Simposium Sains Kesihatan Kebangsaan ke 7
Hotel Legend, Kuala Lumpur, 18 – 19 Jun 2008 : 202 – 204
Chronic pain and psychological well-being
Farezadi, Z.
1
, *Normah, C. D.
1
, Zubaidah, J.
2
& Maria, C.
3
1
Health Psychology Unit, Faculty of Allied Health Sciences, Universiti Kebangsaan Malaysia,
Jalan Raja Muda Abdul Aziz, 50300 Kuala Lumpur, Malaysia
2
Department of Psychiatry, Faculty of Medicine, Universiti Putra Malaysia,
Serdang, Selangor Darul Ehsan
3
Department of Anaesthesiology, Hospital Selayang, Selangor Darul Ehsan
*Corresponding author: Tel: +603-92897048; Fax: +603-26911052; Email address: normah@medic.ukm.my
Chronic pain and psychological distress have been found to
frequently co-occur. The aim of this study is to evaluate the
relationship between pain intensity, physical disability, self-
efficacy, active coping, catastrophizing and psychological
distress (stress/tension, anxiety, and depressive symptoms.
Data were collected from 88 chronic pain patients who were
referred to the pain clinic in Selayang Hospital. The data
collected include sociodemographic data, pain intensity using
the Numeric Rating Scale (NRS), physical disability by using
the Physical Disability Questionnaire (PDQ), psychological
distress assessed by the Depression Anxiety Stress Scale
(DASS-42), pain self-efficacy assessed by the Pain Self-
Efficacy Questionnaire (PSEQ) and catastrophizing thoughts
by using the Pain Responses Self-Statement (PRSS).Self-
efficacy showed negative correlation with both physical and
psychological variables while catastrophizing have positive
correlation with physical and psychological aspect of pain.
Active coping have negative correlation with physical profiles
but showed positive association with psychological aspects of
pain. This study provides information about variables and
factors associated with psychological well-being of chronic
pain sufferers and provide implications on the aspects of
treatment modalities in managing chronic pain patients.
Introduction
Pain, particularly chronic pain, is one of the most common threat
to the quality of life (QOL) worldwide and will become more so
as the age increases. The burden of unrelieved pain is also a major
problem for health services throughout the world.
Pain is a widespread human experience. The International
Association for the Study of Pain defined pain as “an unpleasant
sensory and emotional experience associated with actual or
potential tissue damage, or described in terms of such
damage“(Merskey, 1986). Current understanding and concepts of
pain are based on the developments from the Gate Control Theory
of Pain suggested by Melzack and Wall (1965). The internal
biopsychosocial variables that may influence the pain responses
include the autonomic, immune, stress regulation, and
endogenous opioid system. The psychological variables that may
influence the pain responses include cultural factors, past
experiences, personality, attention, motivational and cognitive
factors (Melzack, 1999a).
Chronic pain does not have any clear biological function and
is usually associated with negative impact on the physical,
psychological and social well-being of the individual (Stembach,
1989). Bonica (1990) defined chronic pain as “pain that persists
beyond the usual course of an acute disease; or persists more than
a reasonable time for an injury to heal or is associated with a
chronic pathological process that causes continuous pain; and
recurs at intervals for months or years”. Its origin, duration,
intensity, and specific symptoms vary. In terms of duration,
chronic pain has been defined as pain lasting longer that three or
six months (Merskey & Bogduk, 1994).
Pain that is not controlled can generate serious physical,
psychological and social effects and can have a disruptive impact
on a person’s daily life. The physical effects may include
progressive physical deterioration such as general fatigue and
debility caused by disturbance of sleep, appetite, decreased
physical activity, side effects from excessive medication (Von
Korff & Simon, 1996).
Most patients with chronic pain experience emotional
distress to a varying degree. The emotional impacts of chronic
pain include reactive depression, hopelessness, despair and
dependency, loss of sleep, loss of self-worth, loss of mobility,
anxiety over the pain itself and also how the patient is perceived
by their family and peers, loss of employment, anger directed
outward in generalized manner, and in some cases, suicide. A
variety of factors such as the nature and prognosis of the
condition, coping abilities, social support, attitudes and behaviors
of health professionals and patient’s beliefs can contribute to the
extent of emotional distress (Skevington, 1995). Other factors
include locus of control, stress level, self-efficacy and negative
thoughts. Active coping strategies were related to reduce pain
severity, lower levels of depression and less functional
impairment while the reverse applied to passive coping strategies
(Nicholas, 1987). Negative thinking such as catastrophizing has
always been found to be significantly related to heightened pain
severity in a variety of chronic pain conditions and related to
lower pain thresholds and pain tolerance levels in normals
(Sullivan et al, 2001). Self-efficacy refers to the ability to cope
effectively or exert control over pain. Self-efficacy was found to
have significant inverse correlation with pain intensity and
interference with life (Lin, 1998).
