven
Leuven
St. Jean
Unit
Ph SL 20 GE Sat 43 GE Sat 42 GE Sat 42
SSD [cm] QI=0.78
QI=0.77 QI=0.77
QI=0.78
100
1.000
1.000
1.000
1.000
90
0.981
0.975
0.976
0.980
80
0.960
0.940
0.941
0.958
0.95
0.96
0.97
0.98
0.99
1.00
1.01
0
10
20
30
40
50
square field size (cm)
C
FS
EDP-30
EDP-30/25
EDP-30/30
EDP-30/35
EDP-30/40
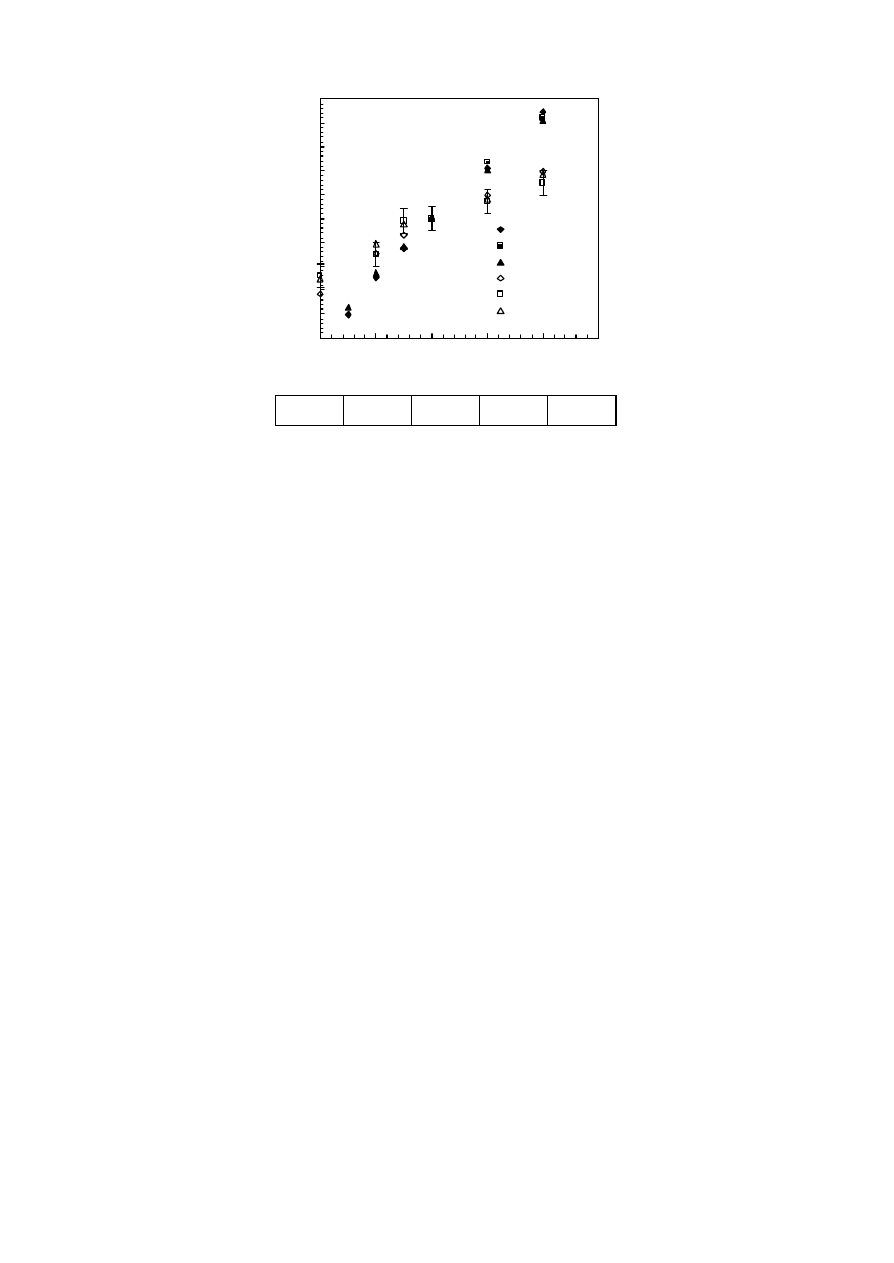
107
70
0.930
0.898
0.908
0.923
Table 5.7 Variation of SSD correction factor for unmodified old type
EDP-20 diodes at 18
MV photon beams measured in different Belgian radiotherapy centers.
Figure 5.15 Variation of the source-surface correction factor C
SSD
with additional
build-up for new and old type EDP-20 diodes in 18 MV photon beams
provided by a GE Sat 43 linac. All results are obtained w ith copper build-
up caps.
The new type of EDP-20 diodes shows a much smaller variation of C
SSD
with SSD than the
old type. For new type EDP-20 diodes C
SSD
increases by about 4-5 % at 18 and 25 MV from
GE linacs when increasing the SSD from 80 cm to 120 cm. This variation exceeds 10% for
the old type EDP-20 for almost all build-up cap combinations. Figure 5.15 shows the C
SSD
variation as a function of source-surface distance and build -up for new and old type EDP-
0.95
0.96
0.97
0.98
0.99
1.00
1.01
1.02
1.03
1.04
1.05
80
90
100
110
120
130
SSD (cm)
C
SSD
OLD EDP-20
OLD EDP-20/30
OLD EDP-20/40
NEW EDP-20
NEW EDP-20/30
NEW EDP-20/40

108
20 diodes in 18 MV photon beams provided by a GE Sat 43 linac. The error bars indicate the
accuracy of
±
0.5 % in the determination of diode correction factors. All results of modified
diodes displayed in Figure 5.15 are obtained with copper build -up caps.
For EDP-30 diodes with a total build -up less than or equal to 30 mm, C
SSD
increases by
about 3.5 - 4.5 % at 18 and 25 MV when increasing the SSD from 80 cm to 120 cm. In 25 MV
photon beams this variation is only 2% for the modified EDP-30/45(Cu) diode.
5.2.3.4 INFLUENCE OF BEAM MODIFIERS: TRAY AND BLOCK CORRECTION
FACTOR C
T
AND C
B
Without additional build -up C
FS
values for a 40 x 40 cm
2
field with and without tray show
variations up to 2% for EDP-20 and 3% for EPD-30 diodes. This difference decreases to
about 1 - 1.5 % for a 30 x 30 cm
2
field and to less than 1 % for fields up to 20 x 20 cm
2
.
For unmodified diodes the SSD correction factor with and without tray varies by about 1.5
–2 % at a SSD of 80 cm. This variation is almost independent of energy and t ype of diode.
For SSDs between 90 and 120 cm the influence of the tray on C
SSD
is less than 1%.
The influence of the tray at small source-surface distances and for large field sizes can be
decreased by adding build -up. For modified EDP-20/30(Cu) and EDP-30/30(Cu) diodes
correction factors with and without tray, field size correction factors C
FS
as well as source-
surface correction factors C
SSD
, differ by less than 1%.
Table 5.8 shows the variation of block correction factors as a function of blocked field size
for different types of diodes and linacs. The collimator setting is kept constant at 20 x 20
cm
2
for all blocked fields. The build -up material is indicated by its chemical symbol.
For unmodified old type EDP-20 diodes block correction factors at 18 MV provided by the
Philips SL 20 linac do not differ by more than 1 % from unity, even when reducing the field
size to 5 x 5 cm
2
for a fixed collimator setting of 20 x 20 cm
2
. For the GE Sat 42 linac, C
B
reaches 1.032 at 18 MV for t he smallest field size. If sufficient build -up material is provided,
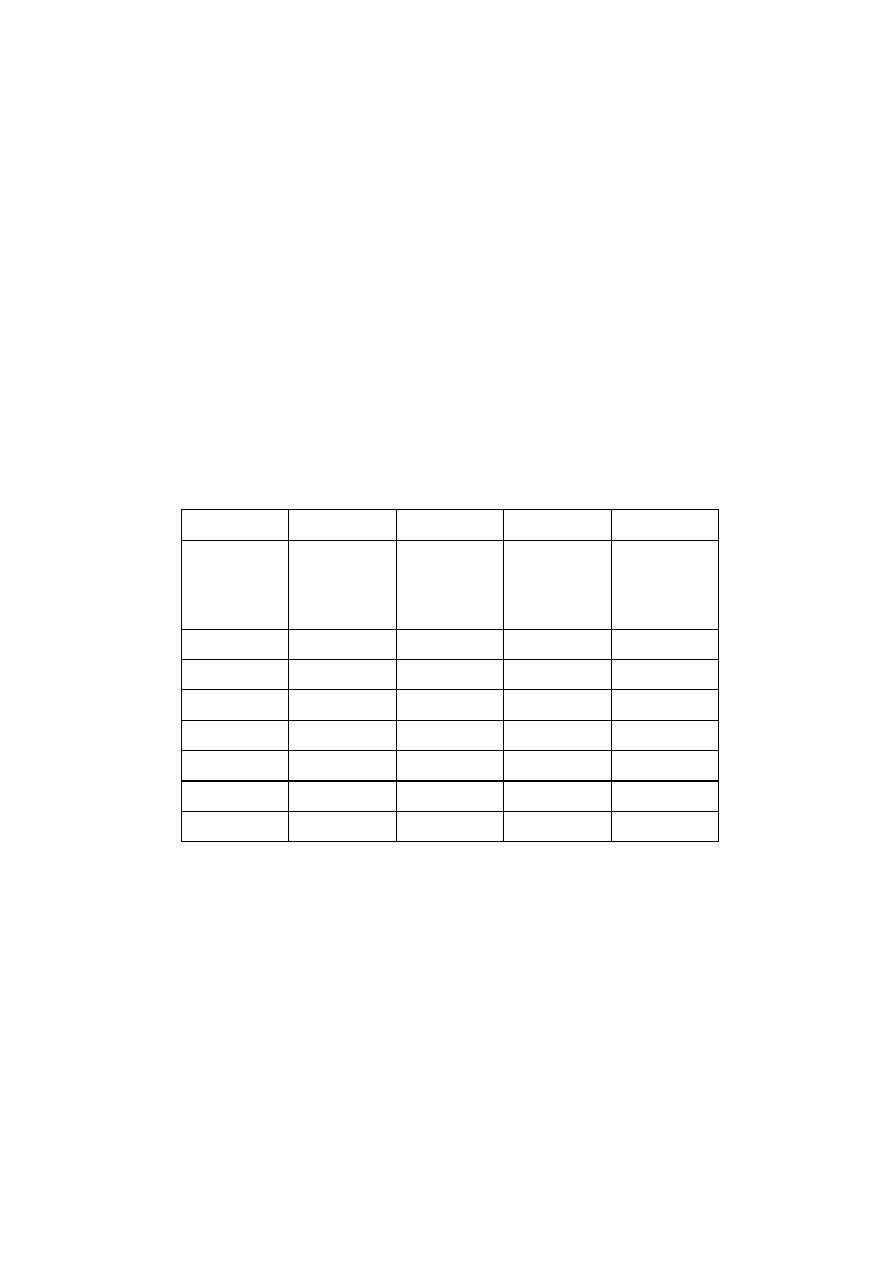
109
the influence of blocks can be significantly reduced. For the modified EDP-20/30 at 18 MV
from the GE Sat 42 C
B
could be reduced to 1.4% for the blocked 5 x 5 cm
2
.
5.2.3.5 WEDGE CORRECTION FACTORS
Wedge correction factors at 18 and 25 MV are of the order of 1.01 - 1.02 for new type EDP-
20/30(Cu) and EDP-30/30(Cu) diodes, and reach 1.06 - 1.07 for the old type EDP-20/30(Cu)
diodes.
The variation of the wedge correction factor C
W
with field size is less than 1 % for modified
and unmodified new type EDP-20 and EDP-30 diodes at 18 and 25MV. Only for unmodified
old type EDP-20 diodes a small field size dependence could be observed: the C
W
difference
between a 5 x 5 cm
2
and a 20 x 20 cm
2
field reaches 2 % at 25 MV and is slightly higher than
1 % at 18 MV. With additional (copper) build -up (old type EDP-20/30 or EDP-20/40) this
variation is reduced to less than 1 %.
Centre
Charleroi
Leuven
St. Jean
Middelheim
Unit
Energy
QI
Ph SL 20
18MV
0.78
Sat 42
18MV
0.77
Sat 42
18MV
0.77
Sat II+
23MV
0.79
FS [cm]
EDP-20
EDP-20
EDP-20/30 (Fe)
EDP-20
5.0
1.009
1.032
0.986
1.032
8.0
1.007
1.032
0.993
1.028
10.0
1.007
1.026
0.997
1.025
14.1
1.000
1.012
0.999
1.017
17.3
1.003
1.007
-
1.012
20.0
1.000
1.000
1.000
1.000

110
Table 5.8 Variation of block correction factor for several unmodified and modified
diodes for higher energy photon beams measured in different Belgian
radiotherapy centres. The results of EDP-20 diodes refer to the old type.
5.2.3.6 CORRECTION FACTOR VA RIATION WITHIN THE SAME BATCH
The correction factor variation for diodes from the same batch is estimated from
measurements using unmodified diodes, which show the largest C
FS
variations. The C
FS
difference for a given field size is less than 1 % for two EDP-20 diodes and reaches 1.3 % as
a maximum for the three EDP-30 diodes. The difference of SSD correction factors for a fixed
SSD is less than 1 %, for both types of diodes. The small deviation of correction fac tors for
diodes from the same batch is in agreement with observations from other authors [Fontenla
1996b]. It can therefore be concluded that it is sufficient to determine correction factors for
one diode of the same batch only.
5.2.3.7 PERTURBATION EFFECTS
Perturbation effects are determined for old and new type EDP-20 and EPD-30 diodes with
and without additional copper build -up caps in a 10 x 10 cm
2
field at 18 and 25 MV. The
relative dose reduction (dose reduction in % with respect to the flat part of the profile at a
specific depth) for unmodified old and new type EDP-20 diodes is about 7-8 % at 18 MV,
and 6-6.5 % at 25 MV, respectively. The corresponding values for the unmodified EDP -30
diode are between 3 % and 3.5 % at 18 and 25 MV, respectively. Depending on energy and
depth, these values are increased by 2-3 % when adding copper build -up caps.
The additional build -up caps have thickness typically around one mm and increase
therefore the area where perturbation effects are present.

111
5.2.4 DISCUSSION
5.2.4.1 INDEPENDENCE OF FIELD SIZE AND SOURCE-TO-SURFACE DISTANCE
CORRECTION FACTORS
For SSDs larger than or equal to 80 cm equation (13) is valid within an uncertainty of 1.5 %
at 18 - 25 MV if the total build -up cap thickness does not exceed 30 mm. It should be noted
that the accuracy in the determination of diode correction factors is better than ± 0.5 %.
The validity of equation (13) within a certain limit has to be considered when defining
tolerance and action levels for entrance dose measurements in higher energy photon
beams, especially at small or large SSDs.
The head-scatter variation of a therapy unit depends strongly on treatment head geometry
([Dutreix 1997], [Nilsson 1998], [Sixel 1996], [Van Gasteren 1991]), and GE linacs are known
to have a pronounced head-scatter variation with field size. Therefore, the independence of
C
FS
and C
SSD
was checked on two GE linacs. Since field size correction factors vary much
less for other linac types (see Table 5.7) the findings for the GE linacs are considered to be
valid for other linacs, too.
5.2.4.2 TOTAL BUILD-UP THICKNESS OF THE DIODE
For EDP-30 diodes the smallest variation of the field size correction factor at 18 MV is
obtained with an additional water equivalent (copper) build -up thickness of 15 mm. The
results for both types of EDP-20 diodes are in good agreement with this. At 18 MV, as well
as at 25 MV, for old and new EDP-20 diodes the smallest FS correction factor (C
FS
)
variation is observed when adding 10 mm water equivalent build -up material, which also
corresponds to about 30 mm depth. This optimal depth has been confirmed using different
build-up cap materials: copper, lead and iron. It should be noted that even with a modified
EDP-10/30(Cu) diode a 1.6 % C
FS
variation is seen at 18MV for the Ph ilips SL 20 linac when
the field size varies between 6 x 6 and 35 x 35 cm
2
. For EDP-30 diodes in 25 MV photon

112
beams, the C
FS
variation of unmodified diodes could not be decreased by adding build -up.
The different diode response at 25 MV for EDP-20 and EDP-30 diodes is most probably due
to the difference in build -up material of the unmodified diodes (stainless-steel versus
tantalum).
5.2.4.3 TREATMENT UNIT DEPENDENCE
For the same diode or diodes from the same batch, field size and source-surface distance
correction factors measured at 18 MV on the GE Sat 43, equipped with an MLC, and
measured on the GE Sat 42, having a conventional collimator (CC), agree mostly within 1%.
The main difference between the two linacs are the collimators, while the flattening filter
position and design are similar. Due to the different collimator design they show a
difference in head-scatter variation with field size (12 % for the GE Sat 43+MLC linac versus
16 % for the Sat 42+CC linac when increasing the field size from 4 x 4 to 40 x 40 cm
2
), but the
depth dose characteristics in the build -up region are almost identical. This finding is in
agreement with a study where two different collimators have been mounted subsequently
on the same accelerator, while all other parts of the linac rema ined the same [Georg 1997].
Here, it has been shown that the depth of maximum dose as well as the skin dose is almost
independent of collimator design while the head-scatter variation is not. Similar doses in
the build -up region but different head-scatter variation may be explained by contaminating
electrons emanating from the flattening filter, which is the main source of contaminating
electrons at higher energies ([Nilsson 1985], [Nilsson 1986], [Sjögren 1996]). The head -
scatter variation, on the other hand, has to be determined at depths large enough to avoid
the unpredictable influence of contaminating electrons in order to describe the field size
variation of the primary photon component [Dutreix 1997].
The same arguments can be used to explain the difference in diode correction factors for
the same type of diode for the same photon beam quality but provided by linacs from
different manufacturers.

113
5.2.4.4 BEAM MODIFIERS
Even for large field sizes at small SSDs the influence of the tray could be decreased to
negligible values when adding additional build -up caps. It should be noted that the
thickness of the tray holder is only 8 mm; thicker trays may have a larger influence.
Additional build -up material also reduces the influence of blocks to less than 1% for
clinical relevant applications. The influence of trays and blocks can be explained by
contaminating electrons. At higher energies the dose contribution of contaminating
electrons produced by trays and blocks is only about 5 – 10 % at depths around 3 - 4 cm,
but between 20 and 40 % at depths up to 2 cm ([Bjärngard 1995], [Sjögren 1996], [Zhu
1998]).
Block correction factors for modified diodes have to be taken into account only when the
field size is substantially reduced by blocks (see Table 5.8). Large field reduction by blocks
can reduce the area of flattening filter seen by the detector which might be accounted for
by a field size correction factor rather than by a block correction factor. However, such
block applications are clinic ally less relevant.
The different doping level for the new type EDP-20 diode was introduced in order to
improve the dose rate linearity of the diode after dose accumulation [Grusell 1993].
Therefore the new type EDP-20 diodes show a smaller variation of SSD correction factors
as well as a smaller wedge correction factor.
5.2.4.5 PERTURBATION EFFECTS
The relative dose reduction caused by the diode is almost independent of depth, which is
in agreement with investigations performed with diodes from another manufacturer [Alecu
1997]. The attenuation at higher photon energies induced by unmodified EDP -20 diodes is
somewhat larger than previously reported values for Scanditronix diodes ([Leunens 1990b],
[Nilsson 1988], [Rikner 1987]), while it is smaller for the EDP-30. When adding build -up
caps these perturbation effects are increased for all diodes, but they are still smaller than

114
the 13 % attenuation in a 15 MV photon beam reported for a diode with a cylindrical build -
up cap [Alecu 1997] and Section 5.1.1.
When performing in vivo dosimetry on a weekly basis and assuming a perturbation effect
of 10 %, the dose reduction due to the presence of the diode will be 2 % for treatments with
5 sessions per week. This value can even be reduced by care fully varying the diode
position for each in vivo measurement or by restricting the in vivo procedure to the
beginning of a treatment.
5.2.5 CONCLUSION
When performing entrance dose measurements at the depth of maximum dose, the diode
correction factors accounting for non-reference conditions strongly depend on
contaminating electrons, whose dose contributions at shallow depths vary with treatment
geometry and treatment unit. The build -up thickness of commercial diodes is not sufficient
to exclude this influence at higher photon energies. In the energy range between 18 - 25
MV a total diode build -up thickness of 30 mm is found to be the ‘best compromise’ for all
types of diodes and treatment units considered. An additional advantage of a build -up cap
modification when using commercial diodes at higher energies, is the reduction of the
influence of beam modifiers. The additional perturbations caused by the increased build -up
thickness do not have an influence on the practical aspects of in vivo dosimetry (for
instance the frequency of measurements) compared to unmodified diodes.

115
5.3 PRACTICAL IMPLEMENTATION OF COST-EFFECTIVE APPROACHES TO
IN VIVO DOSIMETRY - THE EDINBURGH EXPERIENCE
5.3.1 INTRODUCTION
A systematic programme of in vivo dosimetry using diodes to verify radiotherapy delivered
doses was begun in Edinburgh in 1992. Prior to that, TLD -based in vivo dosimetry had
been used for some considerable time, but only for critical organ dosimetry and for
verification of complex treatments, such as TBI and TSEI. [Thwaites 1990] This has
continued. In 1991, a Scanditronix DPD-6 electrometer and a set of p-type silicon diodes
(EDE, EDP-10, EDP-20) was purchased with the following initial aims:
•
to investigate the feasibility of routine systematic use of diodes as part of a
comp rehensive QA programme
•
to carry out clinical pilot studies to test each machine, treatment site and treatment
technique to assess the accuracy of the overall radiotherapy process at the point of
dose delivery
•
from this, to identify and rectify any systematic errors, and also
•
to measure global (as well as specific treatment machine and technique) dosimetric
precision to compare to clinical requirements
As the programme progressed, further electrometers (DPD3 and DPD510) and diodes
(EDD2, EDD5, newer-style EDP-10 and EDP-20, all Scanditronix) were acquired and
additional aims were developed linked to routine implementation. From the results of the
clinical pilot studies, a cost-benefit evaluation was carried out to consider how best to
utilise the diodes in ro utine practice, including consideration of:
•
when to use and on which patients
•
what should be measured in a routine programme
•
who should do what
•
what tolerance and action levels to adopt
•
what action should be taken

116
At the same time, further work was initiated to attempt to simplify the routine
implementation to make it as cost-effective as possible. This has included:
•
comparison of the use of correction factors versus no correction factors
•
the use of additional build -up caps on the standard diodes to minimi se the ranges of
correction factors required
•
the use of combined mid -range ‘generic’ correction factors for a specific modality,
treatment site/field and diode position
•
how data is communicated and recorded, to and from the treatment unit
•
how the diodes are mounted and handled in the treatment room
•
the quality control required for the diodes themselves
The department was fortunate in having a steady supply of multi-disciplinary Master’s
level students interested in the work, who carried out dissertation projects at the testing
and development stages under the supervision of the physicist in charge of the diode
project. Trainee physicists have investigated the initial physics testing and workup of the
systems, including calibration and corrections of the dio des ([Kidane 1992], [Brown 1996])
and phantom and clinical pilot studies [Brown 1996]. A part -time (one day per week)
research radiographer, working within the physics department has been involved with the
project since soon after it started and has carrie d out work on initial clinical implementation,
clinical pilot studies, routine implementation and methodology ([Blyth 1997], [Blyth 2001]).
Trainee radiation oncologists have carried out clinical pilot studies ([Millwater 1993],
[Millwater 1998], [Elliott 1999]). At the time of writing, a number of papers are in
preparation, or submitted, covering various aspects of this programme ([Blyth 2001a],
[Blyth 2001b], [Elliott 2001]).
Implementation on the linacs in the department has been gradual. Initial detail ed studies
were carried out on just one linac, then this has been extended one-by-one to all linacs in
the department. Routine implementation has also been rolled out gradually. Thus different

117
stages of the programme have been in operation on different lin acs at the same time. This
process is not yet complete. At the time of writing, the department is undergoing a major
re-equipping. Allied to this, new diode mounts are being installed in each room, as new
linacs are installed, to enable routine use on all treatment machines.
The following sections briefly discuss the approaches which have been taken in
development and those adopted for routine usage in the department, with an emphasis on
cost-effective, reliable, readily -usable methods. It should be noted that the solutions
chosen are specific to the department. The optimum solutions are not necessarily the same
for every department (nor even for every treatment type within a given department), as
they are influenced by the resources available, the level of implementation, the accuracy
deemed necessary, the other aspects of the department’s quality system and QA
programme in operation, etc. However it is observed that many of the solutions have been
arrived at independently by other departments who have gone through a similar process,
including others contributing to this booklet. Where details are similar and are discussed in
other chapters or sections, they will not in general be repeated here.
5.3.2 INITIAL PHYSICS TESTING AND WORKUP
A conventional approach wa s taken to the initial physics testing and workup. Whilst this
is time-consuming, it is necessary to carry this out in full detail at the outset, whatever the
level of routine implementation is to be. Confidence in the diode programme results, in the
evaluation of clinical pilot studies and in the tolerance levels applied can only be based on
a comprehensive commissioning and evaluation of the diode systems. Thus initial testing
included (see Sections 1.2.1, 5.1): stability of diode signal (leakage), reproducibility of
system response to repeated irradiations, measurement linearity, check on water-equivalent
depth of the diodes and measurement of the related perturbation of the radiation field
beyond the diodes.

118
Following this, entrance and exit dose calibrations were carried out (see Section 1.2.2 and
[Millwater 1997]), comparing diodes to a calibrated ion chamber irradiated simultaneously.
The calibration phantom used wa s of 30 x 30 cm
2
epoxy -resin water-equivalent plastic and a
standard thickness of 15 cm was chosen. The phantom was set up over the thin meshed
area of the treatment couch. For entrance dose calibration, the ion chamber was positioned
at the depth of dose maximum and an SSD of 100 cm was set. To minimise subsequent
routine calibration times, the methodology tested and implemented was to position a
number of diodes spaced around the central axis for calibration, sufficiently far out so as
not to perturb the ion chamber reading. A field size of 15 x 15 cm
2
was selected, to ensure a
sufficient field margin around this ring of diodes. The dose calculated from the calibrated
ion chamber was corrected for the displacement factor, whilst the diode readings were
corrected for the small measured beam non-flatness at their distance out from the central
axis. For exit dose calibrations, the ion chamber and diodes were left in the same positions,
the gantry rotated to 180o, the SSD was reset to 100 cm and simultaneous irradiations were
again carried out. As the exit diode is to be used to compare measured doses against those
calculated using local planning data, the exit calibration factors were corrected for the
measured lack of scatter to the ion chamber at its exit calibration depth (build -down effect).
Entrance and exit correction factors were determined for each individual diode. Standard
methods were used for this (e.g. Sections 1.2.3 and 5.1; [Van Dam 1994], [Mayles 2000]) and
similar magnitude corrections were obtained to those reported in the literature. Correction
factors were determined for each beam for field size, SSD, tray, wedge, blocks, incident
angle and temperature. All were investigated for both entrance and exit measurements. In
addition for exit measurements, the correction factors for phantom thickness were
determined.
Following all of this initial work, irradiations were carried out on phantoms, comparing
diode-measured doses to expected doses in a variety of situations to test the applicability

119
of the methodology and the validity of the calibration and correction factors. In addition
detailed phantom studies have been carried out to aid in relating entrance and exit dose
measurements to isocentre dose estimation, in order to compare measured doses to
prescribed target volume doses.
At this stage, a quality control programme was implemented for the diodes. Initially this
included checks on calibrations approximately monthly and on correction fac tors
approximately yearly [Mayles 2000]. In addition records were begun of the approximate
cumulative doses that each diode had received, as an indication of whether checks should
be more frequent. It was recognised with experience that calibration factors can be
routinely and frequently checked in practice by using the diodes in the linac daily check
procedures, building in a quick consistency check against an ion chamber on at least a
weekly basis. A quick check on correction factor validity can be carrie d out using a second
SSD measurement (see Section 1.2.4). If any of these show significant changes then this
indicates the need for more detailed checks.
5.3.3 PILOT CLINICAL STUDIES
Pilot clinical studies were carried out for diffe rent treatment machines, beams, treatment
sites and treatment techniques. Simpler situations were investigated first, e.g. flat surfaces,
shells, perpendicular incidence, etc., where diode positioning problems were expected to be
less, whilst the underlyin g methodology was tested in the clinical setting. Entrance and exit
doses were measured once per week throughout treatment. All relevant correction factors
were applied to the measurements. The only exception to this was the temperature
correction, as the diode was generally positioned after field setup and just before
irradiation, therefore it was felt in most circumstances that the correction required due to
the temperature change was minimal. Temperature corrections were applied if the diode was
in posit ion for a significant
time. Diodes were positioned wherever possible on the beam
central axis, but account was taken of block presence, asymmetric field position etc. where
appropriate. The doses were compared to expected entrance and exit doses calculated from

120
the planning data, and the deviations were quantified. These were used to estimate target
volume prescription point dose deviations from the individual fields, aided by the phantom
studies. The values for all fields were combined in proportion to the weight of the field to
provide an estimate of the overall deviation of delivered dose from prescribed dose for the
whole treatment. For tangential field breast treatments, the diodes were placed at a point
midway between the field centre and the medial border of the medial field and used there to
measure entrance dose from the medial field and exit dose from the lateral field. The
combined corrected dose was compared to the dose value from the plan at the appropriate
depth below this measurement point.
In all the clinical pilot studies measurements were repeated on a weekly basis throughout
treatment. The observed deviations from all measurements on the same patient were
averaged to provide the best estimate of the overall treatment course deviation betwee n
delivered dose and prescribed dose to the target volume prescription point.
Detailed results are discussed elsewhere, but in summary:
•
Typical distributions of individual entrance dose results for various clinical pilot studies
showed mean differences, measured to expected, close to zero. Standard deviations lay
within the range 1.2 % to 4.1 % (typically 1.5 – 3 %), depending on site and linac.
•
Exit doses showed mean (systematic) differences varying with site, field and method of
treatment planning. Typic ally mean measured doses were observed to be lower than
expected by 1 – 4 %. Standard deviations were within the range of 1.9 – 5 % (typically 3 -
4.5 %)
•
For total treatment course dose delivery to the target volume (prescription point), some
examples of mean deviations (followed by SD), from the combination of all fields and
using all information from repeated measurements are:
head and neck:
-0.2 to +1.0 % (1.5 – 3 %)

121
breast:
-4 %
(2.5 %)
(old technique, isocentre on surface, half beam in air [Redpath 1992])
breast:
-2 %
(2.7 %)
(new technique, isocentre at depth, less beam in air [Carruthers 1999])
pelvic:
-0.4 %
(2.7 %)
conformally blocked prostate and bladder(initial):
+1.5 %
(2.6 %)
conformally blocked prostate and bladder(corrected):
+0.1 %
(2.6
%)
The SD for the distribution of observed differences of estimated prescription point doses
(from combined field measurements) from the expected values was normally lower than the
SD for individual field data. Similarly the SD for measurements which were repeated on the
same patient and averaged over the treatment course was lower than the s.d for individual
measurement data. Some of the reasons for observed discrepancies between measured and
expected doses, on investigation, were found to be due to the in vivo methods. These
include diode positioning problems such as contact, cable pulling, etc.; positioning
difficulties such as entrance or exit through couch, etc.; wrong correction factor use;
measurements through immobilisation devices, etc.; the limiting resolution of the diode
electrometer for small dose wedged components of fields; diode positioning uncertainties
under large wedges or on steeply angled surfaces. On the other hand some causes were
identified as real differences in delivered dose, due to treatment machine performance, to
patient data acquisition, to dose calculation errors (e.g. for tangential field breast
irradiation), to the use of non-CT planning in some situations, to patient set-up variations,
and to incorrect treatment parameters. Some causes were due to changes in the patient at
the time of treatment as compared to the plan, for instance systematic patient size and
shape changes, or random changes such as bowel gas in line with the diode, etc. Some
causes were a combination of factors. The conformal blocked treatments illustrate one such
case. The initial mean deviation was observed to be + 1.5 % (apparent measured dose
greater than expected). On investigation approximately half of this difference was due to an

122
incorrect correction to the diode reading to account for the presence of the conformal
blocks (i.e. diode use and methodology) and approximately half was due to the MU
calculation in these situations (i.e. real change to delivered dose to the patient). On
correcting both of these errors the mean deviation subsequently measured was 0.1 %. This
example nicely illustrates that all discrepancies should be investigated, that diode
dosimetry is precise enough to identify problems at the 1 %, or sub-1 %, level if the system
is implemented carefully and that the diode methodology and use can itself introduce
errors, which should also be suspected and investigated when discrepancies are observed.
As an overall measure of global accuracy of the delivered radiotherapy doses in the
department, considering more than 5000 individual entrance dose measurements, the mean
dose ratio (measured to expected) is close to unity (1.001) and the standard deviation is
close to 3%. This, of course, also inherently includes the uncertainties associated with the
diode measurements.
Tolerance levels were chosen on the basis of the pilot studies, at approximately 2 SD, with
the aim of not being too wide that significant problems were missed, but not too narrow
that time-consuming investigations were triggered which were inconclusive or which gave
rise to reduced confidence in the system. 5% was selected for entrance dose measurements
and 8% for exit doses (although tighter tolerances of 3% and 6% may be applied for
conformal treatments, especially if dose escalation is involved. However this requires a
greater effort to achieve than for the general routine use).
5.3.4 ROUTINE USE
Having carried out the detailed studies outlined above, multidisciplinary discussion then
centred on how the department was to utilise diode verification dosimetry in routine
practice. For this the daily positioning and recording was to be passed from the research
radiographer to the normal treatment unit radiographers, unit by unit as the routine use was

123
rolled out to the linacs one-by-one. Possible usage and the procedures involved were
evaluated in terms of cost-effectiveness and with the aim of minimising the time involved at
the treatment units, as the patient workload per linac in the department is high.
The decisions on how and wh en to use diodes routinely, and the rationale for each, were:
•
to measure only entrance doses for routine radiotherapy treatments, as the
department’s main aim for routine use was to identify significant errors in treatment,
which had not been picked up by the other levels of the quality system, which includes
independent plan calculation checks, independent MU checks, independent check of
information into the verification system and independent radiographer checks on
treatment parameters and patient set-up. It was felt that entrance dose checks were the
most cost-effective way to do this, independently checking the combination of MU,
beam parameters, beam modifiers, patient position and machine performance in a
relatively simple way. To carry out exit dose checks on a routine basis, there is a
significant increase in the time and resources required, without a similar significant pay -
back.
•
to initially aim to check all patients, building up to this gradually, linac-by-linac, as the
pilot studies had not shown any situations which were significantly worse or better
than others. The aim is to re -assess this decision periodically, taking into account the
outcome information of the diode programme as it progresses.
•
to normally take just one measurement on each patient, which must be carried out
within the first few days of treatment, ideally within the first two fractions, but in no
circumstances more than one week into treatment, so that any problems are identified
early in treatment and rectified. Frequently, dio de measurements are carried out on each
linac on one particular day and all new patients on that machine are monitored. This
implies that the number of patients monitored on each machine per week is generally in
the range of 8 - 12.