The aim of this study is to evaluate the relationships between
pain intensity, physical disability, self-efficacy, active coping,
catastrophizing and psychological distress (stress/tension, anxiety,
and depressive symptoms.
Methods
Participants
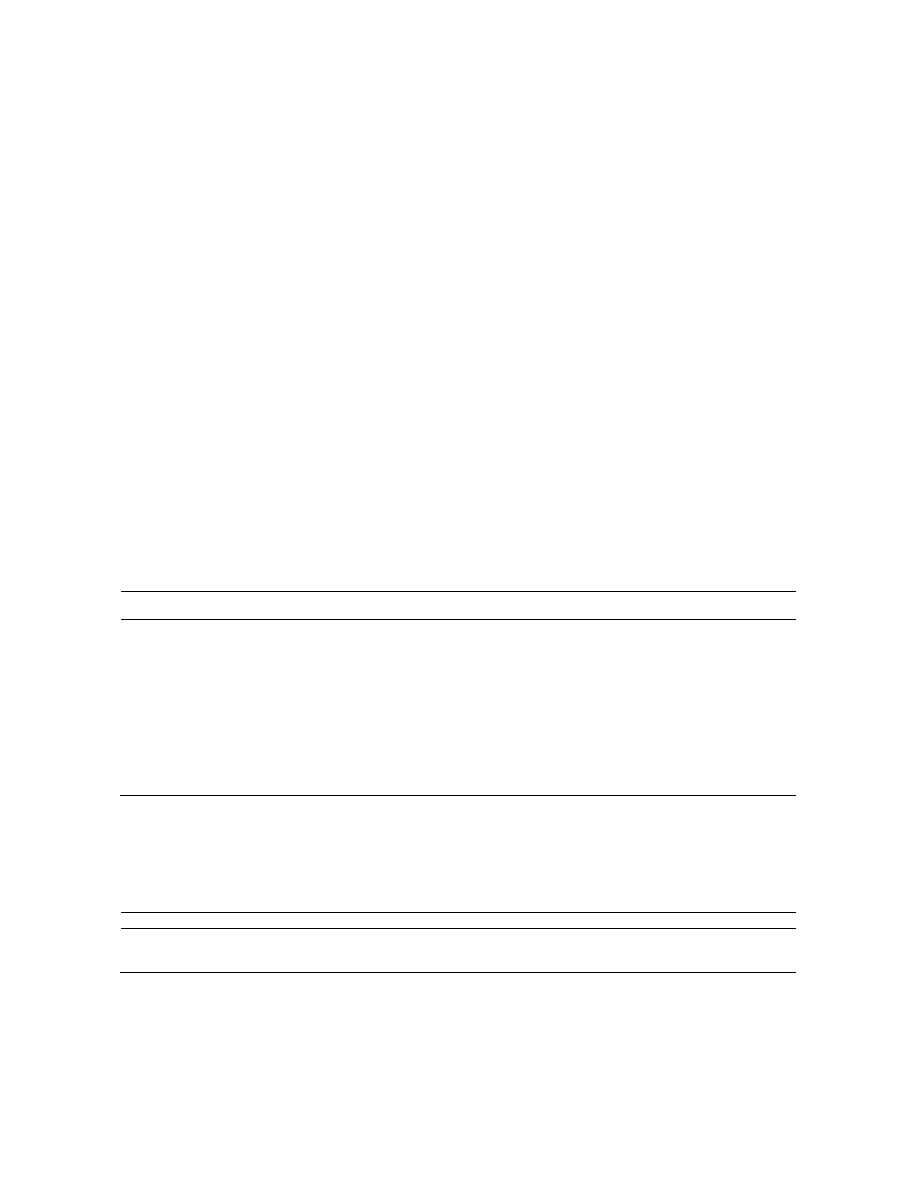
Participants were 88 chronic pain patients recruited from
Selayang Hospital, Selangor. of the 88 patients, 54.5% were
females and 45.5% were males, The average age was 48 ± 12
years old. The majority of patients were married (64.8%),
working (67%) and aged above 41 years old (77.3%). In terms of
ethnicity, 39.8% were Malay, 18.2% Chinese, and 6.8% were
other races (Table 1).