124
•
to apply a general tole rance level of 5 % to individual entrance dose measurements, as
discussed above. The action level is also made equal to the tolerance level, i.e. all
deviations above 5 % are investigated.
•
the actions taken if a deviation is observed over this level have evolved with time.
However this department has come independently to a very similar scheme to that
developed in the Leuven department, as discussed in Section 2.2, Figure 2.2 of this
booklet. On-the-spot checks are carried out on the treatment machine when significant
discrepancy is noted. These checks include patient position, diode position, beam
parameters, etc. In addition, at the earliest opportunity, the treatment unit staff notify a
responsible me mber of the physics department, who checks treatment plan,
calculations, treatment information transfer, information in the verification system,
expected signal from the diode, etc. and looks for possible reasons why there may be a
deviation. Whether or not a reason is identified, and unless a trivial reason is
recognised, a second check would be made on the following fraction, with a member of
the physics department present. If this measurement is within tolerance, then the
treatment is deemed acceptable. If not and the same immediate or afterwards checks do
not identify a valid reason, then the physics department organises a phantom study to
simulate the treatment, comparing ion chamber measurements to the diode to decide
whether the treatment should continue without change or not, i.e. investigating both
the clinical irradiation and the diode behaviour in this situation.
In addition to the above, the routine in vivo dose measurement programme aims to carry
out full entrance and exit
dose studies (and estimation of target volume dose from these)
on selected groups of patients for:
•
newly commissioned treatment units, and/or new treatment techniques, or following
major changes in planning systems or planning calculations, to ensure that the whole
system is tested in these circumstances; in particular in case any potential problems
have been overlooked

125
•
full studies on critical patient/treatment groups, for instance dose escalation groups
(with improved tolerances, as discussed above), TBI (but here using TLD), etc.
•
and occasional full audit studies on selected groups of limited numbers of patients, as a
repeated overall check on both the diode methods and on the total radiotherapy
process.
All these essentially mirror the clinical pilot studies in operation and are carried out by
physics personnel and/or the research radiographer, in conjunction with the radiographers
on the particular treatment unit.
5.3.5 METHODS TO SIMPLIFY ROUTINE USE
A number of things have been investigated and some implemented in an attempt to
simplify routine diode use, to make it as cost-effective as possible and in particular to
minimise the time involved at the treatment unit. This has included:
5.3.5.1 POSSIBLE OMISSION OF CORRECTION FACTORS
A full set of correction factors was applied to all the measurements in the clinical pilot
studies. At this stage it is necessary to obtain the best accuracy possible. However for
routine use on routine treatments (although not necessarily so for critical groups, such as
dose escalated patients), it was thought possible that a simpler approach, omitting
correction factors might be applicable. The advantages would include a simpler
methodology and less quality control on the diodes. Initially a comparison was carried out
for patient groups from the clinical pilot studies, where dose estimates made by removing
the correction factors were evaluated. Typically the mean value changed by acceptable
amounts, depending on site, but the standard deviation generally increased significantly.
This implied that an increased tolerance level would have to be used and would have lead
to situations where some significant clinical discrepancies in dose would have not been
recognised. Therefore this approach was deemed not acceptable. Given that the same

126
diode systems are to be used for the more critical groups, it is still necessary to measure
correction factors and to make quality control checks on their values.
5.3.5.2 THE USE OF BUILD-UP CAPS
Build-up caps have been constructed for the diodes to match the build -up more closely to
the beams in the department, with the aim of reducing the spread of correction factors
dependent on secondary electron and photon spectrum effects (see also Section 5.2 for
‘high energy’ beams). Unmodified EDP-10 diodes were appropriate for the 4 MV beam and
unmodified EDP-20 diodes were appropriate for the 8 - 9 MV beams. However, additional
caps of 0.6 mm of brass, in combination with EDP-10 diodes, have been investigated for the
6 MV beams. For the 15 and 16 MV beams, additional caps of 1.2 mm of brass, copper and
stainless steel, in combination with EDP-20 diodes, have been studied. These additional
caps bring the build -up thickness to 15 mm water-equivalent for 6 MV beams and 30 mm
water-equivalent for 15 – 16 MV beams. Calibration and correction factors were measured
for both ‘old -style’ and ‘new-style’ EDP-10 and EDP-20 diodes with these caps. Detailed
results are reported elsewhere ([Blyth 2001a], [Blyth 2001b]).
In summary:
•
the caps produce a reduced range of those entrance correction factors which depend at
least in part on secondary electron and photon spectrum effects, such as field size, tray,
block, wedge, etc.
•
in general, the caps improve the situation to the stage that the correction factors can be
ignored, i.e. the spread is within ± 0.5 %, for instance field size, trays, etc., or a varying
factor can be replaced by one single factor, e.g. for the motorised wedge for all field
sizes
•
the changes were observed to be significantly less for Scanditronix ‘new-style’ diodes
than for ‘old -style’ diodes, in that the newer versions have less variation on some of
these factors to begin with.
•
there is little change in the range of factors for exit measurements

127
•
the range of values for some correction factors, such as for angle of in cidence, are made
worse
•
the shadowing effect is, of course, increased by the use of caps. However as the
number of times that measurements are carried out on an individual patient in the
department is small, even in the full studies where measurements are repeated once per
week, this does not present a significant problem.
•
the gains were less obvious for the high energy beams (15 and 16 MV) than for the 6
MV beams.
Additional build -up caps of 0.6 mm brass are currently routinely used for all our 6 MV beam
diode measurements. The routine use of build -up caps for 15 and 16 MV beams is still
under discussion.
5.3.5.3 THE USE OF ‘GENERIC’ CORRECTION FACTORS
The use of ‘generic’ correction factors has been investigated for the case of standard
diodes as well as for dio des with build -up caps. For a given treatment modality and for a
specific treatment field, the range of treatment parameters has been investigated for a
representative sample of patients. For each relevant parameter the range of the appropriate
correction factor has been considered and a combined correction factor calculated from the
mid-range values (or the values judged to be most representative). In some cases this has
required a judgement on, for example, the range of beam fractions that are wedged and
unwedged in particular clinical situations (for motorised wedge machines) and a weighted
wedged/unwedged correction factor to be included, etc. In general, the range of overall
correction factors around this generic correction factor is small for the norma l range of
treatment parameters used for different patients for a particular field in a particular type of
treatment. Also this is generally better when build -up caps are used, as the range of a
number of correction factors is reduced.

128
Generic correction factors are currently in use for routine entrance dose measurements for
our 6 MV beams using diodes with build -up caps. Tables of generic correction factors are
available, listed by diode, treatment unit and modality (where normally one specific diode
and electrometer combination are assigned routinely to a given treatment modality), by
treatment technique and by treatment field. In this way, only one factor is required and is
easily available in any particular situation. This approach implies that if an ou t-of-tolerance
value is observed, one of the things that the investigating physicist does first is check that
the particular treatment parameters used for that patient are within a tolerable range of the
factors used to produce the generic factor. In no case so far has the use of generic factors,
coupled with build -up caps, given rise to a problem.
Full correction factors are still used in any audit studies, critical group studies and new
equipment or new technique studies.
The application of generic correction factors is also in use in Amsterdam [Meijer 2001]. The
time required for analyzing the patient measurements is hereby substantially reduced, while
keeping the accuracy within acceptable limits. For prostate treatments, the additional
uncertainty for the target absorbed dose as a consequence of the interpatient varience of
the diode correction factors is estimated to be 0.2 % (1 SD). A similar, though more
radically simplifying approach is used by Alecu et al. [Alecu 1998]. They eliminate the
necessity of measuring seperate diode correction factors by using a second calibration
factor, having as “reference conditions” the average conditions of specific routine
treatment situations that deviate the most from the usual reference calibration conditions.
5.3.5.4 DATA COMMUNICATION AND RECORDING
One of the aims of the department in considering routine diode implementation was to
minimise the time necessary at the treatment unit and also to minimise the duplication of
effort. Therefore for the routine use of diodes fo r monitoring standard treatments, some
consideration was given to the calculation of expected measurement values and to how the
radiographers were required to record results.

129
Throughout the initial and follow-up studies, all measurements have been recorded
manually onto separate in vivo dosimetry sheets and then entered into a spreadsheet by
the research radiographer (or other research student involved in the project). The
calibration and correction factors are applied in the spreadsheet and the resulting dose
compared to the expected value, also calculated there from data input from the
prescription/treatment sheet and from planning data for the patient and for the treatment
machine.
For routine use, the cost-effective method adopted for calculating the exp ected result was
for physics staff, at the treatment planning stage, to produce an expected diode entrance
reading, taking the expected daily given dose and dividing this by the calibration factor for
the diode/treatment modality and by the generic correction factor for the diode, treatment
modality, treatment technique and field. This is easily done at the time of planning and MU
calculation when the given dose is being recorded. At the same time the ± 5 % tolerance is
applied to this value, so that a range of readings is written on the treatment sheet in an in
vivo dosimetry section. The treatment unit radiographers then simply have to check that
the measured reading is within this range and, at the simplest level, tick one box. If the
measurement is not within range, they must cross another box and place the sheet in a tray
for reference to the physics group for further investigation. In practice this process is
simple to operate. For example all breast patients on any particular treatment unit have the
same range of required diode readings, provided the dose and number of fractions is
standard. For our matched units from the same manufacturer, this same range applies for all
breast patients on both units, etc.
One consequence is that this does not record numerical data. However, if required for
analysis, this is obtainable either by requesting the radiographers to write down the
reading, as well as ticking one or other of the boxes, or by directly grabbing the readings
via the electrometer/PC interface. In general, we have not done either of these things for
routine data, although we may occasionally do so for audits. We intend to regularly
quantitatively assess the performance of the systems by limited patient number studies

130
repeating full entrance and exit measurements, as discussed above, and currently feel there
is no pressing need to analyse additional data.
5.3.5.5 DIODE MOUNTING AND HANDLING
In the initial studies, the diodes were connected via cables following the normal dosimetry
channel route from the tre atment room out to the control area. Following this in the early
routine implementation, permanent under-floor cables were installed to remove as much
cable from the floor area as possible and permanent junction boxes were installed on the
wall in the treatment room. Diode mounts on the couch and on the gantry were considered
and some prototype designs studied. Whilst the dedicated research radiographer, or other
research students, were involved in carrying out the measurements this was not a problem,
as they took care of the cabling, the position of the diode throughout patient setup and the
positioning of the diode. This was independent of what the treatment unit radiographers
were doing and practical and logistics problems were minimal. A number of instan ces of
connector damage were noted due to excess strain on the connectors from the hanging
cables, or due to damage when connectors were on the floor or were trapped between the
floor and the rotating patient support system. When the measurements were beco ming
routine and were being rolled out to the treatment unit radiographers, this system was not
acceptable. Instead a simple rotating mount was installed on the ceiling above the
treatment unit, directly above and approximately half-way along the horizontal arm of the
rotating gantry. From this an inverted L-shaped cable support was suspended, made from
light-weight cylindrical pipe, with the cable down the centre. The cable goes through the
centre of the rotating mount and above the false ceiling to a cable-way out of the room to
the control area where the electrometer is sited. At the other end it terminates in a
connector at the end of the pipe. The diode connects to this and rests on a quick-remove
hook at the base of the pipe. The swinging cable support is very easily swung completely
out of the way for patient setup and in towards the isocentre for diode positioning. The
system is shimmed to hold position at any point. The height of the lower edge of the cable -

131
supporting pipe was chosen taking into account the range of heights of our radiographers,
such that it is above the head of the tallest, to prevent accidents, but low enough for the
shortest to reach for swinging in or out! This system, designed in conjunction with the
research radiographer and the treatment unit radiographers has been very well accepted
and is very quick and simple in operation. Cable and connector problems have been
negligible since its installation. As new treatment units are installed in our current re -
equipping programme, similar systems are being installed in each treatment room.
5.3.5.6 DIODE QUALITY CONTROL
Significant simplification and time -saving can be achieved in diode quality control, by
ensuring quick checks are carried out fairly frequently, but requiring little time. These are
used as a warning system, so that major re -evaluations are only carried out when problems
are indicated at this level. This has been discussed above. In addition, a running check on
accumulated diode dose can also give an indication of when re -checks are likely to be
necessary.

132
5.4 LARGE SCALE IN VIVO DOSIMETRY IMPLEMENTATION – THE
COPENHAGEN EXPERIENC E
5.4.1 INTRODUCTION
In 1999 in vivo diode dosimetry was implemented in the Finsen Centre (FC) in Copenhagen,
Denmark. We started with a small group of FC patients, selected by virtue of their relatively
simple treatments. The initial purpose was to develop an effective and reliable quality
assurance procedure and subsequently to include treatments of greater complexity. This
has gradually been achieved. In the FC approximately 2250 patients are treated per year.
Seven linear accelerators (linacs) are available with energies ranging from 4 MV to 18 MV.
At this stage diode measurements are carried out on all linacs but there are still specific
types of treatment to be incorporated into the procedure. Our intention was to perform the
procedural measurements with every FC patient. In Denmark the legislation demands a
protocol where every patient treated should be undergoing in vivo dosimetry commencing
at the start of the treatment course. Taking this into consideration and the capacity of the
centre, our approach has been to utilise an in vivo dosimetry (IVD) system with a relatively
broad tolerance window aiming at detecting large deviations.
5.4.2 METHODOLOGY
The patient dose measurement is carried out in the beginning of the treatment course,
within the first three fractions in order to make it possible to correct any detected errors.
Expected diode values are derived from an independent spread sheet program containing a
database of correction factors and beam data (depth dose distributions). The program is
not integrated with the Record and Verify system (R&V), hence the prescribed dose and
beam parameters are manually entered into the spreadsheet. Clearly this procedure
increases the number of errors in the quality control (QC) process (errors in input data) but
constitutes an independent calculation of the expected entrance dose. However, in case of

133
computerised planning, the entrance dose at a point on the central axis c alculated with the
TPS is entered and relevant correction factors applied.
As asymmetric field technique (half- or three quarter of the field blocked) is standard
practice at the FC, the position of the diode during measurements has to be determined
during the IVD preparation. Therefore additional corrections of the expected diode reading
at the central axis are added in the spreadsheet to account for various focus -to-diode
distances and off-axis positions in wedged fields and treatment fields modulated wit h a
compensating filter. In a situation where the diode is positioned on immobilisation devices,
couch or bolus, the actual focus-to-diode distance is recorded during treatment, followed
by a correction of the expected diode reading.
5.4.3 EQUIPMENT
We sought a QC process with great simplicity and cost-benefit advantage. Therefore we
chose electrometers easy to handle and diodes with low sensitivity degradation with
accumulated dose, in order to reduce the need for repetitious calibration. Presently we use
the Apollo-5 electrometers and diodes P10 (4 MV), P20 (6-8 MV) and P30 (18 MV) (MDS
Nordion AB). In the tangential treatment technique, measurements are carried out with
cylindrically shaped diodes, Isorad-p diodes (Sun Nuclear Corporation), to minimise the
influence of diode directional dependence thus reducing the number of correction factors.
One treatment unit is equipped with QED diodes (Sun Nuclear Corporation). The use of
different types of diodes will allow us to evaluate statistical fluctuations due to various
diode characteristics.
5.4.4 CALIBRATION PROCEDURE
Currently, the calibration frequency is once every third month. Typically, the sensitivity
has decreased by less then 0.5 % during this period of time (corresponding to around
400Gy). The calibration is performed with a Solid Water
TM
phantom in conjunction with the
weekly constancy dosimetry check (ion chamber in plastic phantom) of the treatment unit.

134
Here, some aspects have to be considered regarding the type of errors one aims to detect.
The diode s ystem may be calibrated against:
1) an absolute dosimetry system
2) a constancy dosimetry check system
3) the monitor chamber of the linear accelerator
The ultimate choice of calibration method is to calibrate the IVD system to absorbed dose-
to-water using an ionisation chamber with a traceable calibration factor. Any malfunctions
of the treatment unit as well as human errors, such as an erroneous calibration of the
treatment unit, are then detected. However, this calibration procedure is onerous and time -
consuming. If the QC system is calibrated against a constancy check of the linac output
(accelerator weekly output check), the second suggested calibration method, a
malfunctioning of the treatment unit is most likely to be detected while an erroneous unit
calibration may be veiled. The third, commonly used method would probably not detect
deviations related to an erroneous calibration of the treatment unit. Furthermore, a
systematic error may be introduced if the diode QC system is calibrated against the mo nitor
chamber of the linac i.e. the diodes are adjusted to the level of that linac’s specific day’s
output. Eventhough modern linear accelerators have a high stability (constancy within
±
2
%) this may be of importance in studies where a high accuracy is required in the QC
process (when diode measurements are used to check dose delivery to the target volume).
However, the uncertainty in the diode dose determination is a combination of many
parameters and it is not likely that any day-to-day variations in linac performance in
individual patient measurements will be detected.
Considering the type of deviations that we aimed to detect, we believed that diode
calibration using a constancy dosimetry check system was most cost-effective.
The variation in diode re sponse with temperature was accounted for in the calibration
procedure by means of adding a temperature correction factor to the diode reading during

135
calibration. However, it was considered inappropriate to include the influence of
temperature dependence in the head & neck region where immobilisation devices are used
in most cases.
5.4.5 CORRECTION FACTORS
This section does not deal with diode characteristics or with the variation of different
correction factors, as they are presented and discussed in Chapter 1 and Sections 5.1 and
5.2. Correction factors were applied to account for field size dependence and variations in
response at different SSDs in the energy range of 8 – 18 MV. No wedge correction factor
was necessary as only dynamic wedges are used in the FC. However, a correction factor
accounting for the non-linear dose per pulse dependence of the n -type diodes was applied
in
4 MV treatment fields modulated with compensation filters
.
Temperature dependence was
accounted for in the calibration procedure. In tangential treatment fields the cylindrically
shaped diode has been adopted, consequently no correction of the directional dependence
was required.
In order to reduce the number of correction factors , each diode type (P10, P20) had one set
of correction factors per energy; i.e. the same factors were applied regardless of treatment
unit or the individual diode.
5.4.6 TOLERANCE LEVELS
Fairly broad tolerance levels were chosen during the initial phase of the implementation
with the intention that they would be gradually minimised with hindsight. Reasonable
levels were established from phantom measurements and selected patient measurements.
The tolerance levels, coinciding with action levels, were related to the complexity of the
treatment delivery according to Table 5.9, rather than the intention of the treatment
(radical/palliative).
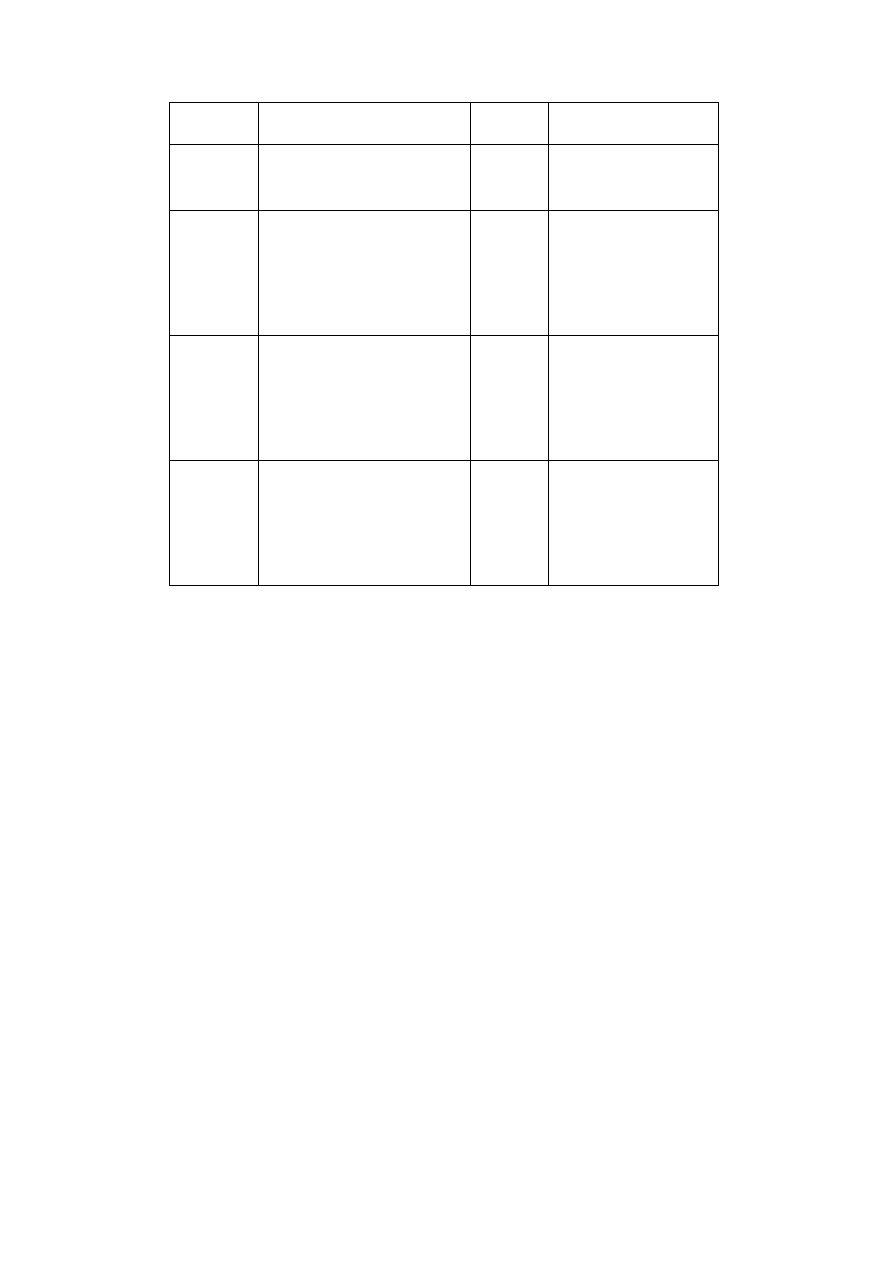
136
Treatment
site
Treatment technique
Tolerance
level
Diode type
Breast,
lumpectomy
Tangential field s, 6 - 8 MV
½ field blocked, dynamic wedge
±
8%
Isorad-p (Sun Nuclear)
Cylindrical build-up cap
Breast,
mastectomy
Anterior field, 6 - 18 MV
¾ field blocked
±
8%
P20, P30
(MDS Nordion AB)
QED 1115/1116
(Sun Nuclear)
Head &
Neck
Patient individual field t echnique
4 – 6 MV, ½ field blocked
compensating filter/dynamic
wedge
±
8%
P10, P20
(MDS Nordion AB)
QED 1115 (Sun Nuclear)
Chest/Pelvic Patient individual field technique
6 – 18 MV
±
5%
P20, P30
(MDS Nordion AB)
QED 1115/1116
(Sun Nuclear)
Table 5.9 Tolerance and action levels established for different treatment sites and the
diode type used.
5.4.7 RESULTS AND DISCUSSION
Since the start in 1999, over 3000 treatment fields have been monitored by means of diode
measurements of entrance dose. Figure 5.16, Figure 5.17 and Figure 5.18 shows of a major
part of all measurements as a percentage deviations from expected values, grouped in bins
of 1 %.
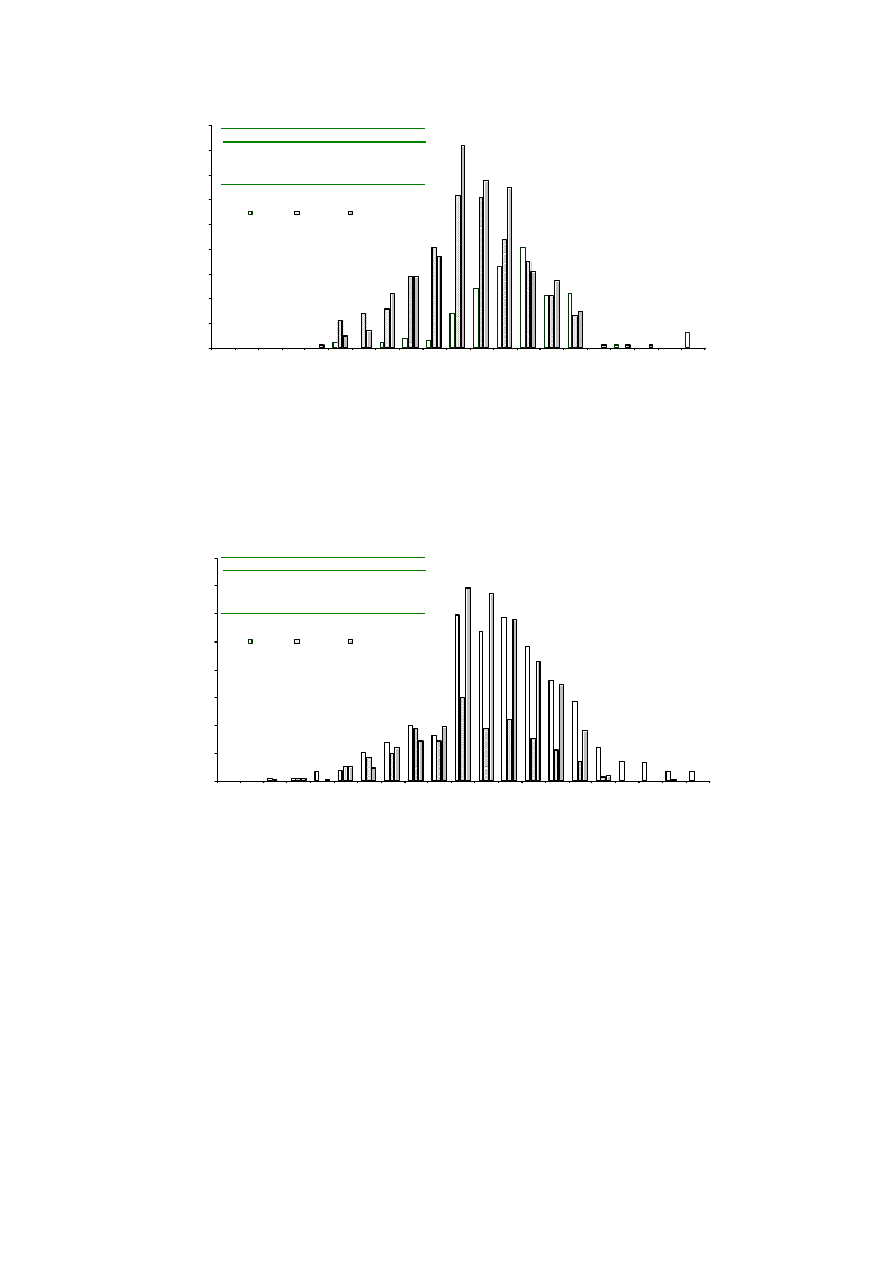
137
Figure 5.16 Deviations from expected value of diode measurements in manually planned
treatments. Breast treatments excluded.
Figure 5.17 Deviations from expected value of diode measurements in computer planned
treatments. Breast treatments excluded.
0
10
20
30
40
50
60
70
80
90
<-9.5
-9
-8
-7
-6
-5
-
4
-3
-2
-1
0
1
2
3
4
5
6
7
8
9
> 9.5
Number of fields
% Deviation from expected value
4 MV
6 – 8 MV
18 MV
4 MV
6 - 8 MV
18 MV
Average
2.64
0.43
0.67
1 SD
2.9
2.3
2.2
Number
173
347
392
0
20
40
60
80
100
120
140
160
% Deviation from expected value
Number of fields
4 MV
6 – 8 MV
18 MV
4 MV
6 - 8 MV
18 MV
Average
1.64
0.31
1.2
1 SD
3.0
2.7
2.2
Number
776
329
699
<-9.5
-9
-8
-7
-6
-5
-
4
-3
-2
-1
0
1
2
3
4
5
6
7
8
9
> 9.5
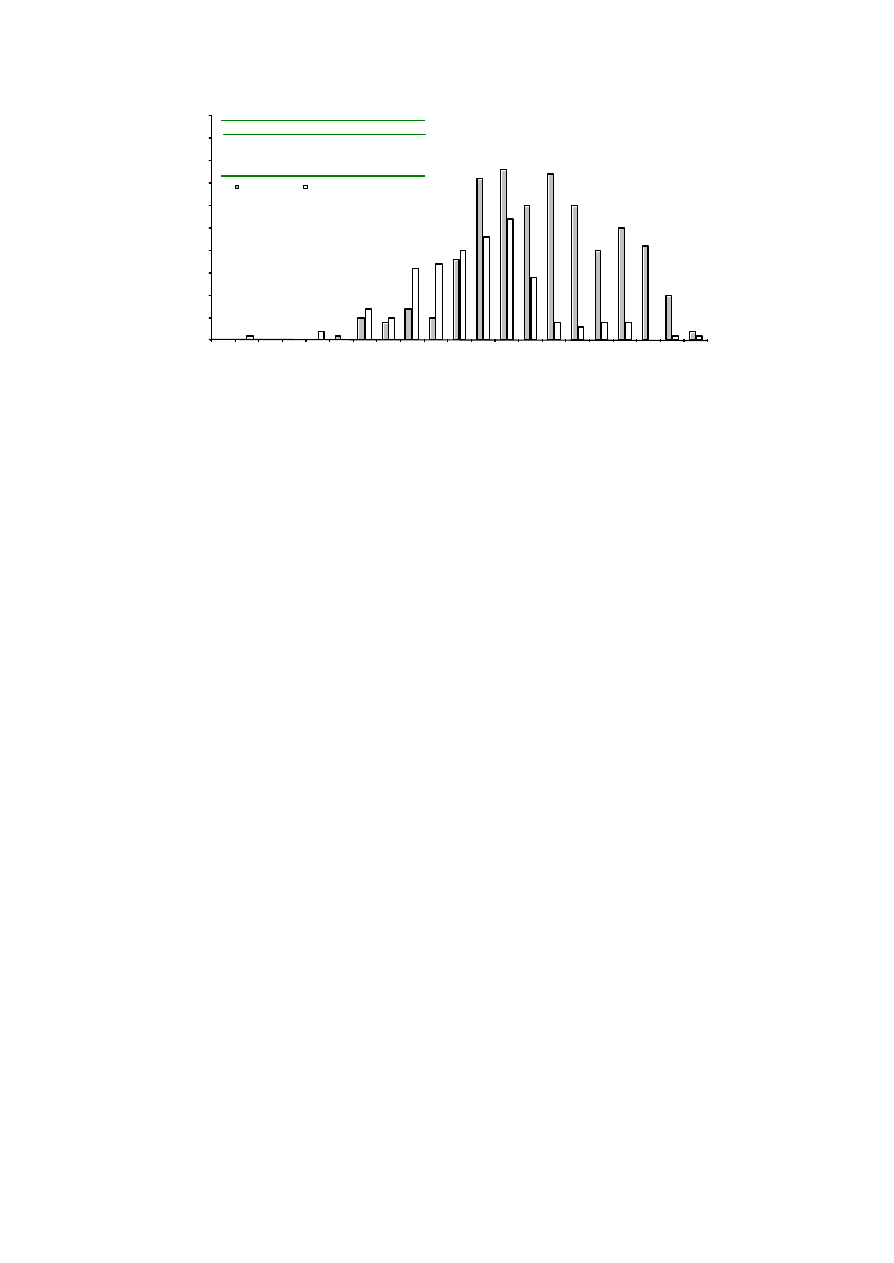
138
Figure 5.18 Deviations from expected value of diode measurements in breast treatments
(computer planned treatments).
The positioning of the diode becomes more critical in treatment fields incorporating
wedges or compensating filters, reducing the precision in the QC process. This can also be
seen as a larger deviation in the frequency distribution. In simple, manually planned
treatments the level of complexity is low (no wedges, compensation filters or field
asymmetry). Consequently, the variations from the expected value are smaller; i.e. for
energies 6 – 8 MV a standard deviation of 2.3 % (1 SD) was calculated and 2.2 % for 18 MV
(Figure 5.16). In more sophisticated, computer planned treatments (Figure 5.17) the
corresponding figures were slightly higher for 6 - 8 MV: 2.7 %. The largest spread was
recorded in the tangential treatment technique with a standard deviation of nearly 5 %.
This would, to some degree, be expected because of the higher level of complexity. The
measurements of mastectomy treatment patients showed a significant shift towards
positive variation suggesting a systematic error. The distribution had an average of 3.5 %
with a standard deviation of 3.1 %. An investigation of possible causes revealed errors in
0
5
10
15
20
25
30
35
40
45
50
Number of fields
Mastectomy
Lumpectomy
<-9.5
-9
-8
-7
-6
-5
-
4
-3
-2
-1
0
1
2
3
4
5
6
7
8
9
> 9.5
% Deviation from expected value
Mastectomy
Lumpectomy
Average
3.51
-1.03
1 SD
3.12
4.71
Number
289
149

139
the output factors used to calculate monitor units in quarter fields (¾ blocked fi eld) i.e. the
shift of the average was induced by systematic errors in the treatment process.
At the end of the year 2000, one of our 4 MV energy units had a breakdown and during the
subsequent absolute dose-to-water calibration the output was, by human error, adjusted
nearly 5% higher than intented. The diode system was not recalibrated at the same time
and consequently, the erroneous calibration was detected with patient diode
measurements. However, these measurements (a total of 27) on their own, do not explain
the shift in the mean average of the distribution in 4 MV energy treatment fields. The shift
shows an average of 1.6 % in computerised planned treatments and 2.6 % in manually
planned treatments. This deviation is believed to indicate a systematic error in the QC
process rather than the treatment process, considering the fact that the dosimetry accuracy
in this treatment technique has been carefully verified. The shift has to be further
investigated. One aspect may be reconsidered: the diode temperature dependence that is
not accounted for in 4 MV treatment fields. Further actions have to be taken to improve the
accuracy in the diode positioning in head, neck and breast treatments.
Besides the erroneous unit calibration and the systematic errors in the dose calculations
the diode QC process so far has detected two errors in the treatment process: 1) A
discrepancy in beam energy between calculation (manually planned) and treatment delivery
caused by an erroneous input in the R&V system. 2) For a patie nt with two target volumes,
the treatment fields were mixed up; caudal target volume was treated with cranial treatment
fields and vice versa.
5.4.8 CONCLUSION
The implementation of a new QC tool, such as diode measurements of entrance doses, is an
ongoing process that continuously needs evaluation and refinement. Our goal was to
implement diode measurements for every patient undergoing external radiotherapy in the
FC. To achieve an acceptable workload, a broad tolerance window was defined, accepting
relatively large deviations.

140
The uncertainty in the QC process is a combination of parameters in diode dosimetry
(calibration and correction factors) and the diode measurement (diode positioning). The
latter uncertainty is, according to our experience, of greater influence, especially when
treatment techniques of considerable complexity (modulated fields with field asymmetry)
are adopted, and should not be underestimated. The professional training of personnel and
clear guidelines on how to accurately perform measurements are the necessary precursors
for an accurate IVD system.
To measure every patient once is a major task but not unachievable. Our results show that
even an in vivo dosimetry system with wide tolerance values will provide a reliable QC
process, where human or systematic errors in dose calculations are likely to be detected.

141
5.5 RESULTS OF SYSTEMATIC IN VIVO ENTRANCE DOSIMETRY – THE
MILANO (HSR) EXPERIENCE
Systematic entrance dose in vivo dosimetry was gradually implemented at our Institute
from the end of ’94 in one of the three treatment rooms. It has recently been extended to
another treatment room (November 1999), and the extension to the third room is currently in
progress (Spring 2001).
In this review we present our experience during the period November ’94 – April 2000 on
more than 3900 measurements referring to 2001 patients.
5.5.1 MATERIALS AND METHODS
5.5.1.1 EQUIPMENT
The two treatment rooms where in vivo dosimetry was implemented are provided with a 6
MV linear accelerator (Linac 6/100); no record and verify systems are available at these
facilities.
For the entrance dose measurements we used p-type silicon diodes (Scanditronix EDP 10)
connected to a multi-channel electrometer (DPD 510, DPD 3 Scanditronix). The diodes are
monthly calibrated against an ionisation chamber in a reference geometry to convert the
diode signal in entrance absorbed dose. Procedures for the calibration are similar to those
reported in the ESTRO Booklet n° 1 [Van Dam 1994]. Cadplan (Varian-Dosetek Oy, versions
2.6.2, 2.7, 3.1) is our 3D treatment planning system (TPS); however, during the period
November ’94 - June ’95 we used (2D) older versions of Cadplan (2.5, 2.6.1).
5.5.1.2 IN VIVO MEASURED AND EXPECTED ENTRANCE DOSE
In vivo entrance dosimetry was generally performed at the first session of the therapy
(always within the first three or four days from the start of the treatment). After patient set -
up, just before the start of the irradiation, the diode was positioned at the centre of the
irradiation field, except in the case where the centre is shielded by blocks: in this case the

142
diode was positioned far from the penumbra region. Before fixing the diode, the source -to-
skin distance (SSD) was read and compared with the value defined during the simulator
session and used for treatment planning. In this way possible effects on the prescribed
dose due to small discrepancies between the two conditions (planning/therapy) could be
assessed during interpretation of the in vivo measurement.
Diode readings were not corrected by inverse square correction factors due to the choice
of monitoring the “true” accuracy of treatment delivery. Only if the focus-to-diode distance
was different from the SSD because of the use of immobilisation systems or other ancillary
equipment, the diode reading was corrected by an appropriate inverse square correction
factor.
The measured entrance dose was defined as the diode reading corrected by correction
factors. The influence on the diode signal of collimator opening, source-skin distance
(SSD), wedges, tray and obliquit y of the beam with respect to the diode axis was
previously investigated and appropriate correction factors were determined. The diode
signals were initially not corrected to take temperature into account. Only during the last
year we introduced a “clinical” correction factor for temperature. Due to the limited time
when diodes are in contact with the skin in clinical conditions (around 1 – 2 min.), based on
our measurements, it was estimated to be small (less than 0.5 % correction).
The expected entrance dose was calculated from the prescribed tumour dose by an
independent formula, based on tabulated TPR values and peak scatter factors for the
appropriate equivalent field sizes.
5.5.1.3 QA CHAIN: METHODS
A 5% action level was applied. However, in the case of opposed beams, a larger error was
accepted in one of the two beams (up to 7-8 %), if the average percentage deviation of the
two opposed fields was within the 5% limit. In this way, we took into account that small
SSD errors may compensate each other in terms o f isocentre dose. The 5% action level was
chosen on the basis of the expected accuracy and reproducibility of our measurement

143
system. This level roughly corresponds to 2 SD where SD is the global standard deviation
of the entrance dose measurement accuracy in most critical conditions (blocked and
wedged fields, tangential beams), excluding patient set-up inaccuracy. The global standard
deviation includes the accuracy and the reproducibility of the entrance dose measurements
with the ionisation chamber and with the diode system and the single SDs of the measured
correction factors.
If the discrepancy between the measured entrance dose and the expected one was below
the action level, in vivo dosimetry data (measured dose, expected dose and the percentage
deviation) was registered by a physicist with the appropriate of information for further
statistical analysis.
When the action level was exceeded, all treatment parameters were verified and the
measurement was generally repeated; a physicist directly performed all these phases (the
repetition of the in vivo dosimetry check may be performed by the technician, often with
the presence of a physicist). Firstly, the agreement between the treatment planning data
and the corresponding simulator data with the control of the data transfer on the treatment
chart was carefully checked. MU calculation/data transfer errors were expected to be rare
because a double check of the treatment chart data, of the treatment planning and of the
MU calculation was always done before tre atment delivery. Further checks concerned the
right use of wedges and blocks, including the presence of a block near the irradiation field
centre. If one of these checks was positive, the percentage deviation between the entrance
measured dose and the expected one could be explained. After correcting the mistake, a
second in vivo dosimetry check was performed to confirm the agreement between the
measured and the expected dose.
These checks were not always able to explain the deviation between the measured e ntrance
in vivo dose and the calculated one. Irrespective of this, a second check was always
performed. If a “large” deviation was detected even after the second check, we sometimes
measured the entrance dose on a solid phantom with diode and ionisation ch amber in the
same treatment conditions (i.e.: field width, wedge, blocks, SSDs…) and compared it with

144
the expected one. Because of the accumulated experience in assessing the causes of the
persistent deviations, the number of phantom controls decreased wit h time.
5.5.1.4 MU CALCULATION/DATA TRANSFER CHECK
From 1991 a double check procedure of MU calculation and data transfer/treatment chart
compilation has been implemented in our department. In previous reports we demonstrated
the ability of this simple tool in strongly reducing the occurrence of systematic errors
before treatment delivery. Every day a “controller” checks the MU and the dose
distribution calculation that has been performed by another operator, together with a check
of the irradiation data reported o n the treatment chart.
5.5.2 RESULTS
5.5.2.1 DETECTION OF SYSTEMATIC ERRORS
The in vivo dose measurements on 2001 patients revealed 14 systematic errors. 12 (0.6 %)
were serious (i.e.: leading to an under/over-dosage larger than 5 %) and 6 (0.3 %) were
larger than or equal to 10 %. In Table 5.10 the causes of all errors are reported. If excluding
“thickness” errors which cannot be detected by the MU calculation/data transfer check,
the rate of serious errors detected by in vivo dosimetry (which “really” escape the MU
calculation/data transfer check) was equal to 0.4 %. A number of minor errors due to an
uncorrected assessment of patient thickness were not considered; a number of random
errors (i.e. occurring for one fraction) we re also not considered.
In vivo dosimetry also permitted us to promptly detect a systematic error in measuring
patient thickness occurring during ‘97, due to a bad resetting of the “zero” indicator of the
simulator couch.