Research Design
Sihat2008
ISBN 978-983-43150-9-2
Farezadi, Z. et al./Sihat2008 : 202 – 204
203
This is a retrospective study. Pain profiles were gathered from the
Pain Management Clinic, Selayang Hospital, Selangor from 2004
to 2007.
Measures
The data collected include the sociodemographic data, pain
intensity using the Numeric Rating Scale (NRS), physical
disability by using the Physical Disability Questionnaire
(PDQ)(Roland & Morris, 1983), psychological distress assessed
by the Depression Anxiety Stress Scale (DASS-42)(Lovibond &
Lovibond, 1995), pain self-efficacy assessed by the Pain Self-
Efficacy
Questionnaire
(PSEQ)(Nicholas,
1989)
and
catastrophizing thoughts by using the Pain Responses Self-
Statement (PRSS).
Result
Self-efficacy in general has significant negative correlation with
pain intensity (r = -.219, p < .05), physical disability (r = -.366, p
< .01), stress (r = -.279, p < .01), anxiety (r = -.251, p < .05), and
depression (r = -.380, p < .01)(Table 2). Catastrophizing in
general has significant positive correlation with pain intensity (r =
.416, p < .01), stress (r = .564, p < .01), anxiety (r = .485, p < .01),
and depression (r = .633, p < .01). Active coping in general has no
significant correlation with pain intensity, physical disability,
stress, anxiety and depression.
Discussion
Self-efficacy in general has significant negative correlation with
pain intensity, physical disability, stress, anxiety and depression.
This means that high self-efficacy reduced the pain instensity,
physical disability, stress, anxiety and depression. This result is
consistent with previous findings by other researchers (Arnstein et
al., 1999; Lynch et al., 1996; Sharloo & Kaptein, 1997).
Catastrophizing in general was found to have positive correlation
with pain intensity, stress, anxiety and depression but not with
physical disability. This means that high catastrophizing will
make the pain intensity and physical disability worse and increase
the level of stress, anxiety and depression. The result is supported
by previous research (Severeijns et al., 2001; Sullivan et al., 2001;
Turner et al., 2001).
Active coping in general has no significant correlation with pain
intensity, physical disability, stress, anxiety and depression. This
result was not supported by other research (Gatchel & Turk,
1999). The nonsignificant relationships can be related to the
coping strategies used which in any given situation are dependent
upon contextual factors and the individual’s appraisal of these. A
passive strategy in one instance may be in fact be adaptive in
another. Second, those with chronic conditions were more likely
to use a combination of various and varied coping responses to
manage their condition and adjust their life accordingly.
TABLE 1 Sociodemographic Data of Chronic Pain Patients
Variables
Frequency
Percent
Age
< 40 years old
20
22.7
> 41 years old
68
77.3
Gender
Male
40
45.5
Female
48
54.5
Ethnicity
Malay
35
39.8
Chinese
16
18.2
Others
6
6.8
Marital Status
Single
20
22.7
Married
57
64.8
Divorced/Widowed
11
12.5
Job Status
Working
59
67
Not Working
29
33
TABLE 2 Pearson Correlation between Self-Efficacy, Catastrophizing, and Active Coping with
Pain Intensity, Physical Disability, Stress, Anxiety and Depression
Pain Intensity
Physical Disability
Stress
Anxiety
Depression
Self-Efficacy
-.219*
-.366**
-.279**
-.251*
-.380**
Catastrophizing
.416**
.185
.564**
.485**
.633**
Active Coping
-.016
-.081
.034
.047
-.011
* p < .05, ** p < .01

Farezadi, Z. et al./Sihat2008 : 202 – 204
204
Conclusion
Chronic pain was found to be associated with psychological well-
being and psychological distress chronic patients. However, this
association was explained by other features, which are known to
be associated with such pain. Chronic pain itself does not
necessarily predict psychological distress, rather, other mediating
factors such as self-efficacy, catastrophizing and coping strategies
might play important role in affecting psychological well-being of
chronic pain patients. The findings support the argument that it is
the interaction between chronic pain, physical, and psychological
factors that influence patients’ psychological well-being.
Therefore, factors such as self-efficacy and catastrophizing should
not be overlooked in the treatment of patients with chronic pain.