145
5.5.2.2 SYSTEMATIC ERRORS DETECTED BEFORE IN VIVO DOSIMETRY BY MU
CALCULATION/DATA TRA NSFER CHECK
In Table 5.10 the systematic errors detected before delivering the treatment by a check of
the treatment chart, of the treatment planning and of the MU calculation are reported. Data
refer to a longer period (‘91-‘99) and to patients treated in all treatment rooms. The rate of
serious errors was found to be equal to 1.53 % with a 0.77 % rate for errors larger than 10
%.
5.5.2.3 PATIENTS WITH MORE THAN ONE CHECK
Globally, 156/2001 (7.8 %) patients underwent more than one check; only 6/2001 had more
than 2 checks (see Table 5.11). The rate of second checks was higher for breast patients
(10.2 %) against non-breast patients (7.3 %, p = 0.06).
5.5.2.4 ACCURACY OF TREATMENT DELIVERY
In Table 5.12 the values of mean, median and SD of the distribution of the deviations
between measured and expected doses are reported together with the rate of deviations
larger than 5, 7 and 10 %. Globally, we had a mean deviation equal to 0.2 % with a SD equal
to 3.1 %. The rates of deviations larger than 5, 7 and 10 % resulted to be 10.3, 2.6 and 0.2 %
respectively. When averaging the deviations of opposed beams, the standard deviation
was 2.7 % and the rates of deviations larger than 5, 7 and 10 % reduced to 4.9, 0.8 and 0.0 %
respectively.
When considering the presence of a wedge, the rate of deviations larger than 5 and 7 %
was significantly higher than in the group without wedge (p < 0.0001). Similarly, the
presence of a block was related to a higher rate of deviations larger than 5 and 7 %
(respectively p < 0.03) and a systematic deviation from 0 (+ 1.5, p < 0.001).

146
When looking at the different anatomical sites, larger SD were found for breast fields;
smaller SD were found for vertebrae. Most of these results have been discussed elsewhere
[Fiorino 2000].
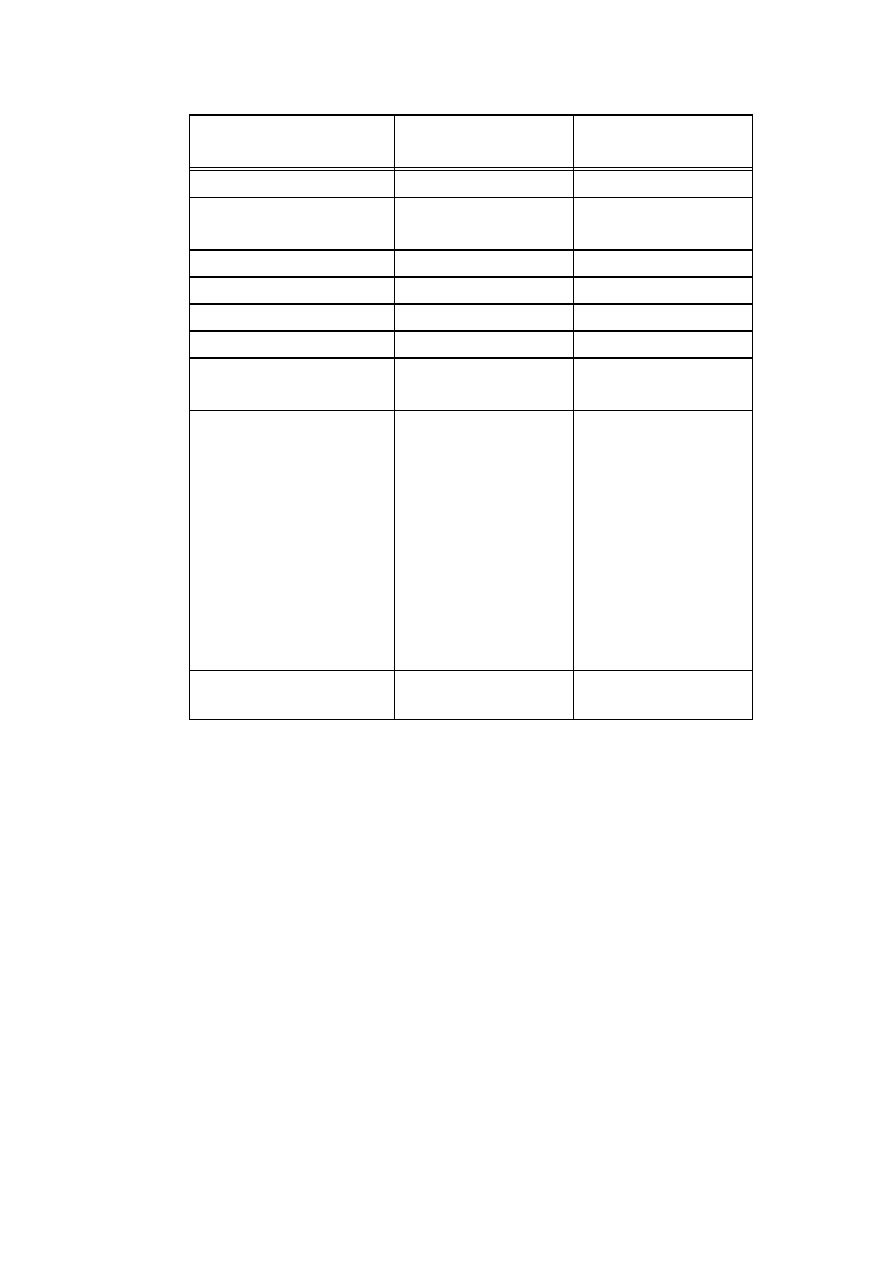
147
In vivo dosimetry
MU calculation and
data transfer check
Period
NOV. ‘94 – APRIL 2000
Sept. ’91 – May ‘99
Beams
Photons 6 MV
Photons 6, 18 MV
Electrons 6, 9, 12, 16 MeV
n° checks
3932
9747
n° patients
2001
7700*
Errors (including minor errors)°
14**
362
Errors > 5 %°
12
118
Error rate =
(n° errors > 5%)/n° patients
0.60 %
1.53 %
Type of errors (> 5 %) and rate:
Data
Energy
Blocks/Equivalent field
TPS (bad data entry)
Normalisation
Wedge
(all excluding thickness)
Thickness*** °
1 (0.05 %)
2 (0.10 %)
0
0
3 (0.15 %)
2 (0.10 %)
(8 (0.40 %))
4 (0.20 %)
42 (0.55 %)
14 (0.18 %)
8 (0.10 %)
3 (0.03 %)
41 (0.53 %)
10 (0.13 %)
Errors
≥
10 % (error rate)
6 (0.30 %)
59 (0.77 %)
* Estimated
** Minor errors due to uncorrect assessment of thickness were not considered
*** Large errors due to wrong assessment of thickness
° Excluding 5 large “thickness” errors due to bad resetting of simulator couch(see
text)
Table 5.10 The systematic errors detected by in vivo dosimetry are shown together
with those detected by MU calculation and data transfer check. Serious
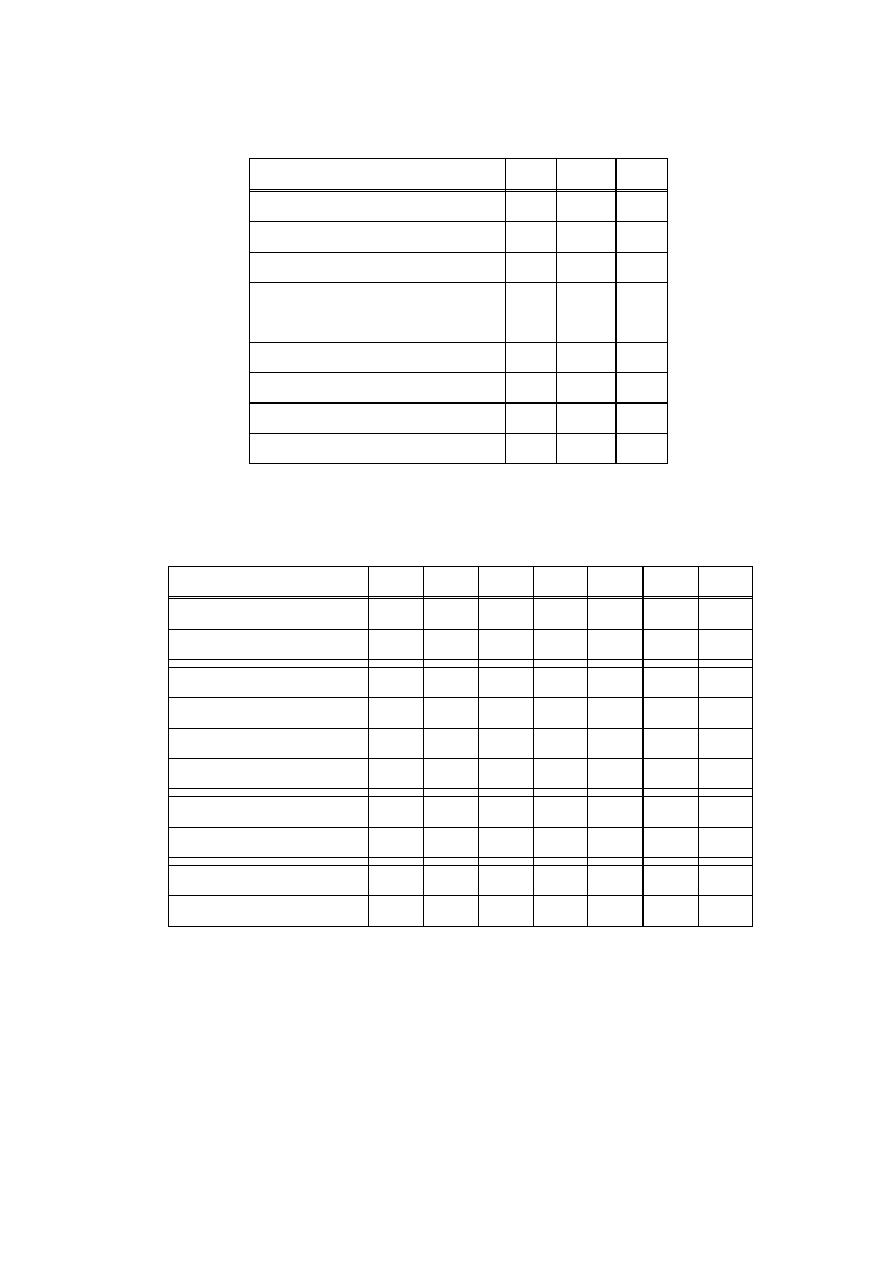
148
systematic errors were defined as those which, if undetected, could lead to a
5 % or more error on the delivered dose to the PTV.
N
N pts
%
Patients with more than one check
156
2001
7.8
Patients with more than two checks
6
2001
0.3
Breast
37
362
10.2
Mediastinum-abdomen – pelvis
(AP-PA fields)
46
640
7.3
Neck (lateral fields)
13
179
7.3
Arms -limbs
9
103
8.7
Brain
23
307
7.5
Others
23
410
5.6
Table 5.11 The rates of repetition of the in vivo dosimetry check.
Beams
N
MEAN Median
SD
%>5% %>7% %>10%
All
3770
0.2
0.2
3.1
10.3
2.6
0.2
All (averaging opposed beams)
2095
0.2
0.2
2.7
4.9
0.8
0.0
AP
1055
-0.2
-0.2
2.6
5.5
1.4
0.0
PA
958
1.0
0.8
3.2
12.7
3.3
0.2
Lateral
957
-0.2
-0.2
3.0
8.3
1.8
0.2
Oblique
799
0.4
0.7
3.5
15.6
4.5
0.4
Wedged
954
0.6
0.8
3.5
15.6
4.8
0.4
Unwedged
2816
0.1
0.0
2.9
8.3
1.9
0.1
Blocked
1259
1.5
1.5
3.0
11.8
3.5
0.4
Blocked & unwedged
1156
1.4
1.5
2.9
10.7
2.8
0.3
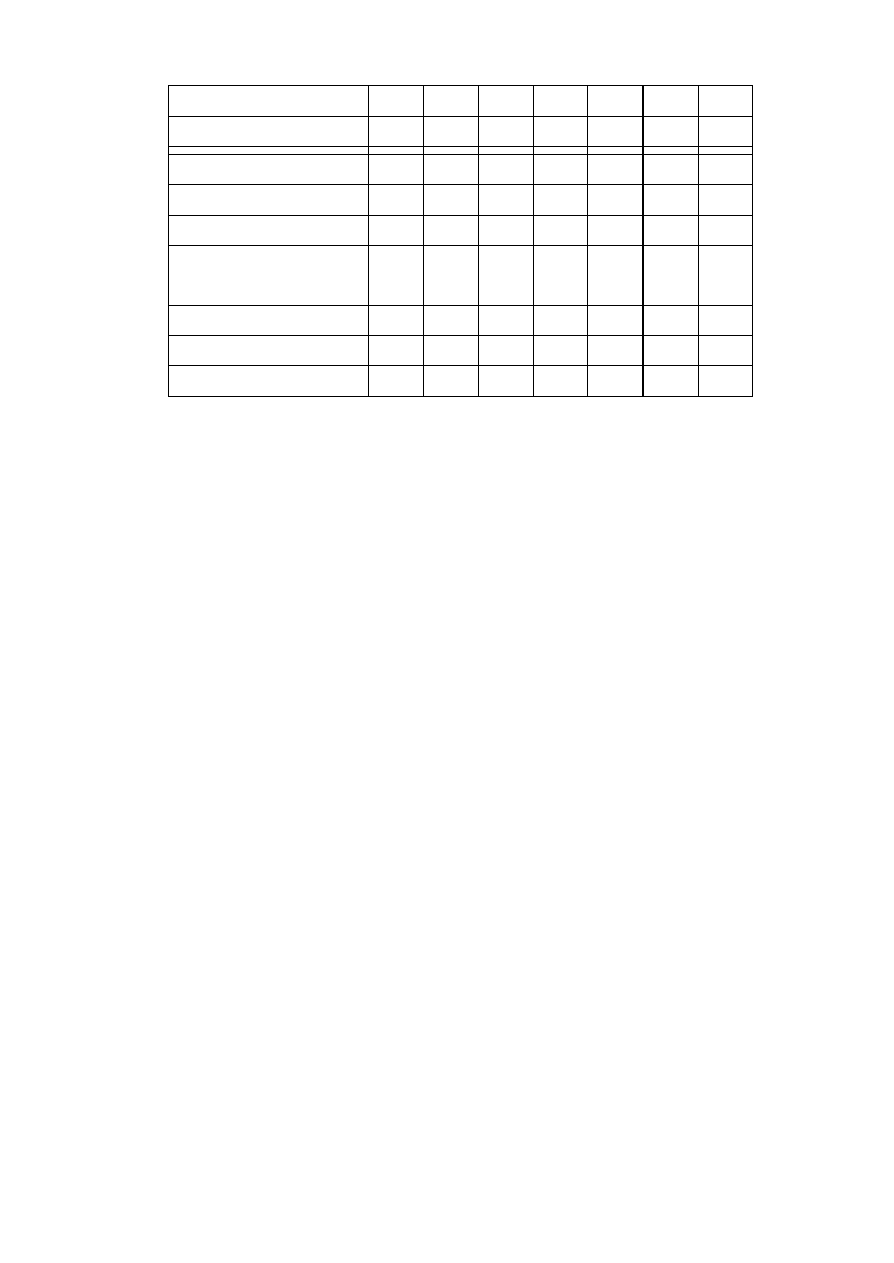
149
Unblocked
2511
-0.4
-0.5
3.0
9.4
2.2
0.1
Unblocked & unwedged
1660
-0.8
-0.9
2.6
6.7
1.3
0.0
Breast
719
0.3
0.5
3.5
15.7
3.9
0.3
Brain
593
-1.0
-1.2
2.8
8.4
1.3
0.0
Neck (lateral)
344
1.1
1.4
2.8
8.1
2.3
0.0
Neck (AP-PA) &
Supraclavicular
103
1.0
1.0
3.3
10.7
5.8
1.0
pelvis, abdomen, thorax AP/PA
1261
0.5
0.3
3.0
10.1
2.0
0.0
ARMS/LIMBS
160
0.1
-0.2
3.2
10.6
6.3
0.0
VERTEBRAE
280
0.1
0.3
2.1
1.0
0.5
0.0
Table 5.12 Deviations between measured and expected entrance dose: mean and median
deviations, SD, rates of deviations larger than 5, 7 and 10 % are presented in
a number of ways. If more than one check was performed, the data of the last
check were considered (n = 3932, 2001 patients).
5.5.3 FINAL REMARKS
Our experience in systematic in vivo dosimetry confirms that a number of serious
systematic errors might escape the independent check of dose calculation and data
transfer, which should be always performed before treatment delivery. Moreover, in vivo
dosimetry permits detection of a number of minor errors (SSDs and thickness errors) which
would be undetected by the independent check, thus improving the global quality of the
treatment. The high accuracy which can be reached by in vivo dosimetry with diodes, once
appropriate correction factors are applied, can also, by pooling patient data, detect
machine-related problems (for example, the discovered bad resetting of the simulator
couch), wrong configuration of treatment units on TPS and uncorrected procedures during
the chain which precedes treatment delivery, wh ich could lead to systematic errors in dose

150
delivery on a large number of patients. Another important goal of in vivo dosimetry is
maintaining a high level of attention on quality by all the involved staff. For this reason, in
our opinion, it is reasonable to suppose that without in vivo dosimetry, the rate of serious
systematic errors could be higher than the one reported by ourselves and in other similar
studies. In our opinion, any effort in implementing systematic in vivo dosimetry is justified.
However, it is mandatory to consider that clinical implementation of such programs implies,
above all, the allocation of human resources and a relevant organisational work. This is the
main cause of the limitation of systematic in vivo dosimetry to one of the three treatment
rooms of our institute until November 1999.
A very important element is the need of precise indications if the action level is exceeded.
Too high a number of second in vivo dosimetry checks may induce a negative impression
concerning the aim of the check and could generate distrust among personnel. Our results
indicate that the 5 % choice for the action level was appropriate. However, it could be
useful to set different action levels depending on the type of beam: in our case it will be
reasonable to set a 6-7 % action level for tangential wedged beams.

151
APPENDIX 1: LITERATURE OVERVIEW
[AAPM 1994]
AAPM
Comprehensive QA for radiation oncology
Report of AAPM Radiation Therapy Committee TG40.
Med. Phys. 21: 581-618 (1994)
[
Alecu 1997
]
R. Alecu, J.J. Feldmeier and M. Alecu
Dose perturbations due to in vivo dosimetry with diodes
Radiother. Oncol. 42: 289-291 (1997)
[
Alecu 1998
]
R. Alecu, M. Alecu, and T.G. Ochran
A method to improve the effectiveness of diode in vivo dosimetry
Med. Phys. 25: 746-749 (1998)
[Alecu 1999]
R. Alecu, T. Loomis, J. Alecu and T.G. Ochran
Guidelines on the implementation of diode in vivo dosimetry programs
for photon and electron external beam therapy
Med. Dosim. 24: 5-12 (1999)
[
Aletti 1991
]
P. Aletti, P. Bey, A. Noel, L. Malissard and C. Sobczyk
Programme d’assurance de qualité dans l’exécution de la radiothérapie
externe au Centre Alexis Vautrin
Bull. Cancer/Radiother. 78: 535-541 (1991)
[
Aletti 1994
]
P. Aletti
In vivo dosimetry: measurement strategy in vivo
Bull. Cancer/Radiother. 81: 453-455 (1994)
[
Altshuler 1989
]
C. Altshuler, M. Resbeut, D. Maraninchi, J.P. Guillet, D. Blaise, A.M.
Stoppa and Y. Carcasonne
Fractionated total body irradiation and allogeneic bone marrow
transplantation for standard risk leuke mia
Radiother. Oncol. 16: 289-295 (1989)

152
[
Aukett 1991
]
R.J. Aukett
A comparison of semiconductor and thermoluminescent dosemeters for
in vivo dosimetry
Br. J. of Radiol. 64: 947-952 (1991)
[Bagne 1977]
F. Bagne
A comprehensive study of LiF TL response to high energy photons and
electrons
Radiology 123: 753-760 (1977)
[Bartolotta 1995] A. Bartolotta, M. Brai, V. Caputo, R. Di Liberto, D. Di Mariano, G.
Ferrara, P. Puccio and A. Sansone Santamaria
The response behaviour of LiF:Mg, Cu, P thermoluminescence
dosimeters to high-energy electron beams used in radiotherapy
Phys. Med. Biol. 40: 211-220 (1995)
[Bascuas 1977]
J.L. Bascuas, J. Chavaudra, G. Vauthier and J. Dutreix
Intérêt des mesures "in vivo" systématiques en radiothérapie
J. Radiol. Electrol. 58: 701-708 (1977)
[Beddar 1992a]
A.S. Beddar, T.R. Mackie and F.H. Attix
Water-equivalent plastic scintillation detectors for high-energy beam
dosimetry: I. Physical characteristics and theoretical considerations
Phys. Med. Biol. 37: 1883-1900 (1992)
[Beddar 1992b]
A.S. Beddar, T.R. Mackie and F.H. Attix
Water-equivalent plastic scintillation detectors for high-energy beam
dosimetry: II. Properties and measurements
Phys. Med. Biol. 37: 1901-1913 (1992)
[Biggs 1979]
P.J. Biggs and C.C. Ling
Electrons as the cause of the observed dmax shift with field size in high-
energy photon beams
Med. Phys. 6: 291-295 (1979)

153
[Bjärngard 1993] B.E. Bjärngard, P. Vadash and T. Zhu
Doses near the surface in high energy x-ray beams
Med. Phys. 22: 465-468 (1995)
[Blake 1990]
S.W. Blake, D.E. Bonnett, and J. Finch
A comparison of two methods of in vivo dosimetry for a high energy
neutron beam
Br. J. of Radiol. 63: 476-481 (1990)
[Blanco 1987]
S. Blanco, M.A. Lopez-Bote and M. Desco
Quality Assurance in radiation therapy: systematic evaluation of errors
during the treatment execution
Radiother. Oncol. 8: 256 – 261 (1987)
[Blyth 1997]
Blyth, A.S. Macleod and D.I. Thwaites
A pilot study of the use of in vivo dosimetry for quality assurance in
radiotherapy
Radiography 3: 131-142 (1997)
[Blyth 2001a]
C. Blyth, M. Paolucci, C. Stacey and D.I. Thwaites
Patient and phantom measurements using diodes with and without
buildup caps for dosimetry verification in breast radiotherapy treatment
submitted to Radioth. Oncol.
[Blyth 2001b]
C. Blyth and D.I. Thwaites
Practical cost-effective implementation of routine diode dosimetry for
quality assurance in radiotherapy
submitted to J. Radioth. in Practice
[Boellaard 1998] R. Boellaard
In vivo dosimetry with a liquid -filled electronic portal imaging device
PhD. Thesis, Vrije Universiteit Amsterdam (1998)

154
[Bolla 1995]
M. Bolla, H. Bartelink, G. Garavaglia, D. Gonzalez, J.C. Horiot, K.A.
Johansson, G. van Tienhoven, K. Vantongelen and M. van Glabbeke
EORTC guidelines for writing protocols for clinical trials of radiotherapy
Radiother. Oncol. 36: 1-8 (1995)
[Briot 1990]
E. Briot, A. Dutreix and A. Bridier
Dosimetry for total body irradiation
Radiother. Oncol. Suppl. 1: 16-29 (1990)
[Broerse 1987]
J.J. Broerse and A.E. Varekamp
Total body irradiation for treatment of haematological diseases
Radiother. Oncol. 9: 87-90 (1987)
[Brown 1996]
L. Brown
Development of a diode-based in vivo dosimetry system for clinical use
in radiotherapy
M.Sc. thesis, University of Glasgow (1996)
[
Calandrino 1993
]
R. Calandrino, G.M. Cattaneo, A. Del Vecchio, C. Fiorino, B. Longobardi
and P. Signorotto
Human errors in the calculation of monitor units in clinical radiotherapy
practice
Radiother. Oncol. 28: 86-88 (1993)
[Calandrino 1997] R. Calandrino, G.M. Cattaneo, C. Fiorino, B. Longobardi, P. Mangili and
P. Signorotto
Detection of systematic errors in external radiotherapy before treament
delivery
Radiother. Oncol. 45: 272-274 (1997)
[Carruthers 1999] L. Carruthers, A.T. Redpath and I. Kunkler
The use of compensators to optimise the three dimensional dose
distribution in radiotherapy of intact breast
155
Radioth. Oncol. 50: 291-300 (1999)
[Chavaudra 1976] J. Chavaudra, G. Marinello, A.M. Brulé and J. Nguyen
Utilisation pratique du borate de lithium en dosimétrie par
thermoluminescence
J. Radiol. Electrol. 57: 435-445 (1976)
[Ciocca 1991]
M. Ciocca, L. Landoni, C. Italia, P. Montanaro, P. Canesi and R. Valdagni
Quality control in the conservative treatment of breast cancer: patient
dosimetry using silicon detectors
Radiother. Oncol. 22: 304-307 (1991)
[Contento 1984] G. Contento, M.R. Malisan and R. Padovani
Response of thermoluminescence dosemeters to beta radiation and skin
dose assessment
Phys. Med. Biol. 29: 661-678 (1984)
[Cozzi 1998]
L. Cozzi and A. Fogliata-Cozzi
Quality assurance in radiation oncology. A study of feasibility and
impact on action levels of an in vivo dosimetry program during breast
cancer irradiation
Radiother. Oncol. 47: 29-36 (1998)
[Cross 1992]
P. Cross, D.J. Joseph, J. Cant, S.G. Cooper and J.W. Denham
Tangential breast irradiation: simple improvements
Int. J. Radiation Oncology Biol. Phys. 23: 433-442 (1992)
[Cunningham 1984] J.R. Cunningham
Quality assurance in dosimetry and treatment planning
Int. J. Radiation Oncology Biol. Phys. 10, Suppl.1: 105-109 (1984)
[Davis 1997]
J.B. Davis, A. Pfafflin and A. Fogliata-Cozzi
Accuracy of two - and three-dimensional photon dose calculation for
tangential breast irradiation of the breast

156
Radiother. Oncol. 42: 245-248 (1997)
[Dawes 1988]
P.J.D.K. Dawes, E.G. Aird and I.P. Crawshaw
Direct measurement of dose at depth in breast cancer using lithium
fluoride
Clinical Radiology 39: 301-304 (1988)
[de Boer 1993]
S.F. de Boer, A.S. Beddar and J.A. Rawlinson
Optical filtering and spectral measurements of radiation-induced light in
plastic scintillation dosimetry
Phys. Med. Biol. 38: 945-958 (1993)
[Ding 1995a]
W. Ding, J.E. Verstraete and J.M. Van Dam
Performance of new Scanditronix diodes for in vivo dosimetry
Acta-Oncol. 34: 268-270 (1995)
[Ding 1995b]
W. Ding, W. Patterson, L. Tremethick, D. Joseph
Calibration of entrance dose measurement for an in vivo dosimetry
programme
Australas Radiol. 39: 369-374 (1995)
[Dische 1993]
S. Dische, M.I. Saunders, C. Williams, A. Hopkins and E. Aird
Precision in reporting the dose given in a course of radiotherapy
Radiother. Oncol. 29: 287-293 (1993)
[Dixon 1982]
R.L. Dixon and K.E. Ekstrand
Silicon diode dosimetry
Int. J. Appl. Radiat. Isot. 33: 1171-1176 (1982)
[Duggan 1997]
L. Duggan, T. Kron, S. Howlett, A. Skov and P. O’Brien
An independent check of treatment plan, prescription and dose
calculation as a QA procedure
Radiother. Oncol. 42: 297-301 (1997)

157
[Dutreix 1992]
A. Dutreix, G. Leunens, J. Van Dam and E. van der Schueren
Quality assurance in radiotherapy at the patient level
AMPI Medical Physics Bulletin 17: 22-25 (1992)
[Dutreix 1997]
A. Dutreix, B.E. Bjärngard, A. Bridier, B. Mijnheer, J.E. Shaw and H.
Svensson
Monitor unit calculation for high energy photon beams
ESTRO Booklet nr 3, Garant (1997)
[Edwards 1997]
C.R. Edwards, M.H. Grieveson, P.J. Mountford and P. Rolfe
A survey of current in vivo radiotherapy dosimetry practice
Br. J. of Radiol. 70: 299-302 (1997)
[Elliott 1999]
P.A. Elliott
In vivo diode dosimetry in pelvic radiotherapy treatments using 16 MV
photons
M.Sc. thesis, University of Edinburgh (1999)
[Elliott 2001]
P.A. Elliott, L. Brown and D.I. Thwaites
In vivo dosimetry of standard and conformal pelvic radiotherapy
treatments
submitted to Radioth. Oncol.
[Essers 1993]
M. Essers, J.H. Lanson and B.J. Mijnheer
In vivo dosimetry during conformal therapy of prostatic cancer
Radiother. Oncol. 29: 271-279 (1993)
[Essers 1994]
M. Essers, R. Keus, J.H. Lanson and B.J. Mijnheer
Dosimetric control of conformal treatment of parotid gland tumours
Radiother. Oncol. 32: 154-162 (1994)
[Essers 1995]
M. Essers, J.H. Lanson, G. Leunens, T. Schnabel and B.J. Mijnheer
The accuracy of CT -based inhomogeneity corrections and in vivo
dosimetry for the treatment of lung cancer
Radiother. Oncol. 37: 199-208 (1995)
158
[Essers 1996]
M. Essers
In vivo dosimetry in radiotherapy, development, use and evaluation of
accurate patient dose verification methods
Ph. D. Thesis, Amsterdam (1996)
[
Essers 1999
]
M. Essers, and B.J. Mijnheer
In vivo dosimetry during external photon beam radiotherapy
Int. J. Radiat. Oncol. Biol. Phys. 43: 245-259 (1999)
[Fiorino 1993]
C. Fiorino, A. del Vecchio, G.M. Cattaneo, M. Fusca, B. Longobardi, P.
Signorotto and R. Calandrino
Exit dose measurements by portal film dosimetry
Radiother. Oncol. 29: 336-340 (1993)
[Fiorino 2000]
C. Fiorino, D. Corletto, P. Mangili, S. Broggi, A. Bonini, G.M. Cattaneo,
R. Parisi, A. Rosso, P. Signorotto, E. Villa, R. Calandrino
Quality Assurance by systematic in vivo dosimetry: re sults on a large
cohort of patients
Radiother. Oncol. 56: 85-95 (2000)
[Fontenla 1996a] D.P. Fontenla, J. Curran, R. Yaparpalvi and B. Vikram
Customization of a radiation management system to support in vivo
patient dosimetry using diodes
Med. Phys. 23: 1425-1429 (1996)
[Fontenla 1996b] D.P. Fontenla, R. Yaparpalvi, C.S. Chui and E. Briot
The use of diode dosimetry in quality improvement of patient care in
radiotherapy
Med. Dosim. 21: 235-241 (1996)
[Gagnon 1979]
W.F. Gagnon and J.L. Horton
Physical factors affecting absorbed dose to the skin from cobalt -60
gamma rays and 25-MV x rays
Med. Phys. 6: 285-290 (1979)

159
[Gandola 1990a] L. Gandola, S. Siena, M. Bregni, E. Sverzellati, P. Piotti, C. Stucchi, A.
Massimo Gianni and F. Lombardi
Prospective evaluation of pulmonary function in cancer patients treated
with total body irradiation, high-dose mephalan, and autologous
hematopoietic stem cell transplantation
Int. J. Radiation Oncology Biol. Phys. 19: 743-749 (1990)
[Gandola 1990b] L. Gandola, F. Lombardi, S. Siena, M. Bregni, P. Piotti, E. Sverzellati, C.
Stucchi, G. Bonadonna, A.M. Gianni and A. Lattuada
Total body irradiation and high-dose melpahalan with bone marrow
transplantation at Istituto Nazionale Tumori Milan, Italy
Radiother. Oncol. Su ppl. 1: 105-109 (1990)
[Garavaglia 1993] G. Garavaglia, K.-A. Johansson, G. Leunens and B.J. Mijnheer
The role of in vivo dosimetry
Radiother. Oncol. 29: 281-282 (1993)
[Georg 1997]
D. Georg, E. Briot, F. Julia, D. Huyskens, U. Wolff and A. Dutreix
Dosimetric comparison of an integrated multileaf collimator vs. a
conventional collimator
Phys. Med. Biol. 42: 2285-2303 (1997)
[Georg 1999]
D. Georg, B. De Ost, M.-T. Hoornaert, P. Pilette, J. Van Dam, M. Van
Dycke and D. Huyskens
Build-up modification of commercial diodes for entrance dose
measurements in ‘higher energy’ photon beams
Radiother. Oncol. 51: 249-256 (1999)
160
[Graham 1981]
W.J. Graham, D.W. Anderson, D.J. Landry and C.R. Bogardus, Jr.
Accuracy of delivered dose in pelvic irradiation
Int. J. Radiation Oncology Biol. Phys. 7: 1117-1119 (1981)

161
[
Grusell 1984
]
E. Grusell and G. Rikner
Radiation damage induced dose rate nonlinearity in a n-type silicon
detector
Acta Radiol. Oncol. 23: 465-469 (1984)
[Grusell 1986]
E. Grusell and G. Rikner
Evaluation of temperature effects in p -type silicon detectors
Phys. Med. Biol. 31: 527-534 (1986)
[Grusell 1993]
E. Grusell and G. Rikner
Linearity with dose rate of low resistivity p-type silicon semiconductor
detectors
Phys. Med. Biol. 38: 785-792 (1993)
[Hamers 1991]
H.P. Hamers, K.-A. Johansson, J.L.M. Venselaar, P. De Brouwer, U.
Hansson and C. Moudi
Entrance and exit TL-dosimetry in the conservative treatment of breast
cancer: a pilot study for the EORTC-Radiotherapy Cooperative Group"
Radiother. Oncol. 22: 280-284 (1991)
[Hamers 1993]
H.P. Hamers, K.-A. Johansson, J.L.M. Venselaar, P. De Brouwer, U.
Hansson and C. Moudi
In vivo dosimetry with TLD in conservative treatment of breast cancer
patients treated with the EORTC protocol 22881
Acta Oncologica 32: 435-443 (1993)
[Hansson 1993]
U. Hansson, K.-A. Johansson, J.C. Horiot and J. Bernier
Mailed TL dosimetry programme for machine output check and clinical
application in the EORTC radiotherapy group
Radiother. Oncol. 29: 85-90 (1993)
[Hazuka 1993]
M.B. Hazuka, D.N. Stroud, J. Adams, G.S. Ibbott, and J.J. Kinzie
Prostatic thermoluminescent dosimeter analysis in a patient treated with
18 MV X rays through a prosthetic hip