Any treatment modalities utilized in treating chronic pain patients
should not only focus on the physical aspects of the patients, but
social and psychological aspects as well. Health practitioners
handling chronic pain patients need to evaluate patients’
psychological aspects so that treatment can be provided
effectively, for example, conducting treatments with the aims of
maximizing self-efficacy and minimizing catastrophizing.
Consequently, this may help chronic patients to improve their
psychological well-being.
References
Arnstein, P., Caudill, M., Mandle, C., Norris, A., & Beasley, R.
Self-efficacy as a mediator of the relationship between pain
intensity, disability and depression in chronic pain patients.
Pain 80: 483-491.
Bonica, J.J. 1990. Definition and taxonomy of pain. In: Bonica,
J.J. Ed. The Management of Pain, pp. 18-27. Pennsylvania:
Lea and Febiger.
Gatchek, R.J., & Turk, D.C. 1999. Psychosocial Factors in Pain:
Critical Perspectives. New York: The Guilford Press.
Lovibond, S.H., & Lovibond, P.F. 1995. Manual for the
Depression Anxiety Stress Scales. Australia: The
Psychological Foundation of New South Wales Inc.
Lynch, R.T., Agre, J., Powers, J.M., & Sherman, J. 1996. Long-
term follow up of outpatient interdisciplinary pain
management with a no-treatment comparison group.
American Journal of Physical Medical Rehabilitation 75:
213-222.
Melzack, R. 1999a. From the gate to the neuromatrix. Pain 6:
S121-126.
Melzack, R., & Wall, P.D. 1965. Pain mechanisms: A new theory.
Science 150: 971-979.
Merskey, H., & Bogduk, N. 1994. Classification of Pain,
Description of Chronic Pain Syndromes and Definition of
Pain Terms. Seattle: IASP Press.
Merskey, H. 1986. Internal Association for the Study of Pain:
Classification of chronic pain. Pain 3: S217.
Nicholas, M.K. 1989. Self-efficacy and chronic pain. Paper
presented at the annual conference of the British
Psychological Society, St. Andrews.
Roland, M., & Morris, R. 1983. A study of natural history of back
pain, part I: Development of a reliable and sensitive measure
of disability in low back of pain. Spine 8: 141-144.
Severeijns, R., Vlaeyen, J.W., van den Hout, M.A., & Weber,
W.E. 2001. Pain catastrophizing predicts pain intensity,
disability, and psychological distress independent of the level
of physical impairment. Clinical Journal of Pain 17: 165-
172.
Skevington, S. 1995. Psychology of Pain. Chichester: John Wiley
& Sons.
Stembach, R.A. 1989. Acute versus chronic pain. In: Wall, P.D. &
Melzack, R. Eds. Textbook of Pain, pp. 242-246. Edinburgh:
Churchill Livingstone.
Sullivan, M.J., Thiorn, B., Haythornthwaite, J.A., Keefe, F.,
Martin, M., Bradley, L.A., & Lefebvre, J.C. 2001. Clinical
Journal of Pain 17: 52-64.
Turner, J.A., Dworkin, S.F., Mancl, L., Huggins, K.H., &
Truelove, E.L. 2001. The role of beliefs, catastrophizing and
coping
in
the
functioning
of
patients
with
temporomandibular disorders. Pain 92: 41-51.
Von Korff, M., & Simon, G. 1996. The relationship between pain
and depression. British Journal of Psychiatry 30: 101-108.
Wyszukiwarka
Podobne podstrony:
[Rathi & Rastogi] Meaning in life & psychological well being in pre adolescents & adolescents
Caplan (2003) Preference for online social interaction A theory of problematic Internet use ans psy
04 Emotions and well being across cultures
25 Natural Ways to Relieve Headaches A Mind Body Approach to Health and Well Being by Romy Fox
The Effects of Performance Monitoring on Emotional Labor and Well Being in Call Centers
Work motivation, organisational identification, and well being in call centre work
Working conditions, well being, and job related attitudes among call centre agents
Chronic Pain Syndromes After Ischemic Stroke PRoFESS Trial
Chronic Pain for Dummies
Moberg Spiritual Well Being Questionnaire
Neurobiology and Psychotherapy 12
22 The climate of Polish Lands as viewed by chroniclers, writers and scientists
Baudrillard, Critical Theory And Psychoanalysis
Methapor and Psychoterapy
Chronic Pain Syndromes After Ischemic Stroke PRoFESS Trial
Toward a Psychology of Being Abraham Maslow
Baudrillard, Jean Critical Theory And Psychoanalysis
więcej podobnych podstron