162
Int. J. Radiation Oncology Biol. Phys. 25: 339-343 (1993)
[Heukelom 1991a] S. Heukelom, J.H. Lanson, G. van Tienhoven and B.J. Mijnheer
In vivo dosimetry during tangential breast treatment
Radiother. Oncol. 22: 269-279 (1991)
[Heukelom 1991b] S. Heukelom, J.H. Lanson and B.J. Mijnheer
Comparison of entrance and exit dose measurements using ionization
chambers and silicon diodes
Phys. Med. Biol. 36: 47-59 (1991)
[Heukelom 1992] S. Heukelom, J.H. Lanson and B.J. Mijnheer
In vivo dosimetry during pelvic treatment
Radiother. Oncol. 25: 111-120 (1992)
[Heukelom 1994] S. Heukelom, J.H. Lanson and B.J. Mijnheer
Quality assurance of the simultaneous boost technique for prostatic
cancer: dosimetric aspects
Radiother. Oncol. 30: 74-82 (1994)
[Holt 1975]
J.G. Holt, G.R. Edelstein and T. E. Clark
Energy dependence of the response of lithium fluoride TLD rods in high
energy electron fields
Phys. Med. Biol. 20: 559-570 (1975)
[Hoogenhout 1990] J. Hoogenhout, W.F.M. Brouwer, J.J.M. van Gasteren, A.
Schattenberg, T. de Witte, W.A.J. van Daal and C.A.M. Haanen
Clinical and physical aspects of total body irradiation for bone marrow
transplantation in Nijmegen
Radiother. Oncol. Suppl. 1: 118-120 (1990)
[Horiot 1993]
J.C. Horiot, J. Bernier, K.-A. Johansson, E. van der Schueren and H.
Bartelink
Minimum requirements for quality assurance in radiotherapy
Radiother. Oncol. 29: 103-104 (1993)

163
[Howlett 1996]
S.J. Howlett and T. Kron
Evaluation of p-type semiconductor diodes for in vivo dosimetry in a 6
MV X-ray beam
Australas Phys. Eng. Sci. Med. 19: 83-93 (1996)
[Howlett 1999]
S. Howlett, L. Duggan, S. Bazley, and T. Kron
Selective in vivo dosimetry in radiotherapy using p -type semiconductor
diodes: a reliable quality assurance procedure.
Med. Dosim. 24: 53-56 (1999)
[Hughes 1995]
D.B. Hughes, A.R. Smith, R. Hoppe, J.B. Owen, A. Hanlon, M. Wallace
and G.E. Hanks
Treatment planning for Hodgkin's disease: a patterns of care study
Int. J. Radiation Oncology Biol. Phys. 33: 519-524 (1995)
[Hussein 1995]
S. Hussein and E. El-Khatib
Total body irradiation with a sweeping 60cobalt beam
Int. J. Radiation Oncology Biol. Phys. 33: 493-497 (1995)
[Huyskens 1994] D. Huyskens, J. Van Dam and A. Dutreix
Midplane dose determination using in vivo measurements in
combination with portal imaging
Phys. Med. Biol. 39: 1089-1101 (1994)
[
ICRU 1976
]
ICRU
Determination of absorbed dose in patients irradiated by beams of X and
gamma rays in radiotherapy procedures
Report 24. ICRU, Bethesda, Maryland (1976)
[Indovina 1989]
P.L. Indovina, M. Benassi, G.C. Giacco, A. Primavera and A. Rosati
In vivo ESR dosimetry in total body irradiation
Strahlenther. Onkol. 165: 611-616 (1989)

164
[Jornet 1996]
N. Jornet, M. Ribas and T. Eudaldo
Calibration of semiconductor detectors for dose assessment in total
body irradiation
Radiother. Oncol. 38: 247-251 (1996)
[Jornet 2000]
N. Jornet, M. Ribas and T. Eudaldo
In vivo dosimetry: intercomparison between p-type based and n-type
based diodes for 16 to 25 MV energy range
Med. Phys. 27: 1287-1293 (2000)
[Kartha 1973]
P.K.I. Kartha, A. Chung Bin and F.R. Hendrickson
Accuracy in clinical dosimetry
Br. J. Radiol. 46: 1083 (1973)
[Kesteloot 1993a] K. Kesteloot, A. Dutreix and E. van der Schueren
A model for calculating the costs of in vivo dosimetry and portal
imaging in radiotherapy departments
Radiother. Oncol. 28: 108-117 (1993)
[Kesteloot 1993b] K. Kesteloot, A. Dutreix and E. van der Schueren
Quality assurance procedures in radiotherapy - Economic criteria to
support decision making
International Journal of Technology Assessment in Health Care 9: 274-
285 (1993)
[Kidane 1992]
G. Kidane
Evaluation of radiation diodes for in vivo dosimetry during radiotherapy
M.Sc. thesis, University of St Andrews (1992)
[Kirby 1992]
T.H. Kirby, W.F. Hanson and D.A. Johnston

165
Uncertainty analysis of absorbed dose calculations from
thermoluminescence dosimeters
Med. Phys. 19: 1427-1433 (1992)
[Klevenhagen 1978] S.C. Klevenhagen
Behaviour of p-n junction silicon radiation detectors in a temperature -
compensated direct-current circuit
Med. Phys. 5: 52-57 (1978)
[Knöös 1986]
T. Knöös, L. Ahlgren and M. Nilsson
Comparison of measured and calculated absorbed doses from tangential
irradiation of the breast
Radiother. Oncol. 7: 81-88 (1986)
[Kron 1993a]
T. Kron, A. Elliot, T. Wong, G. Showell, B. Clubb and P. Metcalfe
X-ray surface dose measurements using TLD extrapolation
Med. Phys. 20: 703-711 (1993)
[Kron 1993b]
T. Kron, M. Schneider, A. Murray and H. Mameghan
Clinical thermoluminescence dosimetry: how do expectations and results
compare?
Radiother. Oncol. 26: 151-161 (1993)
[Kubo 1985]
H. Kubo
Dosimetry of anterior chest treatment by 10 MV x-rays using a tissue
compensating filter
Radiother. Oncol. 4: 185-192 (1985)
[Kutcher 1994]
G.J. Kutcher, L. Coia, M. Gillin, W.F. Hanson, S. Leibel, R.J. Morton, J.R.
Palta, J.A. Purdy, L.E. Reinstein, G.K. Svensson, M. Weller and L.
Wingfield

166
Comprehensive QA for radiation oncology: report of AAPM Radiation
Therapy Committee Task Group 40
Med. Phys. 21: 581-618 (1994)
[Lagrange 1988] J.-L. Lagrange, S. Marcié, A. Costa, M. Héry, O. Saint-Martin and N.
Brassart
Contribution à l'optimisation des mesures in vivo par detecteurs semi -
conducteurs
in "Dosimetry in Radiotherapy". IAEA Publication (IAEA -SM-298/24,
Vienna) Vol. 2: 259-273 (1988)
[Lagrange 1994] J.-L. Lagrange and A. Noel
The role of in vivo dosimetry in radiotherapy
Bull.-Cancer-Radiotherapy 81: 456-462 (1994)
[Lambert 1983]
G.D. Lambert, W.E. Liversage, A.M. Hirst and D. Doughty
Exit dose studies in megavoltage photon therapy
Br. J. of Radiol. 56: 329-334 (1983)
[
Lanson 1999
]
J.H. Lanson, M. Essers, G.J. Meijer, A.W.H. Minken, G.J. Uiterwaal and
B.J. Mijnheer
In vivo dosimetry during conformal radiotherapy
Radiother. Oncol. 52: 51-59 (1999)
[Lathinen 1988]
T. Lahtinen, H. Puurunen, P. Simonen, A. Pekkarinen and A. Väänänen
In vivo dose measurements with new linear accelerators
in "Dosimetry in Radiotherapy", 259-277, International Atomic Energy
Agency (1988)
[
Lax 1991
]
I. Lax

167
Dosimetry of
106
Ru eye applicators with a p -type silicon detector.
Phys. Med. Biol. 36: 963-972 (1991)
[Lee 1994]
P.C. Lee, J.M. Sawicka and G.P. Glasgow
Patient dosimetry quality assurance program with a commercial diode
system
Int. J. Radiation Oncology Biol. Phys. 29: 1175-1182 (1994)
[Leunens 1990a] G. Leunens, J. Van Dam, A. Dutreix and E. van der Schueren
Quality assurance in radiotherapy by in vivo dosimetry. 1. Entrance
dose measurements, a reliable procedure
Radiother. Oncol. 17: 141-151 (1990)
[Leunens 1990b] G. Leunens, J. Van Dam, A. Dutreix and E. van der Schueren
Quality assurance in radiotherapy by in vivo dosimetry. 2. Determination
of the target absorbed dose
Radiother. Oncol. 19: 73-87 (1990)
[Leunens 1991]
G. Leunens, J. Verstraete, J. Van Dam, A. Dutreix and E. van der
Schueren
In vivo dosimetry for tangential breast irradiation: role of the equipment
in the accuracy of dose delivery
Radiother. Oncol. 22: 285-289 (1991)
[Leunens 1992a] G. Leunens, J. Verstraete, W. Van Den Bogaert, J. Van Dam, A. Dutreix
and E. van der Schueren
Human errors in data transfer during the preparation and delivery of
radiation treatment affecting the final result. "Garbage in, garbage out".
Radiother. Oncol. 23: 217-222 (1992)
[Leunens 1992b] G. Leunens, J. Verstraete, A. Dutreix and E. van der Schueren

168
Assessment of dose inhomogeneity at target level by in vivo dosimetry:
can the recommended 5% accuracy in the dose delivered to the target
volume be fulfilled in daily practice?
Radiother. Oncol. 25: 242-250 (1992)
[Leunens 1993]
G. Leunens, J. Van Dam, A. Dutreix and E. van der Schueren
Importance of in vivo dosimetry as part of a quality assurance program
in tangential breast treatments
Int. J. Radiation Oncology Biol. Phys. 28: 285-296 (1993)
[Leunens 1994]
G. Leunens, J. Verstraete, J. Van Dam, A. Dutreix and E. van der
Schueren
Experience in in-vivo dosimetry investigations in Leuven
in "Radiation dose in radiotherapy from prescription to delivery" IAEA
Report TECDOC-734, 283-289 (1994)
[Li 1995]
C. Li, L.S. Lamel and D. Tom
A patient dose verification program using diode detectors
Med. Dosim. 20: 209-214 (1995)
[Loncol 1996]
Th. Loncol, J.L. Greffe, S. Vynckier and P. Scalliet
Entrance and exit dose measurements with semiconductors and
thermoluminescent dosemeters: a comparison of methods and in vivo
results
Radiother. Oncol. 41: 179-187 (1996)
[Lööf 2001]
M. Lööf, H. Nyström and G. Rikner
Characterisation of commercial n - and p -type diodes for entrance dose in
vivo dosimetry in high energy beams
Submitted to Radiother. Oncol.

169
[
Luse 1996
]
R.W. Luse, J. Eema, T. Kwiatkowski and D. Schumacher
In vivo diode dosimetry for total marrow irradiation
Int. J. Radiat. Oncol. Biol. Phys. 36: 189-195 (1996)
[Mangili 1999]
P. Mangili, C. Fiorino, A. Rosso, G.M. Cattaneo, R. Parisi, E. Villa, R.
Calandrino
In vivo dosimetry by diode semiconductors in combination with portal
films during TBI: reporting a 5-years clinical experience
Radiother. Oncol. 52: 269-276, 1999
[Marinello 1977] G. Marinello, A. Buscaill and F. Baillet
Dégradation de l'énergie d'un faisceau fixe d'électrons de 7 MeV en vue
du traitement du mycosis fongoïde
J. Radiol. Electrol. 58: 693-699 (1977)
[Mayles 2000]
W.P. Mayles, S. Heisig and H. Mayles
Treatment verification and in vivo dosimetry
chapter 11 of Radiotherapy Physics in Practice (Williams, J.R., and
Thwaites, D.I., editors ) Oxford Univ.Press,second edition (2000)
[Meijer 2001]
G.J. Meijer, A.W. Minken, K.M. van Ingen, B. Smulders, H. Uiterwaal
and B.J. Mijnheer
Accurate in vivo dosimetry of a randomized trial of prostate cancer
irradiation.
Int. J. Radiation Oncology Biol. Phys. 49: 1409-1418 (2001)
[Meiler 1997]
R.J. Meiler and M.B. Podgorsak
Characterization of the response of commercial diode detectors used for
in vivo dosimetry
Med. Dosim. 22: 31-37 (1997)
[Mellenberg 1993] D.E. Mellenberg and S.L. Schoeppel
Total scalp treatment of mycosis fungoides: the 4x4 technique
170
Int. J. Radiation Oncology Biol. Phys. 27: 953-958 (1993)
[Mijnheer 1991]
B.J. Mijnheer, S. Heukelom, J.H. Lanson, L.J. van Battum, N.A.M. van
Bree and G. van Tienhoven
Should inhomogeneity corrections be applied during treatment planning
of tangential breast irradiation?
Radiother. Oncol. 22: 239-244 (1991)
[Mijnheer 1992]
B.J. Mijnheer
Quality assurance in radiotherapy: physical and technical aspects
Qual-Assur-Health-Care 4: 9-18 (1992)
[
Mijnheer 1994
]
B.J. Mijnheer
Possibilities and limitations of in vivo dosimetry
in “Radiation dose in radiotherapy from prescription to delivery”, IAEA
Report
TECDOC-734, edited by IAEA, 259-264 (1994).
[Millwater 1993] C.J. Millwater
The role of routine in vivo dosimetry as part of quality assurance in a
radiotherapy department: a feasibility study
M.Sc. thesis, University of Edinburgh (1993)
[Millwater 1998] C.J. Millwater, A.S. MaCleod and D.I. Thwaites
In vivo semiconductor dosimetry as part of routine quality assurance
Brit. J. Radiol. 71: 661-668 (1998)
[Mitine 1991]
C. Mitine, G. Leunens, J. Verstraete, N. Blanckaert, J. Van Dam, A.
Dutreix and E. van der Schueren
Is it necessary to repeat quality control procedures for head and neck
patients?
Radiother. Oncol. 21: 201-210 (1991)
[Muller 1990]
R. Muller-Runkel and U.P. Kalokhe
Scatter dose from tangential breast irradiation to the uninvolved breast

171
Radiology 175: 873-876 (1990)
[
Muller 1991
]
R. Muller-Runkel and S.S. Watkins
Introducing a computerized record and verify system: its impact on the
reduction of treatment errors
Med. Dosimetry 16: 19-22 (1991)
[NACP 1980]
Nordic Association of Clinical Physics (NACP)
Procedures in external radiation therapy dosimetry with electron and
photon beams with maximum energies between 1 and 50 MeV
Acta Radiol. Oncol. 19: 55-79 (1980)
[Nilsson 1985]
B. Nilsson
Electron contamination from different materials in high energy photon
beams
Phys. Med. Biol. 30: 139-151 (1985)
[Nilsson 1986]
B. Nilsson and A. Brahme
Electron contamination from photon beam collimators
Radiother. Oncol. 5: 235-244 (1986)
[Nilsson 1988]
B. Nilsson, B.I. Rudén and B. Sorcini
Characteristics of silicon diodes as patient dosemeters in external
radiation therapy
Radiother. Oncol. 11: 279-288 (1988)
[Niroomand 1991] A. Niroomand-Rad
Physical aspects of total body irradiation of bone marrow transplant
patients using 18 MV X rays
Int. J. Radiation Oncology Biol. Phys. 20: 605-611 (1991)
[
Noel 1987
]
A. Noel and P. Aletti
Les mesures in v ivo systématiques. A propos de 800 contrôles

172
J. Eur. Radiother. 8 (1987)
[
Noel 1992
]
A. Noel, P. Aletti, P. Bey, L. Malissard and I. Buccheit
L’erreur est humaine - Détection par dosimétrie in vivo.
Bull. Cancer/Radiother. 79: 307-334 (1992)
[Noel 1995]
A. Noel, P. Aletti, P. Bey and L. Malissard
Detection of errors in individual patients in radiotherapy by systematic
in vivo dosimetry
Radiother. Oncol. 34: 144-151 (1995)
[Ostwald 1995]
P.M. Ostwald, T. Kron, C.S. Hamilton and J.W. Denham
Clinical use of carbon-loaded thermoluminescent dosimeters for skin
dose determination
Int. J. Radiation Oncology Biol. Phys. 33: 943-950 (1995)
[Planskoy 1996a] B. Planskoy, A.M. Bedford, F.M. Davis, P.D. Tapper and L.T. Loverock
Physical aspects of total-body irradiation at the Middlesex Hospital
(UCL group of hospitals), London 1988-1993: I. Phantom measurements
and planning methods
Phys. Med. Biol. 41: 2307-2326 (1996)
[Planskoy 1996b] B. Planskoy, P.D. Tapper, A.M. Bedford and F.M. Davis
Physical aspects of total-body irradiation at the Middlesex Hospital
(UCL group of hospitals), London 1988-1993: II. In vivo planning and
dosimetry
Phys. Med. Biol. 41: 2327-2343 (1996)
[Podgorsak 1995] M.B. Podgorsak, J.P. Balog, C.H. Sibata and A.K. Ho

173
In vivo dosimetry using a diode detector system: regarding Lee et al.,
IJROBP 29: 1175-1182 (1994)
Int. J. Radiation Oncology Biol. Phys. 32: 556-557 (1995)
[Quast 1987]
U. Quast
Total body irradiation - review of treatment techniques in Europe
Radiother. Oncol. 9: 91-106 (1987)
[Quast 1990]
U. Quast, A. Dutreix and J.J. Broerse
Late effects of total body irradiation in correlation with physical
parameters
Radiother. Oncol. Suppl. 1: 158-162 (1990)
[Quast 1991]
U. Quast
The dose to lung in TBI
Strahlenther. Onkol. 167: 135-151 (1991)
[Redpath 1992]
A.T. Redpath, D.I. Thwaites, A. Rodger, M. Aitken and P.D. Hardman
A multidisciplinary approach to improving the quality of tangential
chest wall and breast irradiation for carcinoma of the breast
Radioth. Oncol. 23: 118-126. (1992)
[Ribas 1998]
M. Ribas, N. Jornet, T. Eudaldo, D. Carabante, M.A. Duch, M. Ginjaume,
G. Gómez de Segura and F. Sánchez-Dobaldo
Midplane dose determination during total boday irradiation using in
vivo dosimetry
Radiother. Oncol. 49: 91-98 (1998)
[Rikner 1983]
G. Rikner and E. Grusell
Effects of radiation damage on p -type silicon detectors
Phys. Med. Biol. 28: 1261-1267 (1983)
[Rikner 1984]
G. Rikner and E. Grusell
174
Radiation damage induced dose rate non-linearity in an n-type silicon
detector.
Acta Radiol. Oncol. 23: 465-469 (1984)
[Rikner 1987a]
G. Rikner and E. Grusell
General specifications for silicon semiconductors for use in radiation
dosimetry
Phys. Med. Biol. 32: 1109-1117 (1987)
[Rikner 1987b]
G. Rikner and E. Grusell
Patient dose measurements in photon fields by means of silicon
semiconductor diodes
Med. Phys. 14: 870-873 (1987)
[
Rikner 1993
]
G. Rikner
Silicon diodes as detectors in relative dosimetry of photon, electron and
proton irradiation fields
Doctoral thesis, Department of Physical Biology and Division of
Hospital Physics, Uppsala University, Sweden
[Rizzotti 1985]
A. Rizzotti, C. Compri and G.F. Garusi
Dose evaluation to patients irradiated by
60
Co beams, by means of direct
measurement on the incident and on the exit surfaces
Radiother. Oncol. 3: 279-283 (1985)
[Rudén 1976]
B.-I. Rudén
Evaluation of the clinical use of TLD
Acta Radiologica Therapy Physics Biology 15: 447-464 (1976)
[Sánchez 1994]
F. Sánchez-Doblado, R. Arráns, J.A. Terrón, B. Sánchez-Nieto and L.
Errazquin
Computerized semiconductor probe-based system for in vivo dosimetry
of patients undergoing high-energy radiotherapy
Med. Biol. Eng. Comput. 32: 588-592 (1994)

175
[Sánchez 1995]
F. Sánchez-Doblado, J.A. Terrón, B. Sánchez-Nieto, R. Arráns, L.
Errazquin, D. Biggs, C. Lee, L. Núnez, A. Delgado and J.L. Muniz
Verification of an on line in vivo semiconductor dosimetry system for
TBI with two TLD procedures
Radiother. Oncol. 34: 73-77 (1995)
[
Sen 1996
]
A. Sen, E.I. Parsai, S.W. McNeeley and K.M. Ayyangar
Quantitative assessment of beam perturbations caused by silicon diodes
used for in vivo dosimetry
Int. J. Radiat. Oncol. Biol. Phys. 36: 205-211 (1996)
[Shakeshaft 1999] J.T. Shakeshaft, H.M. Morgan and P.D. Simpson
In vivo dosimetry using diodes as a quality control tool: experience of 2
years and 2000 patients
Br. J. Radiol. 72: 891-895 (1999)
[Sixel 1994]
K.E. Sixel and E.B. Podgorsak
Build-up region of dose maximum of megavoltage X-ray beams
Med. Phys. 21: 411-416 (1994)
[Sjögren 1996]
R. Sjögren and M. Karlsson
Electron contamination in clinical high energy photon beams
Med. Phys. 23: 1873-1881 (1996)
[Sjögren 1998]
R. Sjögren and M. Karlsson
Influence of electron contamination on in vivo surface dosimetry for
high-energy photon beams
Med. Phys. 25: 916-921 (1998)
[Svahn 1976]
G. Svahn-Tapper
Mantle treatment: absorbed dose measurements in patients compared
with dose planning

176
Acta Radiologica Therapy Physics Biology 15: 340-356 (1976)
[Svarcer 1965]
V. Svarcer, J.F. Fowler and T.J. Deeley
Exit doses for lung fields measured by lithium fluoride
thermoluminescence
Brit. J. Radiol. 38: 785-790 (1965)
[Terrón 1994]
J.A. Terrón, F. Sánchez-Doblado, R. Arráns, B. Sánchez-Nieto and L.
Errazquin
Midline dose algorithm for in vivo dosimetry
Med. Dosim. 19: 263-267 (1994)
[Thwaites 1990]
D.I. Thwaites, G.L. Ritchie and A.C. Parker
Total body irradiation for bone marrow transplantation in Edinburgh:
techniques, dosimetry and results
Radioth. Oncol. 18 (suppl. 1): 143-145 (1990)
[Umek 1996]
B. Umek, M. Zwitter and H. Habic
Total body irradiation with translation method
Radiother. Oncol. 38: 253-255 (1996)
[Van Dam 1988]
J. Van Dam, A. Rijnders, L. Vanuytsel and H.-Z. Zhang
Practical implications of backscatter from outside the patient on the dose
distribution during total body irradiation
Radiother. Oncol. 13: 193-201 (1988)
[Van Dam 1990]
J. Van Dam, G. Leunens and A. Dutreix
Correlation between temperature and dose rate dependence of
semiconductor response; influence of accumulated dose
Radiother. Oncol. 19: 345-351 (1990)
[Van Dam 1992a] J. Van Dam, C. Vaerman, N. Blanckaert, G. Leunens, A. Dutreix and E.
van der Schueren

177
Are port films reliable for in vivo exit dose measurements?
Radiother. Oncol. 25: 67-72 (1992)
[Van Dam 1992b] J. Van Dam, G. Leunens, A. Dutreix and E. van der Schueren
Is equipment performance a factor of importance for the quality of
radiotherapy?
AMPI Medical Physics Bulletin 17: 26-30 (1992)
[
Van Dam 1994
]
J. Van Dam and G. Marinello
Methods for in vivo dosimetry in external radiotherapy
ESTRO Booklet Nr. 1, Garant (1994)
[van der Schueren]
E. van der Schueren, A. Dutreix and C. Weltens
In vivo dosimetry in clinical practice: When and What to measure? How
to correct?
ESTRO Booklet, to be published
[Van Dyk 1987]
J. Van Dyk
Dosimetry for total body irradiation
Radiother. Oncol. 9: 107-118 (1987)
[Van Dyk 1993]
J. Van Dyk, R.B. Barnett, J.E. Cygler and P.C. Shragge
Commissioning and quality assurance of treatment planning computers
Int. J. Radiation Oncology Bio l. Phys. 26: 261-273 (1993)
[Van Tienhoven 1997] G. van Tienhoven, B.J. Mijnheer, H. Bartelink and D.G. Gonzalez
Quality assurance of the EORTC Trial 22881/10882: boost versus no
boost in breast conserving therapy - an overview
Strahlenther. Onkol. 173: 201-207 (1997)
[Vanitsky 1993]
S. Vatnitsky and H. Järvinen
Application of a natural diamond detector for the measurement of
relative dose distributions in radiotherapy
Phys. Med. Biol. 38: 173-184 (1993)

178
[Van Gasteren 1991] J.J.M. Van Gasteren, S. Heuke lom, H.J. Van Kleffens, R. van der
Laarse, J.L.M. Venselaar and C.F. Westermann
The determination of phantom and collimator scatter components of the
output of mega-voltage photon beams: measurement of the collimator
scatter part with a beam-coaxial narrow cylindrical phantom
Radiother. Oncol. 20: 250-257 (1991)
[
Voordeckers 1998
]
M. Voordeckers, H. Goossens, J. Rutten and W. Van den Bogaert
The implementation of in vivo dosimetry in a small radiotherapy
department
Radiother. Oncol. 47: 45-48 (1998)
[Vrtar 1998]
M. Vrtar and N. Kovacevic
A model of in vivo dosimetry and quality assurance analysis of total
body irradiation in Zagreb
Acta Medica Croat. 52: 15-26, 1998
[Wall 1982]
B.F. Wall, C.M.H. Driscoll, J.C. Strong and E.S. Fischer
The suitability of different preparations of thermoluminescent lithium
borate for medical dosimetry
Phys. Med. Biol. 27: 1023-1034 (1982)
[Wambersie 1969] A. Wambersie, J. Dutreix and A. Dutreix
Précision dosimétrique requise en radiothérapie - consequences
concernant le choix et les performances exigées des détecteurs
Journal Belge de Radiologie 52: 94-104 (1969)
[Weaver 1995]
R.D. Weaver, B.J. Gerbi and K.E. Dusenbery
Evaluation of dose variation during total skin electron irradiation using
thermoluminescent dosime ters

179
Int. J. Radiation Oncology Biol. Phys. 33: 475-478 (1995)
[Weltens 1993]
C. Weltens, G. Leunens, A. Dutreix, J.M. Cosset, F. Eschwege and E. van
der Schueren
Accuracy in mantle field irradiations: irradiated volume and daily dose
Radiother. Oncol. 29: 18-26 (1993)
[Weltens 1994]
C. Weltens, J. Van Dam, G. Leunens, A. Dutreix and E. van der Schueren
Reliability of clinical port films for measuring dose inhomogeneities in
radiotherapy for head and neck tumours
Radiother. Oncol. 30: 167-170 (1994)
[Weltens 1998]
C. Weltens, D. Huyskens, A. Dutreix and E. van der Schueren
Assessment of dose inhomogeneities in clinical practice by film
dosimetry.
Radiother. Oncol. 49: 287-294, 1998.
[
Wierzbicki 1998
]
J.G. Wierzbicki and D.S. Waid
Large discrepancies between calculated D
max
and diode readings for
small field sizes and small SSDs of 15 MV photon beams
Med. Phys. 25: 245-246 (1998)
[
Wilkins 1997
]
D. Wilkins, X. Allen Li, J. Cygler and L. Gerig
The effect of dose rate dependence of p-type silicon detecors on linac
relative dosimetry
Med. Phys. 24: 879-881 (1997)
[WHO 1988]
WHO
Quality Assurance in Radiotherapy
Geneva (1988)
[Wolff 1998]
T. Wolff, S. Carter, K.A. Langmack, N.I. Twyman and P.P. Dendy
Characterization and use of a commercial n -type diode system
Br. J. Radiol. 7: 1168-1177 (1998)
[Zhu 1998]
T.C Zhu and J.R. Palta

180
Electron contamination in 8 and 18 MV photon beams
Med. Phys. 25: 12-19 (1998)

Entrance in vivo dosimetry with diode detectors has been demonstrated to be a valuable
technique among the standard quality assurance methods used in a radiotherapy department.
Although its usefulness seems to be generally recognized, the additional worklo ad generated
by in vivo dosimetry is one of the factors that impedes a widespread implementation.
Especially during the initial period of establishing the technique in clinical routine, the
responsible QA person is confronted with variable tasks, such as purchasing equipment,
calibrating, defining measurement and interpretation procedures. Often, this is accompanied
by the time-consuming activities of searching through literature and contacting experienced
departments in order to gather information and define the sequence of the steps to be
undertaken.
This booklet is set up as a tool to reduce these initial efforts: it is conceived as a step -by-step
guide to implement entrance in vivo dosimetry with diodes in the clinical routine of a
radiotherapy department.
The first chapter about the preparation of the measurements contains information (including
commercial specifications) on diodes, electrometers and software. Practical guidelines for the
calibration of the diodes and the determination of correction factors are given.
The second chapter discusses the actual tasks of the responsible QA person during the initial
training period, with the emphasis on the implementation of the measurement procedure (e.g.
the training of personnel with explanation of immediate actions to be undertaken in case of
out-of-tolerance measurements)
In the third chapter, the interpretation of the measurement in relation to tolerance and action
levels is discussed and possible origins and consequences of out -of-tolerance measurements
are given.
In an additional chapter, we present an overview resulting from the evaluation of a
questionnaire on how in vivo dosimetry has been implemented in different international
centres. In the final chapter, elaborate contributions are given from five centres about
particular topics in in vivo dosimetry.
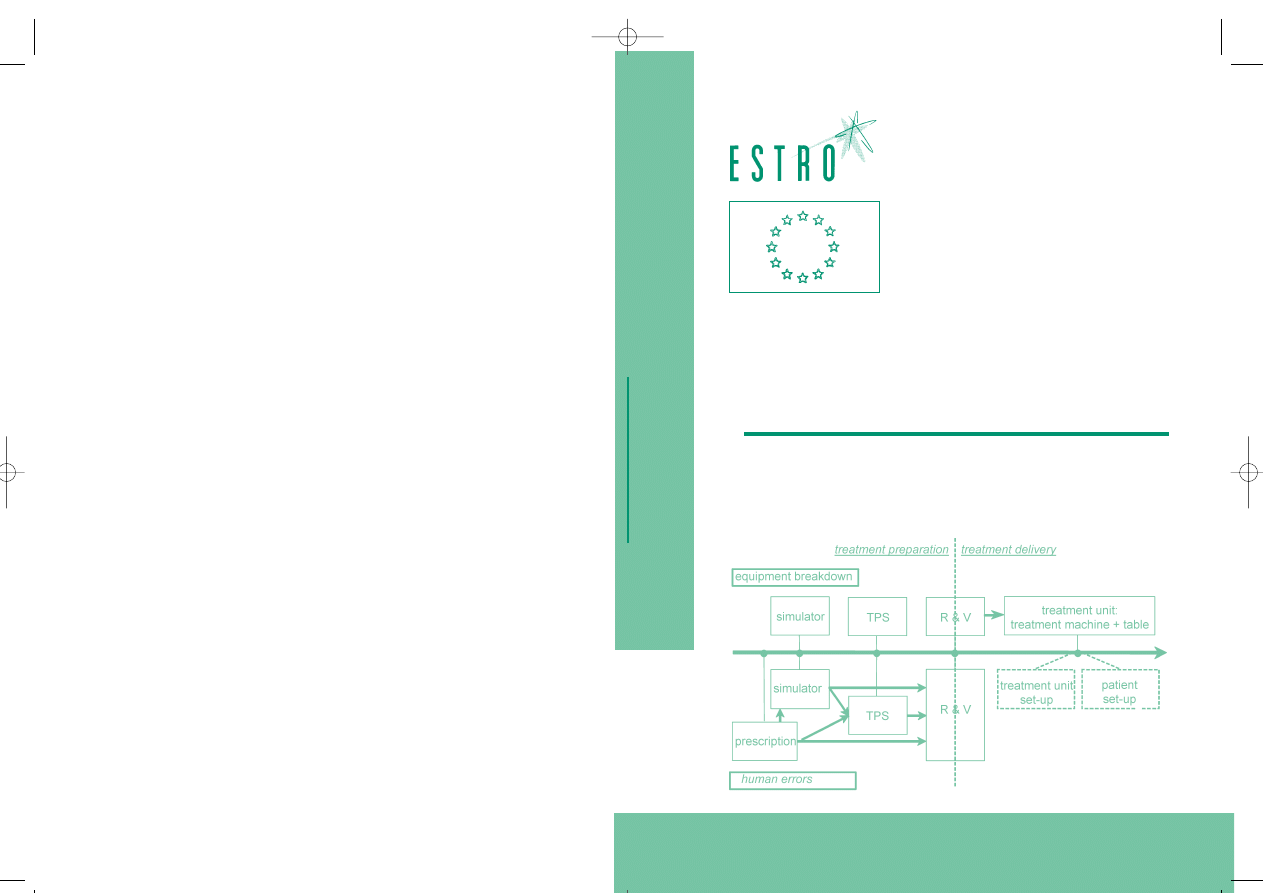
EUROPEAN SOCIETY FOR THERAPEUTIC RADIOL
OG
Y AND ONCOL
OG
Y
D
OMINIQUE
H
UYSKENS
R
IA
B
OGAERTS
J
AN
V
ERSTRAETE
M
ARIKA
L
ÖÖF
H
ÅKAN
N
YSTRÖM
C
LAUDIO
F
IORINO
S
ARA
B
ROGGI
N
ÚRIA
J
ORNET
M
ONTSERRAT
R
IBAS
D
AVID
I. T
HWAITES
Sponsored by
“Europe Against Cancer”
P
RACTICAL
G
UIDELINES
F
OR
T
HE
I
MPLEMENTATION
O
F
I
N
V
IVO
D
OSIMETRY
W
ITH
D
IODES
I
N
E
XTERNAL
R
ADIOTHERAPY
W
ITH
P
HOTON
B
EAMS
(E
NTRANCE
D
OSE
)
PHYSICS FOR CLINICAL RADIOTHERAPY
BOOKLET No. 5
Entrance in vivo dosimetry with diode detectors has been demonstrated to be a
valuable technique among the standard quality assurance methods used in a radio-
therapy department. Although its usefulness seems to be generally recognised, the
additional workload generated by in vivo dosimetry is one of the factors that
impedes a widespread implementation. Especially during the initial period of es-
tablishing the technique in clinical routine, the responsible QA person is con-
fronted with variable tasks, such as purchasing equipment, calibrating, defining
measurement and interpretation procedures. Often, this is accompanied by the
time-consuming activities of searching through literature and contacting expe-
rienced departments in order to gather information and define the sequence of the
steps to be undertaken.
This booklet is set up as a tool to reduce these initial efforts: it is conceived as a
step-by-step guide to implement entrance in vivo dosimetry with diodes in the
clinical routine of a radiotherapy department.
The first chapter about the preparation of the measurements contains information
(including commercial specifications) on diodes, electrometers and software.
Practical guidelines for the calibration of the diodes and the determination of cor-
rection factors are given.
The second chapter discusses the actual tasks of the responsible QA person dur-
ing the initial training period, with the emphasis on the implementation of the
measurement procedure (e.g. the training of personnel with explanation of imme-
diate actions to be undertaken in case of out-of-tolerance measurements)
In the third chapter, the interpretation of the measurement in relation to tolerance
and action levels is discussed and possible origins and consequences of out-of-tol-
erance measurements are given.
In an additional chapter, we present an overview resulting from the evaluation of
a questionnaire on how in vivo dosimetry has been implemented in different inter-
national centres. In the final chapter, elaborate contributions are given from five
centres about particular topics in in vivo dosimetry.
ISBN 90-804532-3
P
RACTICAL
G
UIDELINES
F
OR
T
HE
I
MPLEMENT
A
TION
O
F
I
N
V
IVO
D
OSIMETRY
W
ITH
D
IODES
I
N
E
XTERNAL
R
ADIOTHERAP
Y
W
ITH
P
HOTON
B
EAMS
(E
NTRANCE
D
OSE
)
TW KAFT BOOKLET 5 11-09-2001 11:46 Pagina 1
Wyszukiwarka
Podobne podstrony:
APA practice guideline for the treatment of patients with Borderline Personality Disorder
Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage
GUIDELINES FOR THE APPROVAL OF FIXED WATER BASED LOCAL APPLICATION
guidelines for the content of rig move procedures sept 2008
The American Society for the Prevention of Cruelty
[Pargament & Mahoney] Sacred matters Sanctification as a vital topic for the psychology of religion
International Convention for the Safety of Life at Sea
Microsoft Word MIC1 Guidelines for the Generat
Broad; Arguments for the Existence of God(1)
ESL Seminars Preparation Guide For The Test of Spoken Engl
Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syn
GB1008594A process for the production of amines tryptophan tryptamine
Popper Two Autonomous Axiom Systems for the Calculus of Probabilities
Anatomical evidence for the antiquity of human footwear use
The Reasons for the?ll of SocialismCommunism in Russia
więcej podobnych podstron